A Rare Case of Merkel Cell Carcinoma Presented with Lambert Eaton Myasthenic Syndrome without Cutaneous Findings
K Tsapakidis1*, I Samaras1, K Papacharalampous1, E Maragkouli1, V Papadopoulos1, I Litos1, Esogka1, M Tolia2, GK Koukoulis3 and G Papatsimpas1
1Department of Medical Oncology, University Hospital of Larissa, Greece
2Department of Radiotherapy, University Hospital of Larissa, Greece
3Department of Pathology, University Hospital of Larissa, Greece
Submission: March 25, 2017; Published: April 04, 2017
*Corresponding author: Konstantinos Tsapakidis, Department of Medical Oncology, University Hospital of Larissa, Mezourlo 41110, Larissa, Greece, Tel: +306946123619, Fax: +302413006963,Email: tsapakidisk@yahoo.com
How to cite this article: K Tsapakidis, I Samaras, K Papacharalampous, E Maragkouli, V Papadopoulos, et al. A Rare Case of Merkel Cell Carcinoma Presented with Lambert Eaton Myasthenic Syndrome without Cutaneous Findings. Canc Therapy & Oncol Int J. 2017; 4(2): 555631. DOI: 10.19080/CTOIJ.2017.04.555631
Abstract
Merkel cell carcinoma (MCC) is a rare cutaneous malignancy that has a propensity for local recurrence and regional lymph node metastases. It presents in older patients with light skin tones as a rapidly growing intracutaneous nodule. Lambert-Eaton myasthenic syndrome (LEMS) is a disorder of neuromuscular junction, where most patients present with complaints of slowly progressive proximal muscle weakness as a paraneoplastic neurologic symptom of small cell carcinoma. Herein we present a case of LEMS that was diagnosed in a patient with MCC. A review of the English literature and the association of MCC with LEMS are analyzed. Only 6 cases developed LEMS on the ground of MCC. In the majority of the cases symptoms improved partially or completely with chemotherapy. MCC can be introduced with LEMS and clinicians need to have a high index of suspicion, while the combination of the clinical picture with the characteristic findings can help in the prompt diagnosis.
Keywords: Merkel cell carcinoma (MCC); Lambert-eatonmyasthenic syndrome (LEMS); Proximal muscle weakness; Lymph nodes
Introduction
Merkel cell carcinoma (MCC) first described in 1972, is a very rare aggressive skin malignancy primarily seen in white men patients above 70 years old [1] and has the propensity for local recurrence and regional lymph node metastases [2,3]. Many factors have been associated with the development of MCC, like Merkel cell polyomavirus [4], ultraviolet (UV) radiation exposure [5], and immunosuppression [ 6]. It is often clinically misdiagnosed as a benign lesion (e.g. cyst, lipoma, pyogenic granuloma), because dermoscopic findings are limited and features specific to a diagnosis of MCC have not been identified. Nevertheless, the acronym AEIOU (asymptomatic/lack of tenderness, expanding rapidly, immune suppression, older than 50 years, and ultraviolet-exposed site on a person with fair skin) can describe it fairly [5].
Case Description
Our case refers to a 50 year old man presenting with chest pain and difficulty walking, as well as arising from a chair. Thoracic and abdominal computed tomographies revealed pulmonary embolism, and enlarged left inguinal lymph nodes (with MRI of the brain being negative), (Figure 1A & B). An inguinal lymph node biopsy was performed showing histopathological and immunohisto chemical features of a Merkel cell carcinoma (pankeratin, CK20, synaptophysin, chromogranin, CD56 and NSE positive, while TTF-1 negative), (Figure 2). The main clinical findings were proximal muscle weakness, depressed deep tendon reflexes and dry mouth. Skin examination of the lower limbs, external genitalia and anus was normal. He had a characteristic neurophysiological examination indicating a presynaptic transmission deficitand subsequently was tested for the presence of voltage-gated calcium channel (VGCC) antibodies, based on the clinical suspicion of having Lambert Eaton Myasthenic Syndrome (LEMS). The test was positive and, based on the result of the inguinal lymph node biopsy he was started on chemotherapy (six cycles of cisplatin plus etoposide). The patient gradually regained his muscle strength and re-evaluation by CTs showed a partial response of the disease. Thus, he was submitted to a left groin lymphadenectomy. Histopathologic examination confirmed the initial findings, showing destruction of the architecture of the lymph node parenchyma by a tumor with neuroendocrine features.
