Connective Tissue Disease and its Evolution on Chest CT
Mary Salvatore1,3*, Aditi Mathur2, Ling Fang Guo BA1, Timothy O’Connor1 and Maria Padilla2
1Department of Radiology, Icahn School of Medicine at Mount Sinai, New York
2Department of Medicine, Icahn School of Medicine at Mount Sinai, New York
3Department of Radiology, Columbia University Medical Center, New York
Submission: October 03, 2019; Published: October 28, 2019
*Corresponding author: Mary Salvatore, Department of Radiology, Columbia University Medical Center New York
How to cite this article: Mary Salvatore, Aditi Mathur, Ling Fang Guo BA, Timothy O’Connor, Maria Padilla. Connective Tissue Disease and its Evolution on Chest CT.Curr Trends Clin Med Imaging. 2019; 2(5): 555621. DOI: 10.19080/CTCMI.2019.02.555621
Abstract
Background/Objective: Evaluate the radiographic appearances most commonly associated with Connective Tissue Diseases (CTD) and their evolution over time.
Methods: This systematic review draws data from the IRB approved Mount Sinai Interstitial Lung Disease Registry with 381 enrolled patients at the time of this review. CT scans of 108 patients with a working diagnosis of connective tissue disease (CTD) were evaluated by a Radiologist (MS with 20 years of experience) a Pulmonologist (AM with 5 years of experience). The patient’s first CT scan demonstrating fibrosis and every CT scan at least one year later were reviewed, and the pattern of fibrosis and extent of disease were recorded by consensus agreement.
Results: 108 patients out of 381(28%) had a working diagnosis of CTD based on clinical presentation, serologic markers and chest CT. 80 had multiple CT scans allowing follow-up over time. 35% of the patients had myositis. 24% of patients had a diagnosis of scleroderma (SC). The remaining had organizing pneumonia (OP) (11%), rheumatoid arthritis (RA) (8%), interstitial pneumonia with autoimmune features (IPAF) (6%), mixed connective tissue disease (MCTD) (5%), sjogren’s (Sj) (5%), undifferentiated (UN) (4%) and vasculitis (V) (2%). The radiographic pattern of disease changed over time in 35%. 44% of patients with OP diagnosis returned to normal on follow-up. 50 (63%) of patients had worsening disease on CT over time. 12 (15%) decreased extent of disease or resolved. 18 (23%) remained stable.
Cоnclusiоn: There are many types of CTD with variable radiographic presentations, which can change over time. The diseases are frequently progressive with few returning to normal.
Keywords: Connective tissue disease, Pulmonary fibrosis, Organizing pneumonia, Nonspecific Interstitial pneumonitis, Usual interstitial pneumonitis
Intrоductiоn
There are many types of pulmonary fibrosis which are differentiated by their clinical presentation, radiology and pathology. The most common type of pulmonary fibrosis and the one with the highest morbidity and mortality is idiopathic pulmonary fibrosis (IPF). The pattern on CT scan is a usual interstitial pneumonitis (UIP) pattern which has been defined by the American Thoracic Society, the European Respiratory Society, the Japanese Respiratory Society, and the Latin American Thoracic Association (ATS/ERS/JRS/ALAT) as sub- pleural basilar predominant fibrosis with honeycombing [1]. New anti-fibrotic treatments slow the progression of the disease but do not reverse the disease so fibrosis on CT scans remains stable or progresses [2]. The CTDs affect younger individuals with a female predominance. The CTDs are subdivided based on clinical, radiology and serologic features. The findings on chest CT are more variable than with IPF. They can include nonspecific interstitial pneumonitis (NSIP), organizing pneumonia (OP), UIP, and even chronic hypersensitivity pneumonitis (CHP) patterns [3,4]. The pattern can change over time and even resolve with treatment, making radiology diagnosis challenging. Understanding the most common patterns associated with each type of CTD and the evolution can help with diagnosis and treatment recommendations. The purpose of this paper is to evaluate the radiographic appearances most commonly associated with each CTD and their evolution over time.
