The Impact of Whole Brain Radiation Therapy on Parotid Gland
Savitha D1, Pradeep KN1*, Sunil RA2 and Lokesh V3
1Senior resident, Dept of Radiation Oncology, Kidwai Memorial Institute of Oncology, India
2Assistant Professor, Dept of Radiation oncology Kidwai Memorial Institute of Oncology, India
3Prof and Head Dept of Radiation oncology, Kidwai Memorial Institute of Oncology, India
Submission: May 21, 2020; Published:September 09, 2020
*Corresponding Address:Pradeep KN, Senior resident, Department of Radiation Oncology Kidwai Memorial Institute of Oncology, Bangalore, India
How to cite this article:Savitha D, Pradeep K, Sunil RA, Lokesh V. The Impact of Whole Brain Radiation Therapy on Parotid Gland. Canc Therapy & Oncol Int J. 2020; 16(5): 555950.DOI:10.19080/CTOIJ.2020.16.555950
Abstract
Background and purpose of study: Whole brain radiation therapy (WBRT) has been the treatment of choice for the brain metastasis, irrespective of primary site of malignancy. Many times, parotid glands are not delineated as organs at risk, hence the dose to the parotid glands are not reported during planning of WBRT. Hence in this study we intent to see the dose received by the parotid glands during WBRT.
Materials and Methods: This is a prospective study. Totally 63 patients who had received whole brain radiation therapy from January 2018 to December 2019 at a quaternary Oncology centre were accrued. Patients planned for WBRT with brain metastases from solid organ malignancy and for haematological malignancies were included. Patients planned for brain metastases and PCI received a dose of 30Gy and leukaemia patients a dose of 18Gy in 10 fractions, to the whole brain. Prospectively bilateral parotid glands were delineated.
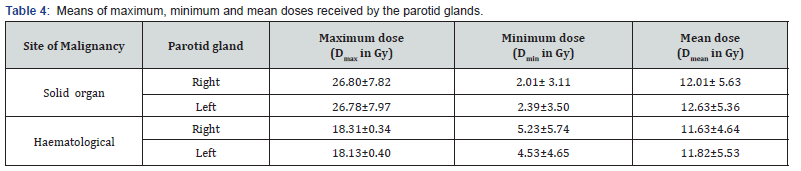
Results: 28 (44%) of the patients received palliative WBRT due to brain metastases due to malignancy arising from solid organs, 35 (56%) of the patients received WBRT due to haematological malignancy. The means of mean doses to right and left parotid glands were 12.01± 5.62Gy and 12.63±5.36Gy respectively in those with solid organ malignancies and similarly in those with haematological malignancies were11.63±4.64Gy and11.82±5.53Gy to right and left parotid gland respectively.
Conclusion: Even in patients planned for WBRT delineating the parotid glands is to be done irrespective of treatment intention, so that the mean dose to the parotid glands could be decreased.
Introduction
Whole brain radiation therapy (WBRT) has been the treatment of choice for the brain metastasis, irrespective of primary site of malignancy. With the advent of newer chemotherapeutic agents to control the systemic disease and early diagnosis of the metastatic disease in brain has led to improvement in the overall survival and longer median survival of 7-10 months of the patients with brain metastases and also improved the quality of life [1,2]. Whole brain radiation therapy has been given in the patients with leukaemia’s, lymphomas and prophylactically in small-cell lung cancer [3]. WBRT delivers significant dose to the parotid glands [4]. Many times, parotid glands are not delineated as organs at risk and avoidance of the radiation therapy are not done. Hence dose to the parotid glands are not reported during WBRT. It is well established that minimizing the dose to the parotid glands during radiation therapy in head and neck cancer patients decreased the risk of xerostomia [5]. Hence in this study we intent to estimate the dose received by the parotid glands during whole brain RT and discuss the risk of these patients developing xerostomia.
Materials and Methods
This is a prospective study conducted among 63 patients who had received whole brain radiation therapy from January 2018 to December 2019 at a quaternary Oncology centre. Patients with brain metastases from solid organ malignancy irrespective of the primary site of origin, histology of the primary disease, number of metastatic lesions in the brain and among patients receiving therapeutic, prophylactic and palliative WBRT for haematological malignancies like leukaemia and lymphoma were included for the study. Patients who received WBRT as prophylactic cranial irradiation (PCI) in small cell lung cancers were also included. Patients who received WBRT for primary brain malignancy, cranio-spinal irradiation and those who were treated with parallel opposed open portal radiation therapy were excluded from the study. In brain metastases the dose of 30Gy in 10fractions, with 3Gy per fraction were given over a period of 2 weeks. In leukaemia, the patients received a dose of 18Gy in 10 fractions, with 1.8Gy per fraction over period of 2 weeks to the whole brain. The patients planned for PCI received a 30Gy in 10fractions, with 3Gy per fraction were given over a period of 2weeks. According to institutional protocol, clinical treatment volume (CTV) of all the patients consisted entire brain parenchyma along with meninges, excluding optic nerves were included from vertex to C1 vertebra. 0.5 cm margin was given all around CTV to create planning target volume (PTV). Once the patients who met with above mentioned criteria were selected, prospectively bilateral parotid glands were delineated by a single radiation oncologist to minimise the subjective bias. The maximum dose (D max), minimum dose (D min), mean dose (D mean) for each parotid gland was noted. Also, volumetric parameters like percentage volume of the parotid gland receiving 5Gy (V5), 10Gy (V10), 15Gy (V15), 20Gy (V20), 25Gy (V25) for each parotid gland were tabulated.