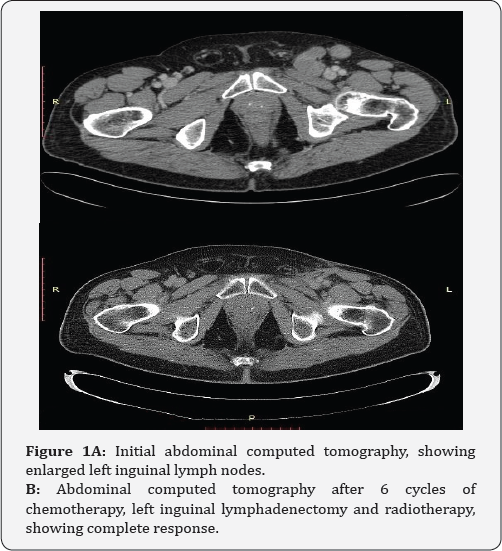
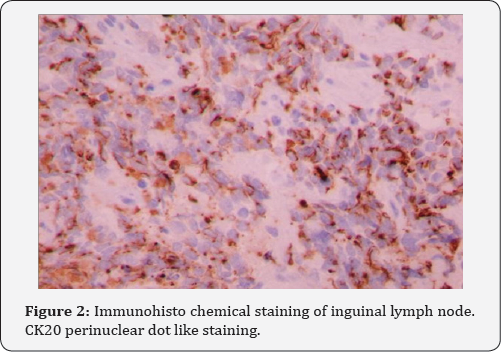
Neoplastic cells exhibited scant eosinophilic/acidophilic cytoplasmic rim, round and vesicular nuclei with finely granular/dusty chromatin and multiple nucleoli. Mitotic figures and apoptotic bodies were plentiful. Immunohisto chemically, positivity for CK20, synaptophysin and chromogranin was observed. Subsequently, he received external beam radiotherapy (3D conformal technique) at the left inguinal area (52 Gy/2 Gy/ fraction) and a simultaneous integrated boost (55.9 Gy/2.15 Gy/ fraction) at the surgical bed. Computed tomographies, six weeks after the completion of radiotherapy, did not show evidence of disease (FigurelB). He remains free of disease nearly six months after the completion of radiotherapy, without neurologic sequelae.
Discussion
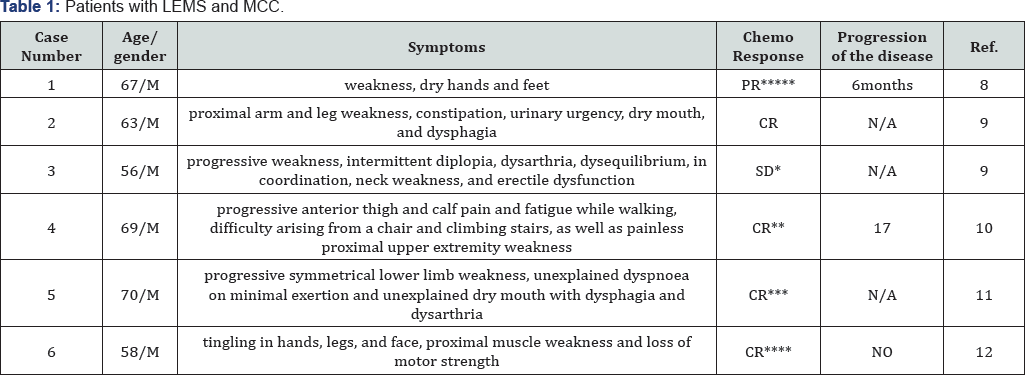
*: His neurologic and autonomic symptoms were persistent, requiring a combined regimen of pyridostigmine 90 mg 4 times daily and 3,4-diaminopyridine 20 mg 4 times daily for adequate control.
