Vocalizer- An Interface
Sanjith Saseedharan1* and P Jagannath2
1Head- Department of Critical Care, India
2Senior Oncosurgeon, India
Submission: April 26, 2017; Published: May 24, 2017
*Corresponding author: Sanjith Saseedharan, Head- Department of Critical Care, SL Raheja, Raheja Rugnalaya Marg, Mahim West, Mumbai-400016, Maharashtra, India, Tel: +919004479549; Email: sanjith@rahejahospital.com
How to cite this article: Sanjith S, P Jagannath. Vocalizer- An Interface. Curr Trends Biomedical Eng & Biosci. 2017; 4(2): 555635. DOI: 10.19080/CTBEB.2017.04.555636. DOI: 10.19080/CTBEB.2017.04.555636
Abstract
Presently no interface exists for communication between a caregiver and a patient when the patient is unable speak due to some medical condition in which his cognition and understanding is retained. This leads to great irritation and discomfort to the patient and is a cause of concern for the caregiver. The vocalizer seems like an application which forms the vital link between the caregiver and the patient at this time of distress.
Keywords: Vocalize; Communication; Ventilator; Variables; Tablet
Discussion
A casual peep into an ICU for a layman is a disturbing rather a horrific site-patients with a number of tubes attached to their bodies, with tube penetrating into their mouth, a mask covering the entire face, etc. Yes they are on support systems, posttrauma, post-surgery etc. No doubt medical science has advanced to such an extent that such sophisticated technologies in an ICU can pull back a person knocking the door of the other world (death). However manya times these sophisticated support systems are retained as per the doctor's advice when patients are conscious, partly regaining their consciousness and becoming aware of their environment, regaining physical and mental wakefulness and having an urge to communicate. This is the most difficult and discomforting period for a patient in the ICU. Another category of patients are those that have undergone surgeries of the oral cavity, or supra major intrathoracic surgeries where they are not able to speak as a pipe is passed directly through the neck called as tracheostomy. Well technology does have a human side. It is indeed a technological marvel that such a situation can be eased and to put it humorously, a tubed, wired and gagged ICU patient can comfortably communicate about all his or her equipments and queries with a path breaking application called vocalizer.
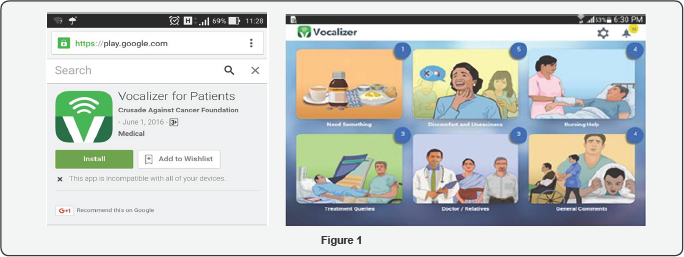
A period of 15 months and many man hours saw the development of the vocalizer (in the authors institute) which is freely available for download on a tablet from Google play store (Figure 1). To begin with, each patient who was on the ventilator or T piece or tracheostomised were questioned after they were shifted out of the ICU as to what they were trying to communicate to the caregivers. A set of 273 frequently asked questions (variables) were elucidated from the patients. Out of them 47 most frequent variables were taken up for representation on the app .The challenge was to make pictures of these apps that could be easily be recognized by any patient irrespective of social background, language and age. Hence easy to understand pictures were formed which were then rigorously tested individually with many patients. Moreover this picture was then coupled with an easy to hear voiceover in English and Hindi .This voice over could also be changed with respect to gender. At times the hand eye coordination may not be optimum and in the event that the picture pointed to at was not right the voice over prompt would help to ask the patient whether it was the same variable he/she wished to select. Over and above, if the patient had something to tell us from any of these pictures the said picture/variable would get marked and remained on the task bar.
This could be deleted after the task was done by the nurse. The first screen that opens up shows
i. Need something
ii. Discomfort and uneasiness
iii. Nursing help
iv. Treatment queries
v. Doctors/relatives
vi. General comments
Each of these commands would further open up to the variables as shown below
A. Need something
i. I want water
ii. I need food
iii. Please give my medicines
iv. I need my spectacles
v. I want tea /coffee
vi. I want a writing pad
vii. I need my mobile phone
viii. Can I have a newspaper/book to read
ix. I am feeling hot, need a fan.