Statistical Analysis
All the data was entered in Microsoft 2010 excel sheet. Continuous data viz., age, volume of parotid glands percentage volume of parotid glands receiving the radiation dose, maximum (Dmax), minimum (Dmin) and mean doses received by the parotids were expressed in means and standard deviations. The categorical data viz., gender and primary site of origin were expressed in proportions and percentages.
Results
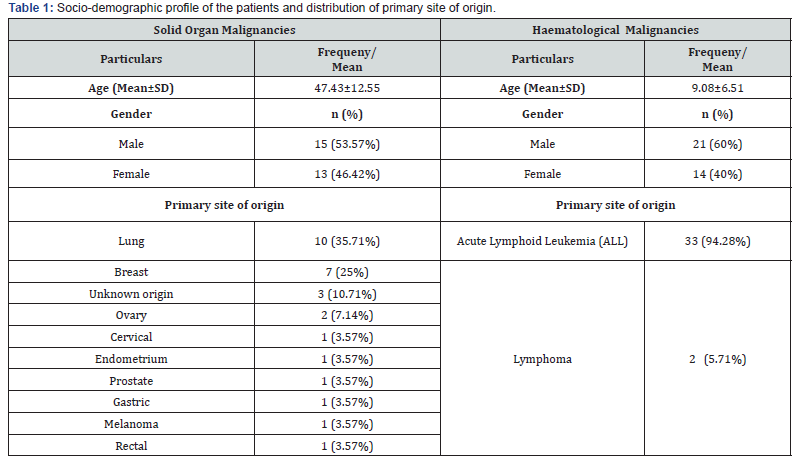
Out of 63 patients selected, 28 (44%) of the patients received palliative WBRT due to brain metastases of malignancy arising from solid organs, 35 (56%) of the patients received WBRT due to haematological malignancy. The mean age of patients with brain metastases due to solid organ malignancy was 47.43±12.55 years and haematological malignancy was 9.08±6.51 years. Among the solid organ malignancy, lung cancer 10 (35.7%), followed by breast cancer patients 7 (25%) made most of the patients and rest malignancy as described in the table 1. Majority i.e., 33 (52.4%) received WBRT as prophylactic radiation therapy due to Acute lymphoid leukaemia (ALL) (Table 1).
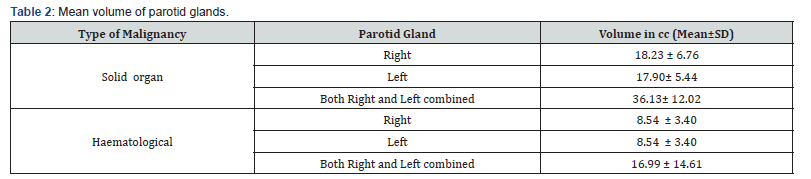
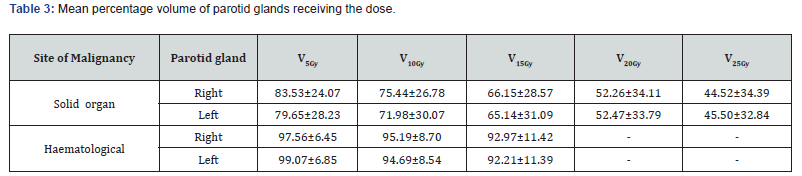
The mean volumes of right parotid gland was slightly more (18.23 ± 6.76 cc) compared to left parotid gland (17.90± 5.44 cc) in those with solid organ malignancies and it was same for both in those with Haematological malignancies i.e., 8.54 ± 3.40cc (Table 2). The mean percentage volumes receiving the dose of 5, 10, 15, 20 and 25 in Gy showed progressive decrease in both the parotid glands among solid organ and similarly the dose of 5, 10 and 15 Gy in haematological malignancies (Table 3). Among those with solid organ malignancies, the means of maximum doses to right and left parotid glands were 26.80±7.82Gy and 26.78±7.97Gy respectively and means of mean dose were 12.01± 5.62Gy and 12.63±5.36Gy respectively. Similarly, among those with haematological malignancies means of maximum doses and mean doses were 18.31±0.34Gy and 11.63±4.64Gy to right parotid gland and 18.13±0.40Gy and 11.82±5.53Gy to left parotid gland respectively (Table 4).
