ILD-PH: a real world diagnosis with lung function and treatment approach
Parthasarathi Bhattacharyya1*, Mintu Paul2, Sayoni Sengupta3, Dipanjan Saha3, Aniruddha De4, Sayanti Karmakar3, Nandini Biswas1, Pawan Agarwal1, Dhiman Ganguly1 and Devanu Ghosh Roy4
1Consultant Pulmonologist, Kolkata, India
2Research Assistant, Institute of Pulmocare and Research, Kolkata, India
3Research Fellow, Institute of Pulmocare and Research, Kolkata, India
4Consultant cardiologist, Kolkata, India
Submission: October 22, 2024; Published: November 22, 2024
*Corresponding author: Parthasarathi Bhattacharyya, Consultant Pulmonologist, Institute of Pulmocare & Research, Kolkata, India
How to cite this article: Parthasarathi B. ILD-PH A real world diagnosis with lung function and treatment approach. Anatomy Physiol Biochem Int J: 2024; 7(4): 555720. 10.19080/APBIJ.2024.07.555720.
Abstract
Background: PH (pulmonary hypertension) in ILD (interstitial lung disease) affects the functionality, quality of life survival adversely. Most often, the patients remain untreated for lack of right heart catheterization and a published recommendation. Hence, an alternate exercise to decide PH-specific therapy in ILD is welcome.
Methods: Stable Symptomatic ILD patients having PH diagnosed on clinico-radio-echocardiographic evaluations were selected. The willing patients having “DLCO-FVC distance≥30” (percentage-predicted values) were given option to receive grading dose of sildenafil or tadalafil in an open, prospective, real-world protocol. We assessed the impact in terms of 2-Chair-Test parameters and CAT score at the first follow up visit.
Results: Sixty-nine patients qualified for treatment, but 32 of them did not opt for it. The qualified-treated group (n=37) differed significantly with lower value of baseline SpO2 (p=0.01), minimum SpO2 after exercise (p=0.006), degree of de-saturation (p=0.04), the systolic echocardiography measured PAP (p=0.004), DLCO (p=0.0001), FVC/DLCO (p=0.004) but not in the FVC-DLCO distance from the qualified-untreated group (n=32). Post treatment, (120.7±86.33 vs. 182.5±156.9 days); the treated group showed improvement in all the measurements as baseline heart rate (p=0.08), maximum pulse rate (p=0.27), health status (CAT-score) (p=0.0001), baseline SpO2 ((p=0.21), minimum SpO2 (0.001), and desat-max (0.0004). There was general worsening in all these parameters including significant worsening in baseline SpO2 (p=0.04) in the untreated group. The non-qualified patients (n=32) showed no difference in status on follow up for 130.9±105.8 days.
Conclusion: The FVC-DLCO distance guided strategy to treat ILD-PH appears potentially prospective. Relatively sicker patients tended to opt vasodilator therapy.
Key words: ILD; Pulmonary Hypertension; DLCO; FVC; 2 Chair Test
Abbreviations: ILD: Interstitial Lung Disease; PH: Pulmonary Hypertension; PAH: Pulmonary Arterial Hypertension; CAT: Copd Assessment Test; 2CT: 2 Chair Test; PAP: Pulmonary Artery Pressure; RHC: Right Heart Catheterization; TPG: Transpulmonary Gradient; PVR: Pulmonary Vascular Resistance; PDE5: Phosphodiesterase-5; SpO2: Arterial Oxygen Saturation; PERR: Post-Exercise Recovery Response
Introduction
Pulmonary hypertension (PH) can develop in ILD (interstitial lung diseases) patients as a complication. The prevalence of such PH referred to as ILD-PH can be frequent depending on the definition, the underlying etiology of PH, the severity of ILD, and the mode of diagnosis of PH [1-3]. PH in ILD imparts an adverse impact on a patient’s functional capacity, health related quality of life, supplemental oxygen demand, risk of hospitalization, and the survival prospect [4,5]. The treatment of ILD-PH patients with supplemental oxygen and/or diuretics is accepted. But, the role pulmonary vasodilators for their treatment remains inconclusive and often controversial [6]. Several PH-specific treatment trials with different classes of pulmonary vasodilators are published and reviewed [7]. There were both positive and negative results and sometimes even deleterious outcome as increased hospitalization or clinical worsening. [8-16]. The PDE5 inhibitor, sildenafil showed hope in some trials [8,9,13-15] and, lately, the trial with parenteral treprostinil was encouraging [17]. Finally, the recent publication of the results of INCREASE trial showed both reduction in clinical worsening and disease progression with functional improvement (6-minute walk distance) using inhaled treprostinil in ILD-PH compared to placebo [18].
