Case Report: Two cases of Typical Hepatic Hemangioma
Sushila B Ladumor*
Consultant Radiologist, Hamad Medical Corporation, Qatar
Submission: February 14, 2018; Published: April 19, 2018
*Correspondence Address: Sushila B Ladumor, Consultant Radiologist, Hamad Medical Corporation, Clinical Radiology Weil Cornel Medical College, Doha, Qatar, Email: drsbladumor@yahoo.com
How to cite this article: Sushila B L. Case Report: Two cases of Typical Hepatic Hemangioma. Canc Therapy & Oncol Int J. 2018; 10(2): 555785. DOI: 10.19080/CTOIJ.2018.10.555785
Abstract
Hemangioma is the most common focal solid benign tumor of the liver which usually diagnosed incidentally same as these cases. Majority of the patients are asymptomatic. Main radiology challenge is to differentiate from other focal solid hepatic neoplasm [1] particularly in cases of atypical hemangioma and hemangioma in fatty liver or other diseased liver.
Keywords: US; CT; MRI (dynamic post-contrast); Hyper echoic; Hypo echoic; Low density; High signal; Low signal; Peripheral nodular; Centripetal enhancement
Abbrevations: US: Ultrasound; CT: Computed Tomography; MRI: Magnetic Resonance Imaging; KUB: Kidney, Ureter and Urinary bladder; CSF: Cerebrospinal Fluid
Clinical History
Both cases are young female with history of renal/ureteric colic. First one for US and second one for un-enhanced CT KUB. After initial imaging findings patient referred for MRI to further characterize the lesion.
Imaging Findings
US
First case referred for US and incidentally diagnosed focal sub capsular hyper echoic liver lesion.
CT
The second case referred for non-contrast CT KUB which demonstrates multiple low density liver lesions, more in right lobe.
MRI with and without Contrast
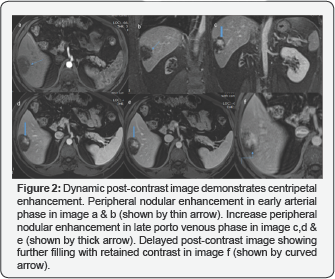
In both cases MRI shows lesion as low signal in T1 weighted sequences, high signal in T2 weighted sequences with dynamic post-contrast images reveals early peripheral nodular enhancement with gradual centripetal filling and complete enhancement with retained contrast in delayed postcontrast images representing typical imaging features of hepatic hemangioma (Figures 1-4).

Discussion
Hepatic haemangiomas, also known as hepatic venous malformations, are benign non-neoplastic solid hyper vascular liver lesions. It commonly diagnosed incidentally in asymptomatic cases of about 20%. Hemangiomas are often solitary, but multiple lesions may be present in both the right and left lobe of the liver in up to 40 percent of patients [2]. The size of hepatic hemangioma varies from a few millimeters to over 20cm. The majority are small (<5cm). Those larger than 5cm have been referred to as giant hemangiomas.

Although they can be diagnosed at any age, 60 to 80 percent of cases are diagnosed in patients who are between the ages of 30 and 50 years. Small hemangiomas are seen more frequently with helical CT, whereas they are easily overlooked on conventional CT because they becomes is dense to liver on late-phase images [2].
They are frequently diagnosed as an incidental finding on imaging, and most patients are asymptomatic. From a radiologic perspective, it is important to differentiate haemangiomas from hepatic neoplasms
The characteristic imaging findings for typical hemangioma are as follows [1]:
a. On US it is usually well-defined hyper echoic
b. On unenhanced CT, seen as low density similar to that of vessels; on dynamic contrast-enhanced CT the lesion demonstrates peripheral globular enhancement and a centripetal fill-in pattern with the attenuation of enhancing areas similar to that of the aorta and blood pool.

On MR imaging, the hemangioma shows high signal on T2- and heavily T2-weighted sequence and low signal in T1 weighted sequence which is comparable to signal of CSF in T1 and T2 weighted sequences. Dynamic post-contrast sequences reveal enhancing pattern same as CT with peripheral globular enhancement and a centripetal fill-in pattern with the attenuation of enhancing areas identical to that of the aorta and blood pool. Heavily T2 weighted images helps to detect even tiny focal hemangioma which can be overlooked in CT easily same as in our second case [3,4].
Hepatic haemangiomas are much more common in females, with a F:M of up to 5:1. Hepatic haemangiomas are thought to be congenital in origin, benign solid tumor and are almost always of the cavernous subtype. Blood supply is predominantly hepatic arterial, similar to other liver tumors. A peripheral location within the liver is most common [3].
SPECT
99Tc RBC labelled SPECT can be sensitive for larger lesions and typically demonstrate decreased activity on initial dynamic images followed by increased activity on delayed, blood pool images.
Differential Diagnosis
Typical hepatic hemangioma has characteristic imaging feature with relatively no differential diagnosis.
References
- Hyun-Jung Jang, Tae Kyoung Kim, Hyo Keun Lim, Sang Jae Park, Jung Suk Sim, et al. (2003) Hepatic Hemangioma: Atypical Appearances on CT, MR Imaging, and Sonography. AJR 180(1).
- Klotz T, Montoriol PF, Da Ines D, Petitcolin V, Joubert-Zakeyh J, et al.(2013) Hepatic haemangioma: common and uncommon imaging features. Diagn Interv Imaging 94(9): 849-859.
- Michael P Curry, Sanjiv Chopra (2013) Hepatic hemangioma. Uptodate.
- Jay P Heiken (2007) Distinguishing benign from malignant liver tumours. Cancer Imaging 1:7.






























