Metastatic Melanomas of the Groin Lymph Nodes without Known Primary Lesion in a Developing Community
Wilson I B Onuigbo*
Department of Pathology, Medical Foundation and Clinic, Nigeria
Received: April 14, 2017; Published: April 19, 2017
*Corresponding author: Wilson I B Onuigbo, Department of Pathology, Medical Foundation and Clinic, 8 Nsukka Lane, Enugu 400001, Nigeria, Email: wilson.onuigbo@gmail.com
How to cite this article: Wilson I B O. Metastatic Melanomas of the Groin Lymph Nodes without Known Primary Lesion in a Developing Community. Canc Therapy & Oncol Int J. 2017; 4(4): 555643. DOI: 10.19080/CTOIJ.2017.04.555643
Abstract
Melanoma could present with metastasis from an unknown primary. It is an event reported to happen in 2-3%. In particular, lymph nodes could be the organs involved as reported in a USA case recently. Therefore, the author reports 8 cases obtained from a histopathology data pool situated in a developing community; this idea followed the suggestion of a Birmingham (UK) group, namely, that such a pool promotes epidemiological analysis.
Keywords: Melanoma; Metastasis; Lymph nodes; Unknown primary; Epidemiology; Developing community.
Introduction
In a recent USA case report [1], a 58-year-old Caucasian male presented with a right sided swelling in the inguinal region. It was surgery that revealed it to be due to metastatic melanoma. As no cutaneous lesion was identified by history or physical examination, it was theorized that spontaneous regression was a possibility. Accordingly, it is desirable to publish such cases worldwide. The present cases were documented in a Nigerian community due to following the suggestion made by a Birmingham (UK) group [2], namely, that the establishment of a histopathology data pool promotes epidemiological analysis.
Investigation
*No 2 is worthy a of full account.
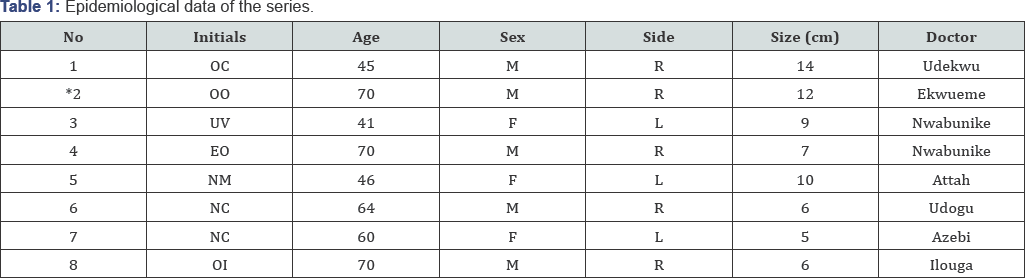
The establishment of a Regional Pathology Laboratory in 1970 in Enugu, the capital ofthe Eastern Region of Nigeria, helped matters, seeing that the author became the pioneer pathologist. Therefore, this investigation concerns the benefitting Nigerian ethnic group, the Igbos or Ibos [3]. In particular, the clinicians working among them were encouraged to send formalin-fixed biopsy specimens complete with notes as to age, sex, complaints and any interesting findings [Table 1].
OO, a 70-year-old man, presented at the University of Nigeria Teaching Hospital, Enugu, with a lump in the right groin of 3 years duration. There was no associated history of ulceration in the drainage area. This was carefully biopsied. The submitted skin ellipse measured 12 x 10 cm and there was a central ulcer. Below it, there was a 15 x 5 x 4 cm mass. On section, it was inky black and necrotic in the center. There were solid satellites up to 2 cm across. Microscopy revealed an ulcerated growth undermined by a necrotic melanin forming spindle called growth. There was no junctional activity. Malignant melanoma was diagnosed.
Remarks
As regards both site and structure, the probability is that this is a metastasis. The primary is either healed as is known to occur rarely or hidden in urethra, anus or rectum.
Discussion
In the treatment of melanoma, the standard of cure for palpable groin lymph nodes is dissection [4,5]. This was undertaken in the present series.
Surprisingly, the nearer group is not the groin but the popliteal group in terms of pedal primaries. Therefore, it must have been skipped, a well known mechanism in metastasis [6]. Little wonder that case reports have been recorded lately in terms of the melanoma [7-9]. Indeed, the author has personally challenged researchers [10]; they should explain why this is a rarity in lung cancer in which millions of cancer cells necessarily enter the circulation [11].