The real world of diagnosis and treatment of ILD is burdened with significant logistic constraints in India [19]. The gold-standard diagnostic evaluation for PH, the right heart catheterization, is often not accessible or feasible. Hence, in the patients of ILD-PH, PH remain mostly unidentified allowing the patients to suffer progressively and relentlessly. Therefore, framing an objective and effective mode of diagnosis of ILD-PH without subjecting the patients to right heart catheterization is both difficult and daunting. Furthermore, advocating treatment with pulmonary vasodilators demands extra caution and evidence for ethical acceptance. Here, in the manuscript, the authors have presented an observation of diagnosing and treating ILD-PH in real-word on a rational and consensus endorsed approach with PDE5 (phosphodiesterase-5) inhibitor.
Materials and Methods
p>The real world protocol was approved by the Institutional Ethics Committee of the Institute of Pulmocare and Research, Kolkata and was subsequently enrolled in clinical trial registry of India (CTRI number-CTRI/2015/07/005962). The study was also endorsed by a consensus decision of the PH group, Kolkata been formed of a few physicians from the related fields showing interest in treatment and research of PH. The group engaged and forwarded an approach of identifying and treating ILD-PH in situations of logistic constraints when a right heart catheterization deems impossible or not feasible.
Utilizing the clinico-radio-echocardiographic algorithm of diagnosis of PH by the institute [20], the group evolved an effective strategy to treat ILD-PH with a PDE5 inhibitor (sildenafil or tadalafil) through a consensus decision using information from spirometry and DLCO. The method included:
Diagnosis of ILD and basic physiological evaluations: The diagnosis of ILD was accomplished with joint opinion of at least two experts (a radiologist and a pulmonologist) on high-resolution computerized tomography (HRCT) pictures of thorax in clinic-radiologically (chest-x-ray) suspected patients. Spirometry with estimation of DLCO was done in all observing the standard norm of performance.
Diagnosis of PH: The diagnosis of PH was achieved through exercising the institute’s clinico-radio-echocardiographic criteria-based PH identifying algorithm [20].
Determination of post exercise recovery response by 2 chair test: A single expert technician performed all the 2-Chair Tests [2CT]. This test has been developed by the institute to assess the post-exercise recovery response (PERR) uniformly in patients with various respiratory diseases [21]. The test can be performed in patients with chronic lung diseases observing defined inclusion and exclusion criteria and provision of flexibility. This desat-max or the maximum de-saturation in the post exercise period is seen to correlate best with the perceived sickness by the patient (unpublished data). Concomitant recording of the CAT (COPD assessment test) score was a routine practice in all the visits.
Selection of patients for anti-PH treatment: Any patient of having ILD with PH on the clinico-radio-echocardiographic criteria underwent spirometry and the measurement of the diffusion capacity as per standard recommendation of regular evaluation of ILD. We noted the percentage-predicted values of their FVC (forced vital capacity) and the adjusted diffusion capacity (measured in the same sitting). Those who showed a FVC-DLCO distance to be ≥30 were considered eligible by the consensus opinion of the members of the PH group for treatment with a pulmonary vasodilator. Patients unwilling to undergo pulmonary vasodilator therapy for any reason, those having any other concomitant lung disease or any significant systemic problem, and patients with obvious contraindication or known intolerance for PDE5 inhibitors were excluded at this stage.