Methods
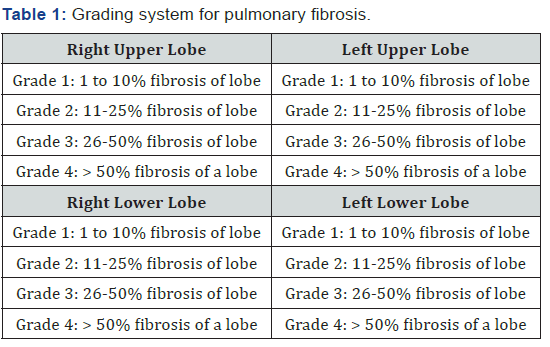
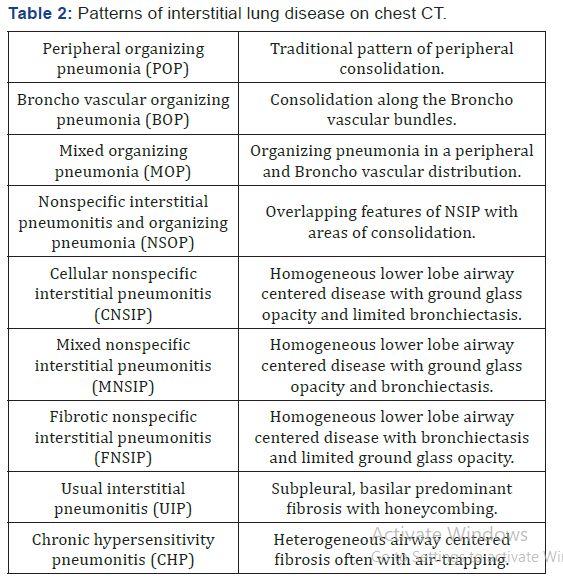
Internal Review Board approval was obtained. Our paper draws patients from the Mount Sinai ILD Registry, which at the time of the study contained 381 patients with pulmonary fibrosis among whom 108 had a CTD Working Diagnosis based on a multidisciplinary approach. Patients signed an informed consent to participate in the registry. The age and gender of each patient was recorded as well as the specific CTD diagnosis. The first CT scan with evidence of interstitial lung disease and all follow up CT scans that were at least 1 year apart were reviewed by a thoracic radiologist and pulmonologist and their consensus opinion was recorded. The date of the CT scan, the pattern of disease and the extent of disease were recorded. The grading of extent of disease was based on a previously reported grading system for lung fibrosis [5] (Table 1). The right upper lobe and right middle lobe are considered as one lobe in this grading system. The maximum score is 16. The pattern of disease is described in (Table2) (Figure1).
Results
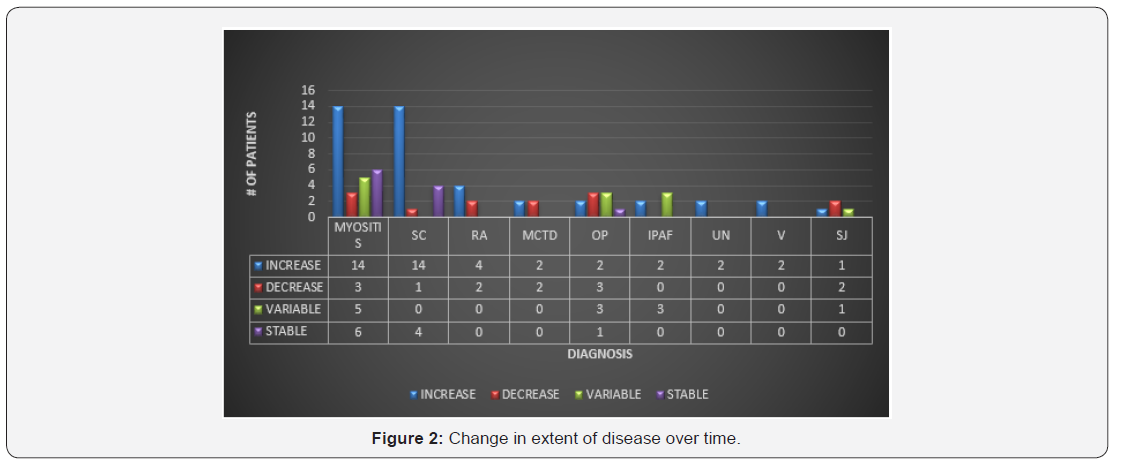
108 patients out of 381(28%) had a working diagnosis of CTD. Of those 108 patients, 80 had multiple CT scans allowing assessment of CT pattern and extent of disease over time. 28 (35%) of the patients had myositis which included dermatomyositis, polymyositis and antisynthetase diagnoses. 19 (24%) of patients with CTD had a diagnosis of scleroderma. The remaining patients had OP 9 (11%), RA 6 (8%), IPAF 5 (6%), MCTD 4 (5%), sjogren’s 4 (5%), undifferentiated 3 (4%) and vasculitis 2 (2%). The oldest patients were in the idiopathic group and the youngest patients had a working diagnosis of MCTD. All patients with MCTD and sjogren’s were females. Overall, 6 patients returned to normal on CT over the course of their disease, 4 of these patients had a diagnosis of organizing pneumonia. 