Endovascular Removal of Foreign Bodies
Rodrigues R1*, Anacleto G1, Agostinho A2 and Gonçalves O1
1Department of Angiology and Vascular Surgery, University Hospital Coimbra, Portugal
2Department of Radiology, University Hospital Coimbra, Portugal
Submission: May 01, 2018; Published: May 15, 2018
*Corresponding Address: Rodrigues R, Department of Angiology and Vascular Surgery, University Hospital Coimbra, Portugal, Email: roger.cc@hotmail.com
How to cite this article: Rodrigues R, Anacleto G, Agostinho A, Gonçalves O. Endovascular Removal of Foreign Bodies. Canc Therapy & Oncol Int J. 2018; 10(5): 555799. DOI: 10.19080/CTOIJ.2018.10.555799
Abstract
The use of central venous accesses in clinical practice is becoming more frequent. They are used for the administration of drugs, chemotherapy or parenteral diets. They are also used to hemodynamic monitoring, for the implantation of pacemakers or, still, for use as an access route for the endovascular treatments. It is recommended the extraction of all foreign bodies diagnosed, because this will prevent potentially serious and fatal complications. This study is focused on the migration of catheters since they represent the majority of cases of embolization. We present one of the largest published series of removal of foreign bodies with endovascular techniques.
Keywords: Foreign body; Endovascular; Catheters
Introduction
Intravascular embolization of a foreign body, either by fracture or migration, is a rare condition, occurring in approximately 1% [1]. The most common foreign bodies removed are fragments of central venous catheters. Catheter embolization is asymptomatic in most cases and is only identified on chest radiography, with other presentations including infra/supraclavicular swelling. Prompt removal of catheter fragments is preferred due to potential complications including pulmonary thromboembolism, cardiac perforation, cardiac arrest and endocarditis [2].
Objective
The objective of the present study is to demonstrate the different locations where foreign bodies, in most cases catheters, can be found, the technique used to remove them and the affected population.
Methods
This is a 9 years retrospective study in which we report the cases of foreign bodies’ removal performed by an endovascular approach between 2009 and 2017 in our institution. It includes 53 patients: 28 women and 25 men. The average age was 58 years (ranging from 15 to 87 years). The catheters were implanted by a heterogeneous group of professionals.
Results
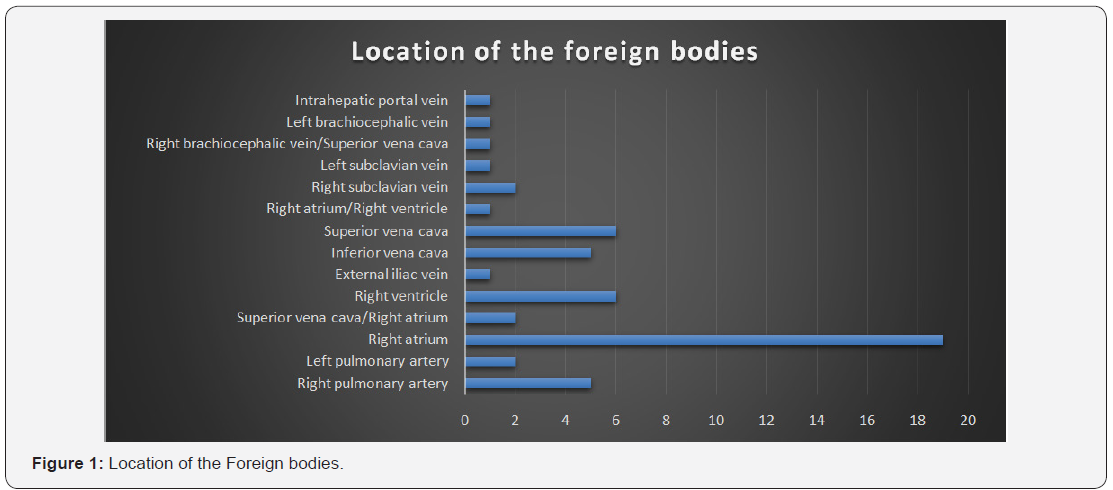
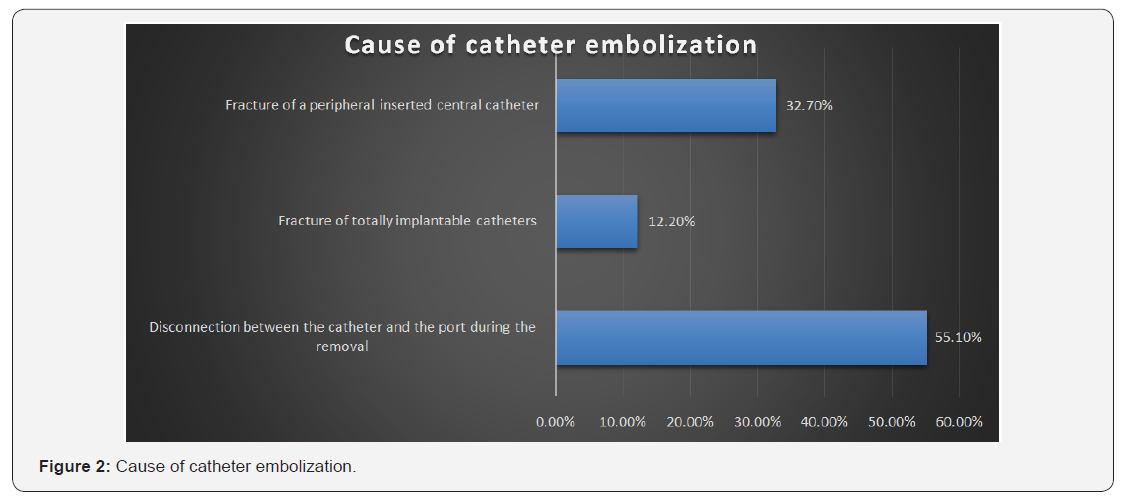
In our study we found: 33 implantable catheters (Implantofix®); 16 peripheral inserted central catheters; 3 Guide Wires; 1 angioplasty balloon; 1Amplazer vascular plug. The most common sites for the lodging of one of the ends of the intravascular foreign bodies were the right atrium (35,8%) the superior vena cava (11,3%) and the right ventricle (11,3%) (Figure 1). In 98,1% of the cases, only one venous access was used for extraction of foreign bodies, and in 96,2% of the cases the right femoral access was used. The loop-snare technique was used in 