Specific anti-PH treatment: Only the willing and the qualified (FVC-DLCO distance ≥30) patients for vasodilator therapy were prescribed an oral PDE5-inhibitor as sildenafil (10 mg thrice daily) or tadalafil (10 mg once daily) to start with and on toleration, doubling the dose after 5 to 7 days and subsequently continuing it. The patients were informed about the adverse reaction of the drug before prescription and they were requested to report any obvious or suspected adverse reactions. Stand by provision of oxygen supplementation was a universal pre-requisite to start such treatment. Oxygen supplementation was advised to keep SpO2>90% in case of any observed desaturation (SpO2<90%) with any activity or in the 2-chair test.
The follow-up plan: The patients were instructed to follow up at least once every 12 weeks or/and whenever necessary without any prescribed follow-up schedule. At each follow up, the 2CT was repeated along with CAT (COPD assessment test); a repeat echocardiography, though suggested at least after 3 months, was not made mandatory.
The statistical calculations were done after recording the status at the first follow up visit; the statistical exercise included unpaired Student’s ‘t tests’ for intergroup comparison between the qualified treated and the qualified but not treated groups and the former with the disqualified group at the beginning. Further paired ‘t-test’ was applied for intra-group comparison separately for all the groups of subjects comparing the initial and the final follow up measurements of the 2-chair test variables (baseline pulse rate, maximum pulse rate, baseline SpO2, maximum SpO2, and the desat-max or maximum de-saturation) and CAT score.
Results
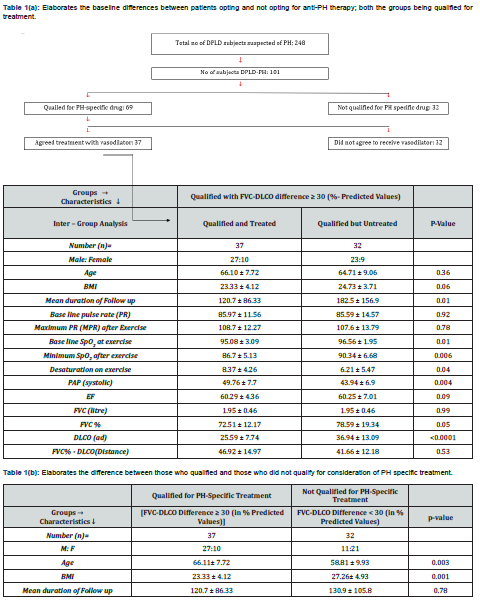
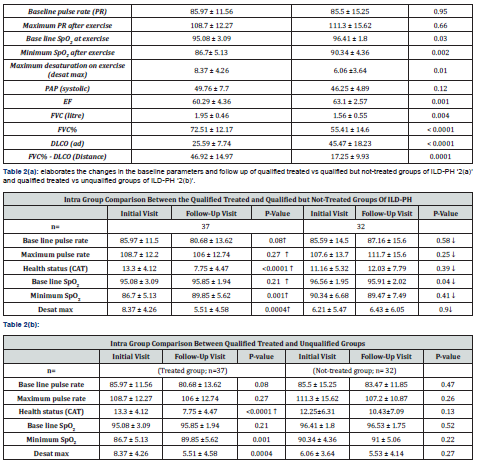
Sixty-nine out of 109 subjects qualified but finally 37 out of them agreed for treatment. The comparison between the qualified and treated vs. qualified and untreated patients in terms of demography, lung function (spirometry and DLCO), echocardiography, CAT score, and 2 chair test parameters are shown in (Table 1). The change from the baseline values in the same parameters (2CT-variables and the CAT score) were noted in intra group comparison following treatment (Table 2).
The common adverse effects of the treated patients (compared to the qualified but not treated patients) were pedal swelling (18.92% vs. 6.25%), headache (13.52% vs. 3.12%), reduced appetite (10.81% vs. 6.25%), weight loss (8.11% vs. none), and muscle cramps 5.40 % vs. none). The latter group (qualified, not-treated patients), however, had higher sleeplessness (6.25% vs. 2.70%), itching (9.37% vs. 2.70%) and facial puffiness as (6.25% vs. 2.70 %). Weakness (12.5%), weight loss (12.5%), loss of appetite and constipation (both 9.37%) were the common side effects of those who did not qualify for treatment. The common comorbidities of both the groups were diabetes, hypertension, and hypothyroidism.