50 (63%) of patients had worsening disease on CT over time. 12 (15%) decreased extent of disease or resolved. 18 (23%) remained stable. 36 patients had an NSIP pattern on first CT. 18 had OP, 14 had NSOP, 9 had UIP and 3 had CHP pattern (Figure 2 & 3).
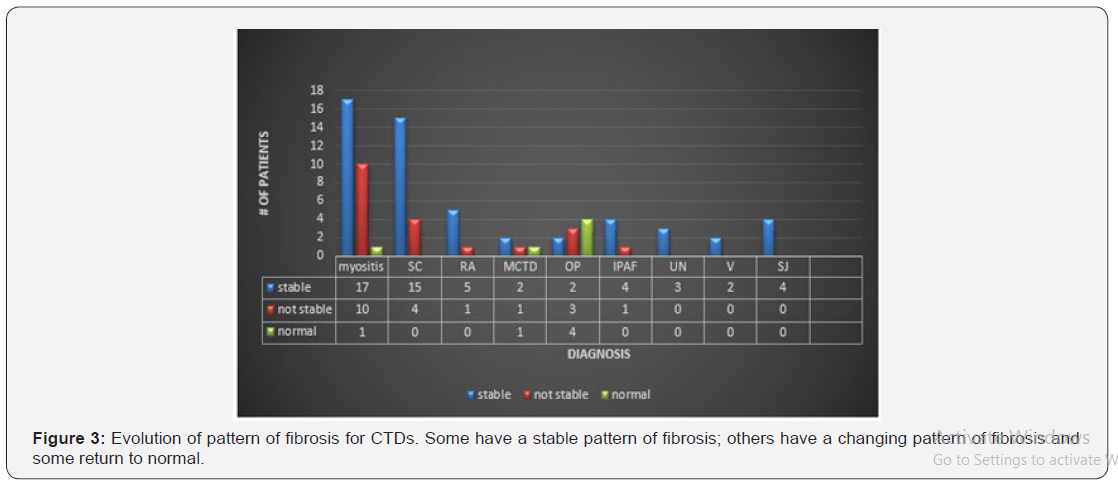
Myositis-35% of the patients with CTD had myositis which included dermatomyositis, polymyositis and anti-synthetase diagnoses. The average age was 57 years old. The percentage of female patients was 46 %. NSIP and NSOP patterns were most common as seen with other researchers including Debray who found 45% had an NSIP pattern [6]. Half of the patient’s extent of fibrosis progressed over the study interval however the pattern of disease remained relatively stable. 1/28 patients CT returned to normal (Table 3). Scleroderma-24% of patients with CTD had a diagnosis of scleroderma. The average age was 63 and 78% were women. The NSIP pattern was most common but a few people had a UIP pattern which is similar to other authors [7]. Many patients (74%) progressed and none returned to normal suggesting overall, that this is a CTD with a worse prognosis (Table 4). Organizing Pneumonia-11% of patients with CTD had OP. The average age in our study was 57 which was relatively young. Only 11% were female. As would be expected nearly all the patients had an OP pattern on CT as has been described in the literature. Nearly half improved over the course of follow-up but some had a waxing and waning course as is typical of the disease.