45 cases (84.9%) and in 8 cases a basket was the option. The most common cause of catheter embolization was the disconnection between the catheter and the port during the surgery for its removal, which occurred in 55,1% of the cases. Fracture of totally implantable catheters occurred in 12.2 %. The fracture of a peripheral inserted central catheter represents 32,7 % of cases of embolization (Figure 2). Atrial fibrillation, occurred in 8 cases. The mortality rate during the procedure was zero. Technical success was 100%.
Discussion
In the present study, most catheters extracted were totally implantable type catheters which, maybe because they must be in place for a longer period of time, might cause them to wear and tear more quickly [3-4]. Catheter fracture may be also related to tearing of the catheter during insertion or traction and/or pinching of the catheter hub junction, allowing fatigue of the catheter material and subsequent dislodgement. Another cause of fracture can is a chronic compression of the catheter between the clavicle and the first rib, known as a pinch-off syndrome. This syndrome may be prevented by using the jugular access, or else by the implantation of the catheter in the most lateral part of the subclavian vein [5]. When the foreign bodies are located in the cardiac cavities we recommend their removal with the presence of a Cardiologist due to the risk of potentially life-threatening arrhythmias [6].
Conclusion
Percutaneous intervention for removal of intravascular foreign bodies is currently the best treatment option for these patients. It is a minimally invasive, procedure, with low complication rates. Given the subtle nature of the embolization and the potential complications, clinicians should be vigilant for catheter fracture and embolization. Embolised material can be quite safely retrieved and this presents an attractive alternative to surgical removal of these devices. Our paper demonstrates the efficacy and safety of endovascular catheter removal, but also highlights the need for surveillance of catheter quality and their adequate management in order to reduce this type of complications.
References
- Smouse HB, Fox PF, Brady TM, Swischuk JL, Castañeda F, et al. (2000) Intravascular foreign body removal. Semin Intervent Radiol 17: 201- 212.
- Fisher RG, Ferreyro R (1978) Evaluation of current techniques for nonsurgical removal of intravascular foreign bodies. Am J Roentgenol 130: 541-548.
- Aitken DR, Minton JP (1984) The pinch-off sign: a warning of impending problems with permanent subclavian catheters. Am J Surg 148(5): 633-636.
- Surov A, Jordan K, Buerke M, Persing M, Wollschlaeger B, et al. (2006) Atypical pulmonary embolism of port catheter fragments in oncology patients. Support Care Cancer 14(5): 479-483.
- Motta-Leal-Filho JM, Carnevale F, Nasser F, Santos A, Junior W, et al. (2010) Táticas e técnicas endovasculares para retirada de corpos estranhos intravenosos. Rev Bras Cir Cardiovasc 25(2): 202-208.
- Denny MA, Frank LR (2003) Ventricular tachycardia secondary to Porta- Cath fracture and embolization. J Emerg Med 24(1): 29-34.






