Discussion
The results show interesting revelations. The qualified- treated group (n = 37) had significantly lower DLCO [(25.59±7.74 vs 36.94±13.09; p=0.0001)] and lower %-predicted FVC [(72.51±12.17 vs 78.59±19.34; p=0.05)]. This made their FVC-DLCO distance significantly higher [(46.92±14.97 vs. 41.66±12.18; p=0.53)] and the same happened to the FVC/DLCO ratio [(2.81±1.51 vs. 2.27±0.54; p=0.004] compared to the qualified but unwilling for vasodilator treatment group [(FVC-DLCO difference>30%) group; (n=32)] (Table 1). The age and the BMI of the treated patients were similar to those refusing treatment.
The treated group was worse compared to those not qualifying the treatment (Table 2). They had higher age (p=0.003), lower BMI (P = 0.001), lower base line saturation before exercise (p=0.03), minimum saturation after exercise (p=0.002), lower FVC (p=0.004), lower ejection fraction (p=0.001), and lower DLCO (25.59±7.74 vs. 45.47±18.23; p<0.0001) with higher FVC-DLCO distance (46.92±14.97 vs. 17.25±9.93; p=0.0001) (Table 2).
The intragroup analysis after treatment reveals the global positive changes in the treated group reflected in baseline pulse rate (p=0.08), minimum post-exercise SpO2 (p=0.001) and degree of de-saturation (desat max) (0.0004) while the qualified but untreated group had global worsening with significant reduction in baseline SpO2 (p=0.04) (Table 1).
The planning and execution of the study was done much before the publication of the majority of the vasodilator trials in ILD-PH. Hence, we adopted the mean pulmonary artery pressure (mPAP) value >25mm of Hg satisfying old definition of PH. ILD happens to be a common etiology of Group-3 PH and compared to the other members of the group, it shows the worst survival [22]. The development of PH in ILD appears ominous.
Highly predictive radiological features of PH in chest x-ray [23] can support the clinical suspicion of PH. In CT/HRCT chest, the ratio of the diameter of pulmonary trunk to the adjacent aorta may turn ≥1 [24] and the same between pulmonary artery branch diameter and the accompanying bronchus [25] appearing ≥1 (more than one) in three or more lobes strongly indicates presence of PH. Our clinic-radio-echocardiographic mode of diagnosis of PH included these features with supportive evidences by echocardiography to diagnose PH [20]. We could not use the gold-standard hemodynamic criteria for PH from right heart catheterization (RHC) for obvious real world reason. RHC, in our real world, is rarely practiced; hence, to outwit the problem, we evolved a clinico-radio-echocardiographic mode for diagnosis of PH [20] and innovated separate treatment strategies for COPD-PH and ILD-PH. The strategy on COPD-PH was based on maximum de-saturation in 2CT [26] and for ILD-PH, we endorsed an idea of offering PH-specific treatment based on an indirect assessment of the impact of PH. ILD-PH patients are often observed by physicians helplessly deteriorating with development of cor-pulmonale. A treating physician finds himself trapped in the crossfire of conscience and the quest of evidence with having no RHC data to decide treatment of PH.
Both FVC (forced vital capacity) and DLCO are affected in both PH and ILD; however, PH primarily does not influence the FVC. In ILD without PH, the DLCO is expected to correlate and move somewhat parallel to the FVC, a marker of restriction been produced by tissue fibrosis. However, the DLCO is expected to fall ‘disproportionately’ from aco-presence of PH in ILD. This is endorsed in IPF with FVC over 70% of predicted where a DLCO<30 % suggests a higher prevalence and greater severity of PH than patients with DLCO>30% [27]. Since DLCO has been found to be the best individual prognostic marker in IPF, the co-presence of PH in ILD is likely to contribute to such poor survival [28].