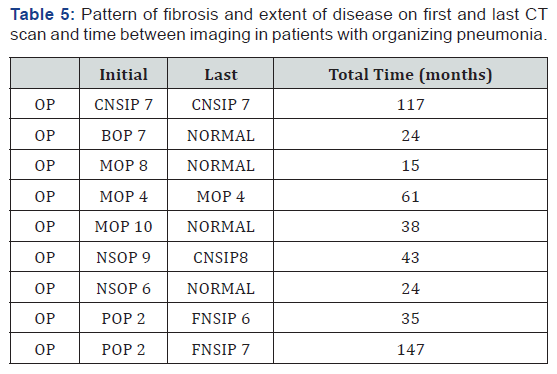
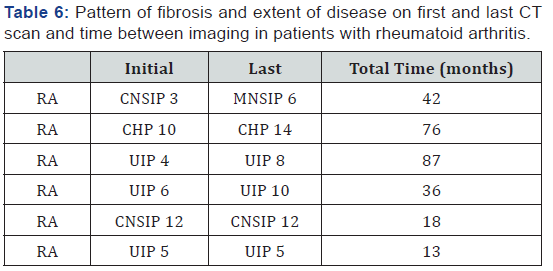
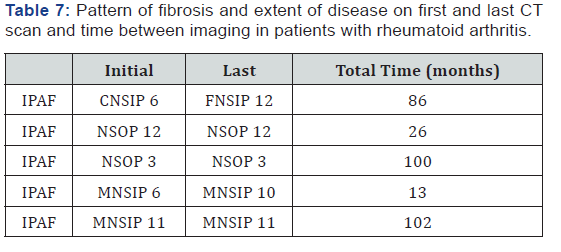
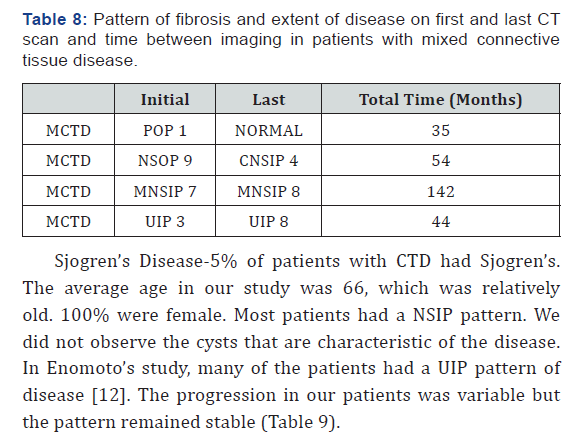
Most continued to have the same pattern of disease over time. 4 CTs returned to normal supporting the idea that OP has a good prognosis (Table 5). Rheumatoid Arthritis- 9% of patients with CTD had RA. The average age in our study was 66 and 83% were female. 3/6 had a UIP pattern similar to that which has been described in the literature [8]. None improved over the course of follow-up. Most continued to have the same pattern of disease over time. No patient with RA returned to normal on CT (Table 6). Idiopathic Pulmonary Fibrosis with Autoimmune Features: 6% of patients with CTD had IPAF, defined as a combination of findings of at least 2 of the following; clinical manifestations of CTD, positive serologies or specific chest CT pattern or pathology [9]. The average age in our study was 66, which was relatively old. 80% were female. Most patients had an NSIP pattern (60%). Chung found that UIP pattern was more common in the patients he studied [10] (Table 7). Mixed Connective Tissue Disease-5% of patients with CTD had MCTD. The average age in our study was 58, which was relatively young. 100% were female. There was a variable appearance on CT with no predilection for a specific pattern [11]. Most continued to have the same pattern of disease over time. One person’s CT returned to normal (Table 8).