Perhaps, in the case of melanomas, one is up against a tumor endowed with molecular and genetic diversity [12]. Incidentally, there is even inter-observer variation in the histopathological diagnosis of clinically suspicious pigmented skin lesions [13]. In the circumstances, what is new, asked Evoy's group [14], "in the management of malignant melanoma?" As they answered, "The combination of sentinel lymph node mapping coupled with immunotherapy in node-positive patient may have potential to increase survival." Of course, this concept is a far cry in terms of a developing community!
References
- Shimada K, Ichikawa T, Aono G, Oohara T, Abe R, et al. (2010) Malignant melanoma of rare occurrence in the digestive organs; review of the Japanese literature. Geka Jpn J Surg 72: 503-508.
- Katz SC, Bowne WB, Wolchok JD, Busam KJ, Jaques DP, et al. (2007) Surgical management of melanoma of the gallbladder: a report of 13 cases and review of the literature. Am J Surg 193(3): 493-497.
- Takada T (2007) Clinical practice guidelines for management of biliary tract & ampullary carcinomas. J Hepatobiliary Pancreat Surg 15(1): 1.
- M Guida, A Cramarossa, A Gentile, M De Lena (2003) Metastatic malignant melanoma of the gallbladder: a case report and review of the literature. Melanoma Research 12(6): 619-625.
- U Kohler, T Jacobi, G Sebastian, M Nagel (2000) Laparoscopic cholecystectomy in isolated gallbladder metastasis of malignant melanoma. Chirurg 71(12): 1517-1520.
- DL Bartlett (2000) Gallbladder cancer. Semin Surg Oncol 19(2): 145¬155.
- Schwimmer J, Essner R, Patel A, Jahan SA, Shepherd JE, et al. (2000) A review of the literature for whole-body FDG PET in the management of patients with melanoma. Q J Nucl Med 44(2): 153-167.
- Cellerino P, Corsi F, Morandi E, Foschi D, Trabucchi E (2000) Metastatic melanoma of the gallbladder. Eur J Surg Oncol 26(8): 815-816.
- Dong XD, De Matos P, Prieto VG, Seigler HF (1999) Melanoma of the gallbladder: are view of cases seen at Duke University Medical Center. Cancer 85(1): 32-39.
- Blecker D, Abraham S, Furth EE, Kochman ML (1999) Melanoma in the gastrointestinal tract. Am J Gastro enterol 94(12): 3427-3433.
- BJ Holloway, DM King (1997) Ultrasound diagnosis of metastatic melanoma of the gallbladder. Br J Radiol 70(839): 1122-1125.
- MH Seelig, K Schonleben (1997) Laparoscopic cholecystectomy for a metastasis of a malignant melanoma in the gallbladder. Zeitschrift fur Gastroenterologie 35(9): 673-675.
- Manolidis S, Donald PJ (1997) Malignant mucosal melanoma of the head and neck: review of the literature and report of 14 patients. Cancer 80: 1373-1386.
- Ollila DW, Essner R, Wanek LA, Morton DL (1996) Surgical resection for melanoma metastatic to the gastrointestinal tract. Arch Surg 131(9): 975-980.
- Isiklar I, Leeds NE, Fuller GN, Kumar AJ (1995) Intracranial metastatic melanoma: cor-relation between MR imaging characteristics and melanin content. AJR Am J Roentgenol 165(6): 1503-1512.
- Avila NA, Shawker TH, Fraker D (1994) Color-flow Doppler ultrasonography in metastatic melanoma of the gallbladder. J Clin Ultrasound 22(5): 342-347.
- Balch CM, Houghton AM (1992) Diagnosis of metastatic melanoma at distant sites. Cutaneous melanoma (2nd edn), Lippincott, Philadelphia, USA, pp. 439-467.
- Stutte H, Muller PH, D Hoedt B, Stroebel W (1989) Ultrasonographic diagnosis of melanoma metastases in liver, gallbladder, and spleen. J Ultrasound Med 8(10): 541-547.
- DI Heath and C Womack (1988) Primary malignant melanoma of the gall bladder. Journal of Clinical Pathology 41(10): 1073-1077.
- N Daunt, DM King (1982) Metastatic melanoma in the biliary tree. British Journal of Radiology, 55(659): 873-874.
- Backman H (1969) Metastases of malignant melanoma in the gastrointestinal tract. Geriatrics 24: 112-120.
- Abrams HL, Spiro R, Goldstein N (1950) Metastases in carcinoma; analysis of 1000 autopsied cases. Cancer 3(1): 74-85.






