Significant correlations between FVC/DLCO (in %-predicted values) and the level of systolic and mean PAP (pulmonary artery pressure) have been found (p<0.05) [29]. The FVC/DLCO ratio has been regarded as a marker of presence of pulmonary hypertension by some authorities. In patients with systemic sclerosis associated PH, a ratio >1.91 was found 87.5 % sensitive and 100 % specific for the presence of PH [30]. When calculated, in our patients show a mean FVC/DLCO ratio of 2.81 (far above 1.91) signifying obvious co-presence of PH. Therefore, on consensus, we decided a cut-off mark of FVD-DLCO distance as ≥ 30% as ‘disproportionate’ reduction of DLCO to qualify for PH-specific treatment. Further, the consensus allowed us to monitor these patients for the effect of treatment with the 2-Chair Test. We have forwarded this novel test of post-exercise recovery response (PERR) as a tool to assess the functional jeopardy of cardiopulmonary reserve [25]. We have noticed that the desat-max in 2CT remained the best parameter to appreciate the degree of sickness (unpublished data). The highly significant improvement observed in the post exercise saturation with treatment even with the relatively small sample size is encouraging despite the lack of RHC data.
The lung disease related PH (PH developing as a complication of a chronic lung disease) is marked by protracted hypoxia from a primary reduction in the respiratory reserve (ventilation and /or diffusion capacity) along with a concomitant and subsequent reduction in circulatory reserve leading to the development of PH as a secondary phenomenon. The cumulative effect of the depletion of both the reserves determines the physiological impact and the symptomatology. Since the pathology in ILD is usually likely to reverse very little in most of the cases and the PH imparts deleterious effects on the right ventricle, the treatment of pulmonary hypertension on objective basis should be explored. We pursued decision policy within initiation of a PDE5 inhibitor (sildenafil/ tadalafil) since they have been tried already [8, 9, 13, 14]. The scaling up of the dose was done to avoid the chance acute pulmonary vasodilatation induced worsening of ventilation-perfusion (V/Q) mismatch leading to clinical worsening. The maintenance of a fixed dose in our experience, though small, is rewarding. The modification of dose with repeat assessment of the FVC-DLCO could have been better.
The treatment efforts of ILD-PH with PH specific drugs especially the PDE5 inhibitors have yielded mixed results with hope [8,9,13,14]. Randomized trial with bosentan was a failure [10]. The ARTEMIS-IPF trial with ambrisentan was terminated early for increased disease progression and hospitalization in the ambrisentan group of the randomized controlled trial compared to placebo [12]. In the STEP-IPF trial, sildenafil was tried in IPF and it showed slower decline in 6MWD and improvement in quality-of-life measurements in a subgroup of patients [13,14]. Similarly, a randomized riociguat trial (RISE-IIP) was unsuccessful [15]. Amidst the negative scenario, parenteral treprostinil was found associated with increased 6MWD, RV function, and hemodynamics in ILD-PH (mPAP>35mm) [17]. Recently, inhaled treprostinil has shown a great promise in treating ILD-PH in INCREASE trail [18] that revealed improvement in 6MWD (six minutes and reduction in the clinical worsening with other positive effects including improvement in lung function.
The weaknesses are many folds. They include the relatively small number patients, the lack of hemodynamic data from RHC (right heart catheterization) and the lack of assessing the dynamics of FVC-DLCO following treatment. The echocardiographic information could have been more inclusive especially with right ventricular functional assessments with TAPSE (Tricuspid Annular Plane Systolic Excursion), right ventricular E/e and the free wall GLS (global longitudinal strain) of right ventricle. A more holistic assessment with inclusion of repeat echocardiography, and change in parameters as quality of life and 6MWD would have been better. The duration of follow up was not uniform for the real world reasons. The dynamics of decline of both the parameters (FVC and DLCO) may be different in different etiologies, nature (predominantly fibrotic or not), and at different stage of ILD. Hence, the FVC-DLCO distance may not be applicable in advanced and predominantly fibrotic ILD where FVC may reduce significantly. Despite the shortcomings, we feel that the novelty of the approach needs attention and criticism. Subject to validation and modification with further research, the philosophy may find place in future in the diagnostic work up and/or treatment decision of the ILD associate PH especially in resource poor situations.