Discussion
The incidence of brain metastasis is hypothesized to have increased during the last 20 years partly due to increased usage of MRI in detection of lesions and a global increase in incidence and diagnosis of cancer [1]. According to Deasy JO et al. [6,7] and Quantitative Analyses of Normal Tissue Effects in the Clinic (QUANTEC) group the severe xerostomia can be avoided, if at least one parotid gland receives a mean dose lesser than 20 Gy or both parotid glands receives a mean dose less than 25 Gy. Though the guidelines say so, in other literatures, significant loss of salivary secretion has been noted at even low mean dose of even 10 Gy [8]. Chao et al. [9] showed an exponential reduction of approximately 4% in salivary flow for each Gray of mean parotid dose impacting the quality of life of patients surviving for longer duration post radiation therapy [9] Noh OK et al., predicted rates of Normal tissue complication probabilities (NTCP) for the parotid gland-xerostomia, ranged from 9%-19% vs. 6%-12%, for the mean parotid dose of 15.3 Gy vs. 11.9 Gy [4]. Hence in our study the mean dose of the parotid glands being 12Gy and 11Gy in both solid organ and haematological malignancies, chances of developing parotid gland dysfunction cannot be ruled out. In paediatric patients ranging from 3-18 years in our study, the mean doses received by right and left parotids were 11.90±4.37 Gy and 11.57±5.40 Gy respectively which is also more compared to above mentioned literature.8 Moreover, the volume of right and left parotid glands among the paediatric patients with haematological malignancies between 3-18 years were 8.12±2.94 cc and 7.91±3.19 cc which are comparatively smaller compared to that of those of higher age group with solid organ malignancies. The means of percentage volume of the gland receiving dose V5Gy, V10Gy, V15Gy were also more in paediatric patients with haematological malignancies between 3-18 years were 97.31±6.56, 94.83±8.83 and 92.96±10.74 for right parotid and 96.83±6.99, 94.38±8.71 and 91.83±11.62 for left parotid respectively and are relatively more compared to that of those of higher age group with solid organ malignancies. Hence expecting higher survival of paediatric patients with haematological malignancies, development of xerostomia in latter part of life will be tragic [10]. Due to limited availability of studies conducted in patients receiving WBRT of paediatric age group, we were not able to quantify the damage induced by the radiation therapy in those growing age group.
Conclusion
Compared to the existing literatures, we would conclude that delineation of the parotid glands is to be done irrespective of the intention of the treatment even in patients planned for WBRT and decrease the mean dose of the parotid glands as much as possible. The dose delivered to the paediatric parotids is much more compared to the adult parotids considering smaller parotid volumes.
References
- Tabouret E, Chinot O, Metellus P, Tallet A, Viens P, et al. (2012) Recent trends in epidemiology of brain metastases: an overview. Anticancer research 32(11): 4655-4662.
- Agboola O, Benoit B, Cross P, Da Silva V, Esche B, et al. (1998) Prognostic factors derived from recursive partition analysis (RPA) of Radiation Therapy Oncology Group (RTOG) brain metastases trials applied to surgically resected and irradiated brain metastatic cases. Int J Radiat Oncol Biol Phys42(1):155-159.
- Marsh JC, Gielda BT, Herskovic AM, Abrams RA (2010) Cognitive sparing during the administration of whole brain radiotherapy and prophylactic cranial irradiation: current concepts and approaches. J Oncol 2010:198208.
- Noh OK, Chun M, Nam SS, Jang H, Jo S, et al. (2011) Parotid gland as a risk organ in whole brain radiotherapy. Radiother Oncol98(2): 223-226.
- Ren G, Xu SP, Du L, Feng LC, Qu BL, et al. (2015) Actual anatomical and dosimetric changes of parotid glands in nasopharyngeal carcinoma patients during intensity modulated radiation therapy. Biomed Res Int2015:670327.
- Deasy JO, Moiseenko V, Marks L, Chao KC, Nam J, et al. (2010) Radiotherapy dose–volume effects on salivary gland function. Int J Radiat Oncol Biol Phys76(3):S58-63.
- Beetz I, Steenbakkers RJ, Chouvalova O, Leemans CR, Doornaert P, et al. (2014) The QUANTEC criteria for parotid gland dose and their efficacy to prevent moderate to severe patient-rated xerostomia. Acta Oncologica53(5):597-604.
- Bussels B, Maes A, Flamen P, Lambin P, Erven K, et al. (2004) Dose–response relationships within the parotid gland after radiotherapy for head and neck cancer. Radiotherapy and oncology73(3):297-306.
- Chao KC, Deasy JO, Markman J, Haynie J, Perez CA, et al. (2001) A prospective study of salivary function sparing in patients with head-and-neck cancers receiving intensity-modulated or three-dimensional radiation therapy: initial results. Int J Radiat Oncol Biol Phys49(4):907-916.
- Matsuzaki A, Ishii E, Nagatoshi Y, Eguchi H, Koga H, et al. (2001) Long-term outcome of treatment with protocols AL841, AL851, and ALHR88 in children with acute lymphoblastic leukemia: results obtained by the Kyushu-Yamaguchi Children’s Cancer Study Group. Int J Hematol73(3):369-377.






