**: pyridostigmine therapy and chemotherapy.
***: only with surgery.
****: only with surgery and radiation.
*****: prednisone and chemotherapy.
Our case presented with a very rare neuro endocrine malignancy, MCC which is an extra pulmonary small cell carcinoma, and a para neoplastic neurologic complication, LEMS. LEMS is often found together with SCLC [7], but not with MCC, as it has been only described in six male cases in the literature, with a mean age of 63 years old, even without any cutaneous lesion (Table 1) [8-12]. LEMS is an uncommon disorder of neuromuscular junction transmission presenting as slowly progressive proximal muscle weakness with the patients describing an alteration in gait or difficulty arising from a chair or managing stairs [13]. The most effective therapy of LEMS is cancer-associated treatment chemotherapy, while surgery as well as radiotherapy, prednisone and pyridostigmine may provide some assistance to that [8]. Clinicians need to have a high index of suspicion and request any necessary test when the syndrome is suspected, in order to establish the diagnosis and offer the appropriate treatment to the patients. LEMS may be the first sign of MCC, a rare cancer whose early recognition is very important, as survival depends mainly on the extent of the disease and in a lesser degree on other factors, like female sex, age less than 65 years, and the absence of co morbid conditions [14,15].
Summary
We describe a rare presentation of MCC, a rare extra pulmonary SCC, and its association with paraneoplastic neurologic disease, LEMS. Clinicians must maintain a high index of suspicion for syndromes in which antibody markers suggest SCLC and chest imaging findings are normal.
Conflict of Interests
We declare any financial interest or any conflict of interest.
References
- Albores Saavedra J, Batich K, Chable Montero F, Sagy N, Schwartz AM, et al. (2010) Merkel cell carcinoma demographics, morphology, and survival based on 3870 cases: a population based study. J Cutan Pathol 37(1): 20-27.
- Tothill R, Estall V, Rischin D (2015) Merkel cell carcinoma: emerging biology, current approaches, and future directions. Am Soc Clin Oncol Educ Book 2015: e519.
- Toker C (1972) Trabecular carcinoma of the skin. Arch Dermatol. 105(1): 107-110.
- Feng H, Shuda M, Chang Y, Moore PS (2008) Clonal integration of a polyomavirus in human Merkel cell carcinoma. Science 319(5866): 1096-1100.
- Heath M, Jaimes N, Lemos B, Mostaghimi A, Wang LC, et al. (2008) Clinical characteristics of Merkel cell carcinoma at diagnosisin 195 patients: the AEIOU features. J Am Acad Dermatol 58(3): 375-381.
- Clarke CA, Robbins HA, Tatalovich Z, Lynch CF, Pawlish KS, et al. (2015) Risk of merkel cell carcinoma after solid organ transplantation. J Natl Cancer Inst 107(2).
- Galanis E, Frytak S, Rowland KM Jr, Sloan JA, Lennon VA (1999) Neuronal autoantibody titers in the course of small-cell lung carcinoma and platinum-associated neuropathy. Cancer ImmunolImmunother 48(2-3): 85-90.
- Bombelli F, Lispi L, Calabro F, Corsi FM, Petrucci A (2015) LambertEaton myasthenic syndrome associated to Merkel cell carcinoma: report of a case. Neurol Sci 36(8): 1491-1492.
- Simmons DB, Duginski TM, McClean JC, Amato AA, Sladky JH (2016) Lambert-eatonmyasthenic syndrome and merkel cell carcinoma. Muscle Nerve 53(2): 325-326.
- Eggers SD, Salomao DR, Dinapoli RP, Vernino S (2001) Paraneoplastic and metastatic neurologic complications of Merkel cell carcinoma. Mayo Clin Proc 76(3): 327-330.
- Siau RT, Morris A, Karoo RO (2014) Surgery results in complete cure of Lambert-Eaton myasthenic syndrome in a patient with metastatic Merkel cell carcinoma. J Plast Reconstr Aesthet Surg 67(6): e162-164.
- Iyer JG, Parvathaneni K, Bhatia S, Tarabadkar ES, Blom A, et al. (2016) Paraneoplastic syndromes (PNS) associated with Merkel cell carcinoma (MCC): A case series of 8 patients highlighting different clinical manifestations. J Am Acad Dermatol 75(3): 541-547.
- O Neill JH, Murray NM, Newsom Davis J (1988) The Lambert-Eaton myasthenic syndrome.A review of 50cases. Brain 111(3): 577-596.
- Tai PT, Yu E, Tonita J, Gilchrist J (2000) Merkel cell carcinoma of the skin. J Cutan Med Surg 4: 186.
- Eng TY, Boersma MG, Fuller CD, Cavanaugh SX, Valenzuela F, et al. (2004) Treatment of merkel cell carcinoma.Am J Clin Oncol 27(5): 510-515.






