Conclusion
It appears that in selected situation, ILD-PH can be identified with lung function (spirometry and DLCO) alone and such PH may qualify treatment based on relatively disproportionate reduction of DLCO compared to FVC. Further research is warranted with hemodynamic endorsement of the approach.
Acknowledgements
Indranil Haldar, Santanu Dutta, Sushmita RoyChowdhury, Subhendu Mondal, Shuvanan Ray, Mr. Madan Sarma, Ms. Ratna Dey, Mrs. Malobika Pandit, Mrs. Eti Dutta of Institute of Pulmocare and Research.
References
- Shlobin OA, Brown AW, Nathan SD (2017) Pulmonary hypertension in diffuse parenchymal lung diseases. Chest 151(1): 204-214.
- Andersen CU, Mellemkjær S, Hilberg O, Kudsk JEN, Simonsen U, et al. (2012) Pulmonary hypertension in interstitial lung disease: prevalence, prognosis and 6 min walk test. Respiratory medicine 106(6): 875-882.
- Ryu JH, Krowka MJ, Swanson KL, Pellikka PA, McGoon MD (2007) Pulmonary hypertension in patients with interstitial lung diseases. Mayo Clinic Proceedings 82(3): 342-350.
- Klinger JR (2016) Group III pulmonary hypertension: pulmonary hypertension associated with lung disease: epidemiology, pathophysiology, and treatments. Cardiol Clin 34(3): 413-433.
- Nathan SD, Barbera JA, Gaine SP, Harari S, Martinez FJ, et al. (2019) Pulmonary hypertension in chronic lung disease and hypoxia. Eur Respir J 53(1): 1801914.
- King CS, Shlobin OA (2020) The Trouble with Group 3 Pulmonary Hypertension in Interstitial Lung Disease: Dilemmas in Diagnosis and the Conundrum of Treatment. Chest 158(4): 1651-1664.
- Szturmowicz M, Kacprzak A, Kuś J (2017) Pulmonary hypertension in diffuse parenchymal lung diseases - is there any benefit of PAH-specific therapy? Adv Respir Med 85(4): 216-223.
- Collard HR, Anstrom KJ, Schwarz MI, Zisman DA (2007) Sildenafil improves walk distance in idiopathic pulmonary fibrosis. Chest 131(3): 897-899.
- Corte TJ, Gatzoulis MA, Parfitt L, Harries C, Wells AU, et al. (2010) The use of sildenafil to treat pulmonary hypertension associated with interstitial lung disease. Respirology 15(8): 1226-1232.
- Corte TJ, Keir GJ, Dimopoulos K, Howard L, Corriset PA, et al. (2014) Bosentan in pulmonary hypertension associated with fibrotic idiopathic interstitial pneumonia. Am J Respir Crit Care Med 190(2): 208-217.
- Prins KW, Duval S, Markowitz J, Pritzker M, Thenappan T (2017) Chronic use of PAH-specific therapy in World Health Organization Group III Pulmonary Hypertension: a systematic review and meta-analysis. Pulmonary circulation 7(1):145-155.
- Raghu G, Behr J, Brown KK, Egan JJ, Kawut SM, et al. (2013) Treatment of idiopathic pulmonary fibrosis with ambrisentan: a parallel, randomized trial. Annals of internal medicine 158(9): 641-649.
- Network IPFCR, Zisman DA, Schwarz M, Anstrom KJ, Collard HR, et al. (2010) A controlled trial of sildenafil in advanced idiopathic pulmonary fibrosis. New England Journal of Medicine 363(7): 620-628.
- Bhattacharyya P, Bhattacherjee PD, Maji S, Chatterjee S, Paul R, et al. (2014) Role of Sildenafil in treating Pulmonary Hypertension in COPD patients. The Pulmoface 1(2): 3.