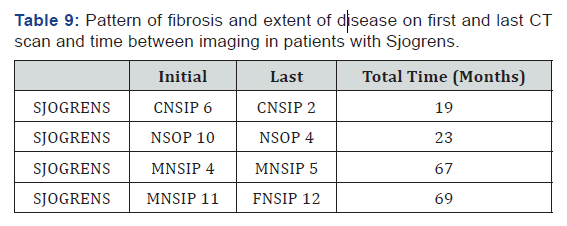
Sjogren’s Disease-5% of patients with CTD had Sjogren’s. The average age in our study was 66, which was relatively old. 100% were female. Most patients had a NSIP pattern. We did not observe the cysts that are characteristic of the disease. In Enomoto’s study, many of the patients had a UIP pattern of disease [12]. The progression in our patients was variable but the pattern remained stable (Table 9).
Discussion
Ultimately, there are many types of CTD and they have variable radiographic presentations, which can evolve differently over time. The variability of the radiographic appearance within a specific type of CTD is interesting as is the overlap in appearance between different diseases. The OP pattern which is seen in many of the CTD is typically early and often resolves. In contrast the NSIP pattern is more likely to be persistent. Lung manifestations may be present prior to joint manifestations so it is important for rheumatologists to consider the lung in evaluation of patients with suspected connective tissue diseases. Further research is needed to determine the effect of immunosuppressant drugs on the evolution of findings on chest CT and determine if clinical parameters parallel radiographic appearance [13].
References
- Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, et al. (2011) An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med 183(6): 788-824.
- Pollack AFDA (2014) Approves First 2 Drugs for Treatment of a Fatal Lung Disease. NY Times.
- Gutsche M, Rosen GD, Swigris JJ (2012) Connective Tissue Disease-associated Interstitial Lung Disease: A review. Curr Respir Care Rep1: 224-232.
- Li H, Xiong Z, Liu J, Li Y, Zhou B (2017) Manifestations of the connective tissue associated interstitial lung disease under high-resolution computed tomography. Zhong Nan Da Xue Xue Bao Yi Xue Ban 42(8): 934-939.
- Salvatore M, Henschke CI, Yip R, Jacobi A, Eber C, et al. (2016) Evidence of Interstitial Lung Disease on Low-Dose Chest CT Images: Prevalence, Patterns, and Progression. AJR Am J Roentgenol 206(3): 487-494.
- Debray MP, Borie R, Revel MP, Naccache JM, Khalil A, et al. (2015) Interstitial lung disease in anti-synthetase syndrome: initial and follow-up CT findings. Eur J Radiol 84(3): 516-523.
- Ostojic P, Cerinic MM, Silver R, Highland K, Damjanov N (2007) Interstitial lung disease in systemic sclerosis. Lung 185(4): 211-220.
- Tanaka N, Kunihiro Y, Kubo M, Kawano R, Oishi K, et al. (2018) HRCT findings of collagen vascular disease-related interstitial pneumonia (CVD-IP): a comparative study among individual underlying diseases. Clin Radiol 73(9):e1-833.e10.
- Végh J, Szilasi M, Soós G, Dévényi K, Dezso B, Soltész P, et al. (2005) Interstitial lung disease in mixed connective tissue disease. Orv Hetil 146(48): 2435-2443.
- Roberton BJ, Hansell DM (2011) Organizing pneumonia: a kaleidoscope of concepts and morphologies. Eur Radiol 21(11): 2244-2254.
- Fabrizio Luppi, Athol U Wells (2016) Interstitial pneumonitis with autoimmune features (IPAF): a work in progress. European Respiratory Journal 47: 1622-1624.
- Chung JH, Montner SM, Adegunsoye A, Lee C, Oldham JM, et al. (2017) CT Findings, Radiologic-Pathologic Correlation, and Imaging Predictors of Survival for Patients with Interstitial Pneumonia with Autoimmune Features.AJR Am J Roentgenol 208(6): 1229-1236.
- Enomoto Y, Takemura T, Hagiwara E, Iwasawa T, Okudela K, et al. (2014) Features of usual interstitial pneumonia in patients with primary Sjögren׳s syndrome compared with idiopathic pulmonary fibrosis.Respir Investig. 52(4): 227-235.






























