Clots on the Run
Lisa Jongbloed1 and Adriaan Dees1*
1Resident Internal Medicine, Ikazia Hospital, Netherlands
2Internist, Department of Internal Medicine, Ikazia Hospital, Rotterdam, The Netherlands
Submission: July 9, 2019; Published: July 22, 2019
*Corresponding author: Adriaan Dees, Dept. of Internal Medicine, Ikazia Hospital, Montessoriweg 1 3083 AN Rotterdam, Netherlands
How to cite this article: Lisa Jongbloed, Adriaan Dees. Clots on the Run.Curr Trends Clin Med Imaging. 2019; 2(5): 555615. DOI: 10.19080/CTCMI.2019.02.555615
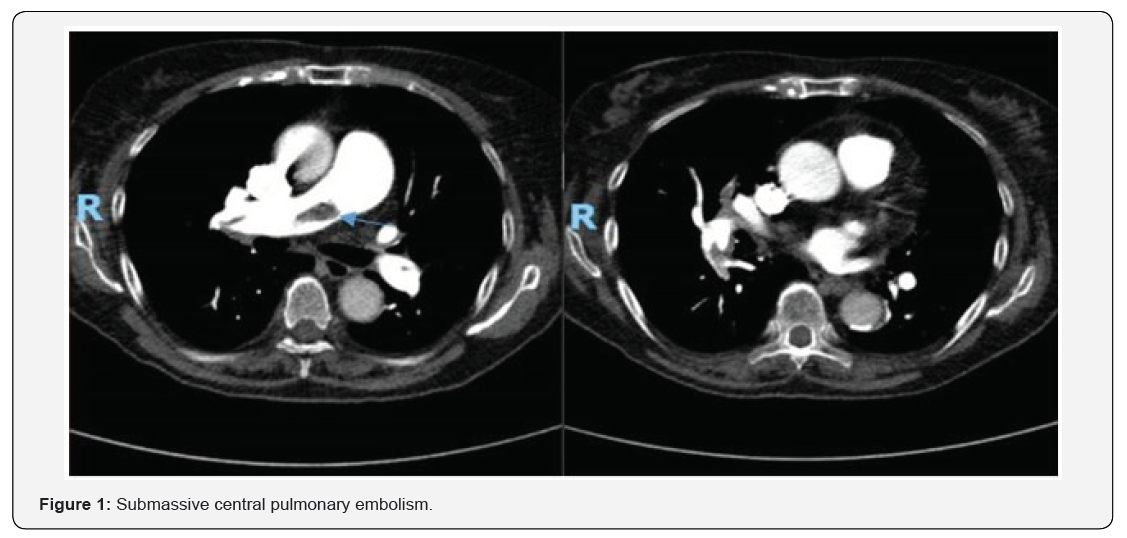
Opinion
An 86-year-old woman presented with severe dyspnea and pleuritic pain. She had a history of unprovoked pulmonary embolism and deep venous thrombosis eight years ago and was treated with acenocoumarol for 12 months. On admission, she was noted to have a blood pressure of 150/95 mm Hg and a pulse rate of 112 beats/min (regular). Arterial blood gasses: pCO2 was 30 mm Hg (normal 35 - 48 mm Hg), pO2 was 85 mm Hg (normal 75-100 mm Hg), HsTNT was 107 ng/l (normal 0-14 ng/l) and NT-proBNP was 240 pmol/l (normal <18 pmol/l). On CT-angiography, submassive pulmonary embolism at the bifurcation of the pulmonary arterial trunk was observed (arrow), in addition to peripheral emboli on both lung sides (Figure 1). She was observed in the intensive care unit because of the extensive spread of the clots. Initial treatment with low-weight heparin was followed by treatment with rivaroxaban, a factor X inhibitor [1]. The patient’s vital parameters, tachycardia in particular, improved and she was sent to the internal ward.
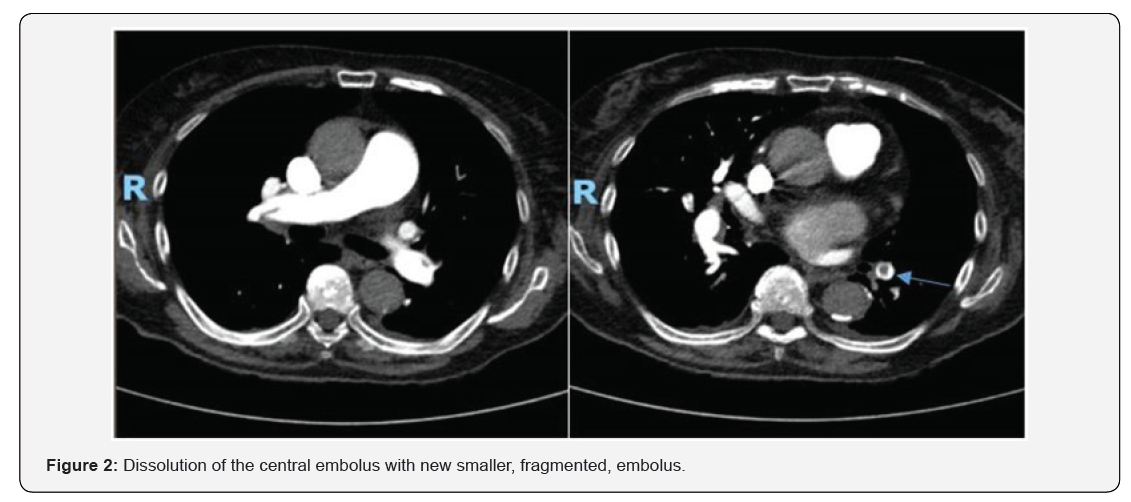
Three days after her initial presentation, she experienced new chest pain, that was mainly left -sided. Blood pressure, pulse rate and other controls remained unchanged. Because of the heaviness of her complaints, a new CT-scan was performed (Figure 2). The central embolus had disappeared; however, new small emboli were observed (arrow). The duration of complete resolution of pulmonary embolism (PE) is unknown. A study in which PE patients were evaluated by CT angiography scan after six weeks of therapy found that normalization occurred in 32 percent. In patients with atrial fibrillation, treated with rt-PA therapy, secondary thrombo -embolic complications due to incomplete thrombi dissolution have been described [2]. We next discuss the case. In hemodynamically stable patients, we do not routinely perform a second CT angiography or echocardiography to assess the dissolution of right heart or central pulmonary thrombus. The patient made a full recovery and was transferred to a nursing home.
References
- Van der Hulle T, Kooiman J, Den Exter PL, Dekkers OM, Klok FA, et al. (2014) Effectiveness and safety of novel oral anticoagulants as compared with vitamin K antagonists in the treatment of acute symptomatic venous thromboembolism: a systematic review and meta‐analysis. Journal of Thrombosis and Haemostasis 12(3): 320-328.
- Van Rossum AB, Pattynama PM, Ton ETA, & Kieft GJ (1998) Spiral CT appearance of resolving clots at 6 week follow-up after acute pulmonary embolism. Journal of computer assisted tomography 22(3): 413-417.






