- Han MK, Bach DS, Hagan PG, Yow E, Flaherty KR, et al. (2013) Sildenafil preserves exercise capacity in patients with idiopathic pulmonary fibrosis and right-sided ventricular dysfunction. Chest 143(6): 1699-1708.
- Nathan SD, Behr J, Collard HR, Cottin V, Hoeper MM, et al. (2019) Riociguat for idiopathic interstitial pneumonia-associated pulmonary hypertension (RISE-IIP): a randomised, placebo-controlled phase 2b study. The Lancet Respiratory Medicine 7(9): 780-790.
- Saggar R, Khanna D, Vaidya A, Derhovanessian A, Maranian P, et al. (2014) Changes in right heart haemodynamics and echocardiographic function in an advanced phenotype of pulmonary hypertension and right heart dysfunction associated with pulmonary fibrosis. Thorax 69(2):123-129.
- Waxman A, Jaramillo RR, Thenappan T, Ravichandran A, Engel P, et al. (2021) Inhaled treprostinil in pulmonary hypertension due to interstitial lung disease. N Engl J Med 384(4): 325-334.
- Bhattacharyya P, Mukherjee S, Mukherjee A, Paul M, Handa A, et al. (2022) Etiological profile and evaluation of ILD in real-world: the perceived impression of the ILD treating doctors in India. J Assoc Chest Physicians 10: 75-80.
- Bhattacharyya P, Sengupta S, Saha D, Paul M, Choudhury P, et al. (2020) Group III Pulmonary Hypertension: relative frequency of different etiologies in a referral pulmonary OPD. J Assoc Chest Physicians 8(2): 69-75.
- Bhattacharyya P, Saha D, Paul M, Ganguly D, Mukherjee B, et al. (2020) Two chair test: a substitute of 6 min walk test appear cardiopulmonary reserve specific. BMJ Open Respiratory Research 7(1): e000447.
- Prins KW, Rose L, Archer SL, Pritzker M, Weir EK, et al. (2018) Disproportionate Right Ventricular Dysfunction and Poor Survival in Group 3 Pulmonary Hypertension. Am J Respir Crit Care Med 197(11): 1496-1499.
- Kenemoto N, Furuya H, Etoh T, Sasamoto, H, Matsuyama S (1979) Chest roentgemgram in primary pulmonary hypertension. Chest 76(1): 45-49.
- Tan RT, Kuzo R, Goodman LR, Siegel R, Haasler GR, et al. (1998) Utility of CT scan evaluation for predicting pulmonary hypertension in patients with parenchymal lung disease. Chest 113(5): 1250-1256.
- Greiner S, Jud A, Aurich M, Hess A, Hilbel T, et al. (2014) Reliability of noninvasive assessment of systolic pulmonary artery pressure by Doppler echocardiography compared to right heart catheterization: analysis in a large patient population. Journal of the American Heart Association 3(4): e001103.
- Bhattacharyya P, Sengupta S, Bhattacharjee PD, Ganguly D, et al. (2018) Post exercise desaturation can help identifying treatment responders of COPD pulmonary hypertension in real world: an appraisal. J Pulm Respir Med 8(469): 2.
- Sharp C, Adamali HI, Millar AB (2017) A comparison of published multidimensional indices to predict outcome in idiopathic pulmonary fibrosis. ERJ open research 3(1): 00096-2016.
- Hussein AAM (2017) Evaluation of FVC/DLCO ratio as a predictor for pulmonary hypertension in patients with interstitial lung diseases. European Respiratory Journal 50(suppl 61): PA861.
- Donato L, Elisiana CG, Giuseppe G, Pietro S, Michele C, et al. (2017) Utility of FVC/DLCO ratio to stratify the risk of mortality in unselected subjects with pulmonary hypertension. Intern Emerg Med 12(3): 319-326.
- Riad NM, Morshedy NA, Shoukri AM. (2015) Role of pulmonary function tests in screening pulmonary arterial hypertension in scleroderma. Egyptian Journal of Bronchology 9: 287-292.






