B. Discomfort and uneasiness
a. I can't speak
b. I can’t breathe
c. I have pain
d. I am feeling itchy
e. My hand is swollen
f. I am not able to pass urine
g. My back hurts
h. Please turn me to the left
i. Please turn me to the right
C. Nursing help
a. Remove/ wipe secretions from my mouth
b. I want to pass motion
c. Please raise my head
d. I am feeling cold
e. I have passed motions please clean me
f. Stay here, I’m scared
g. IV hurts. Help
h. Nose tube is irritating .Help
D. Treatment queries
a. How was the operation
b. Are the reports ok?
c. When is the discharge?
d. Why are you taking blood?
e. Why are you giving blood?
f. Why does physiotherapy hurt?
When will I be shifted to the ward
E. Doctor/Relatives
a. I want to speak to the doctor
b. I want to speak to my wife/husband
c. Call my relatives
d. When will I become ok?
e. I need something else*
*I need something else: This command opens a type board in which the patient can easily type in large alphabets what he wishes to convey which can thus be easily read by the caregiver. In the absence of this feature the patient attempts to write on a writing pad and very often the handwriting is hardly discernible due to the difficult position in which the patients write, parallax of vision, and weakness due to which the patient is in the ICU.
F. General comments
a. I want to sleep
b. No sleep last night
c. Too noisy, can't sleep
d. Want to go home
e. Why are you not feeding me?
f. What is the time?
g. I am hungry
h. I am fine
i. Please witch off the light.
Where will this application be extremely useful?
a) Patients who have undergone tracheostomy for some oropharyngeal surgery and hence are unable to speak.
b) Patient who have been put on an invasive form of ventilation due to
a. Neuromuscular problems like GBS/Myasthenia Gravis
b. Post operatively due to some elective surgery which may require prolonged ventilation
c. In recovery room post anesthesia when patient is going to removed off the ventilator in a few hours.
Oncology Canters with high volume of surgeries requiring tracheostomies will benefit maximum with this application and will serve as a good help to the caregiver. Intensive care units dealing with high volumes of post op cases and neuromuscular cases will benefit with this application.
Where this application cannot be used
1. When patient is incoherent, drowsy and not responsive to commands
2. Agitated patient
3. Blind patient
Even in a patient who cannot operate the device voluntarily the set of questions can be pointed to by the caregiver which can be nodded to by the patient and thus in a systematic manner all of the patients requests can be heeded to.
Benefits
a) Patient feels secure that all his wishes and requirements are getting addressed
b) Since all his requirements are getting addressed he does not get agitated and hence the requirements of sedation in the ICU reduce and the patient usually does not get into a state of ICU delirium.
c) Patient gets an overall sense of satisfaction
d) Relatives rest assured that his requests are getting heeded to.
e) Patient- doctor- nurse interaction increases thus instilling confidence in the treatment provided and makes the doctor satisfied that he is able to understand the problem of the patient.
On which interface this would work best:
a) This app works best with a tablet interface as the figures are seen big and easily. Big figures help the patient to point to it without problem
b) This app could also be used on a large mobile LED which could be wheeled in front of the patient
c) This could also be downloaded on a Smartphone. However this interface may be slightly difficult to use as pointing to the figure may require finer movements which may be difficult for a sick and weak patient.
Further vision
a) To couple the commands to a mobile phone this will be received by the caregiver as a message
b) Fine tune the application with more commands in the next few years.
c) Couple it with videos of procedures and explanation in written format of procedures that the patient has undergone or going to undergo.
Benefits observed by the author during the use of this app
Patients feel more comfortable pre and post intensive care. Doctors and caregivers are not rendered helpless as we are able understand what the patient wishes to convey. Patients go into surgeries with confidence and no fear of the post-operative stay.
Conclusion
It is of the authors opinion that the device should be a part of every hospital as this does get care where it is needed in an area that has long been neglected, an area that demands compassion and empathy. A whole gamut of information, requirements, discomfort, wishes etc of the patient on a ventilator is taken care of by this application. A thorough research has gone into the various situations that doctors and caregivers inside an ICU face while handling such conscious patients. This is comforting not only to the patient but also to the caregivers who can now be assured that they have precisely understood such patients' wants and requirements. It helps to dissolve the frustrations of both the cared and the caring. Apart from all the research technique medicines, medical procedures etc. that go into treating a critically ill patient a patients response and mental satisfaction which comes from prompt and careful nursing and caregiving goes along way in achieving a patients whole hearted participation in prognosis and treatment and wellness. The vocalizer does this part!!!!
Acknowledgement
Tata interactive has been closely associated in the development of the application.
Conflicts of Interest
i. SanjithSaseedharan-Holds the copyright for the application.
ii. Edwin Pathrose-No conflict of interest.
iii. P Jagannath-Co-holder of copyright for the application.






























