Abstract
Background: In pediatric emergency care, accurate diagnosis is critical for the desired treatment. Systemization of clinical pathology and imaging might lead to higher accuracy of diagnoses in various diseases of children.
Objective: The study aims to evaluate the feasibility of clinical pathology and imaging protocol regarding diagnostic accuracy in pediatric emergent disorders and corresponding age and condition performance.
Methodology: The cross-sectional study involved a single centre excluding patients<18 years old without needing diagnostic imaging. Age group and conditions, sensitivity, specificity, Positive Predictive Value (PPV), and Negative Predictive Value (NPV) were also determined. Patient data were extracted from patients’ charts, initial core application biomarker assays, and radiologic results and confirmed with comparison to their clinical records.
Results: The protocol was 87% sensitive in general and 92% specific, although sensitivity remained constant across ages while specificity was slightly higher in the oldest children. The protocol proved especially useful in identifying crucial conditions that require immediate action; meningitis had the highest sensitivity of 93%.
Conclusion: This study provides evidence for using integrated diagnostic protocols in pediatric emergency care, and newer adaptation strategies may even build the capacity for more precise diagnosis. The authors also suggest multi-centre trials and further changes to its age-dependent markers to ensure the high accuracy of the method in other clinics.
Keywords:Pediatrics; Imaging; Emergency; Biomarkers
Abbreviations:PPV: Positive Predictive Value; NPV: Negative Predictive Value; PECs: Pediatric Emergency Cases; ITP: Immune Thrombocytopenic Purpura
Introduction
Early diagnosis in pediatric emergency departments is the key to enhancing patient outcomes and optimizing resource use. Due to the nature of emergency department work as a fast-paced setting with high-stakes patients, accurate and swift diagnosis is often required. Children’s signs and symptoms may sometimes mimic other disease stages that are not severe enough to warrant emergency care. This is well grounded in current studies by prospective diagnostic analysis, which points to the strong influence of diagnostic accuracy and can be improved by systematic configurations of identifying symptoms for pediatrics emergency cases [1].
The diagnostic process in pediatric practice is quite challenging because children cannot express their symptoms and rely on clinical and laboratory tests. This reliance highlights clinical diagnosis as a branch that greatly supports identifying the biomarkers or pathogens or any other aspect related to children’s health [2]. The participation of clinical pathology assessments as a track in the diagnosis procedures in an emergency has enhanced the diagnostic decision of the associated diseases since the clinical pathology assessments yield fast results that either affirm or negate the possibility of the disease. Specifically, in pediatric emergency care, patients by conditions have seasonal variations and prevalence of typical diseases when accuracy in diagnostics may call for immediate further treatment and adequate therapy [3]. For instance, cases of respiratory infections during winter compel the health care personnel to distinguish between viral and bacterial causes as their management is different. In these terms, diagnostic audits are defined as assessing, verifying, and attesting the practice reliability of practice to ensure appropriate zone development and the approaches towards diagnosis-making in zones [4].
This research will be carried out with specific reference to diagnoses peculiar to pediatric emergency care due to the belief that structured audits and evaluations can only improve diagnosis accuracy. Based on these findings, certain changes can be made to future protocols that could better integrate diagnostic processes with known effective practices and contribute to evolving diagnosis for children in emergency settings to further the patient and provider’s betterment. Thus, this research aims to identify commonly used diagnostic patterns for child patients, evaluate the accuracy of these diagnoses using clinical pathology criteria, and identify the potential for systematization of these concepts for enhancing pediatric emergency care.
Literature review
The issue of diagnostic accuracy in Pediatric Emergency is a significant concern since children can have so many atypical presentations, which hinders accurate diagnosis of their conditions. Specifically, contemporary research underscores diagnostic uncertainty and variability inherent to emergency pediatric care with the potential for diagnostic lag or diagnostic [5,6]. Studies have confirmed that using image and clinicpathological data has better diagnostic accuracy, improving the treatment benefits to the patients. For instance, a descriptive cross-sectional survey of diagnostic disagreement in an urban Emergency department revealed that 50.5% of absolute interprofessional diagnostic disagreement was associated with clinically significant management changes, where emergency physicians increased morbidity in 10% of cases because of misdiagnosis at first instance [5]. Such findings stress the need to deploy diagnosis imaging optimally to make correct diagnoses and manage emergency conditions in children [5].
Guidelines based on clinical pathology protocols develop a framework for systematically analyzing diagnostic strategies in pediatric practice, primarily when these guidelines are used in conjunction with imaging. Biomarkers, which are biological measurements that provide information about the physiological state of a body, together with markers of infection, provide essential information in diagnosis that physical examination does not give, leading to a correct diagnosis [7]. These guidelines, particularly useful for highly charged conditions including but not limited to pediatric emergency departments, underline the importance of credible diagnostic standards that are readable and relevant for pediatric patients. Whiting et al. pointed out that due to the inadequacy of exact biomarkers, particularly in children, many diagnosticians in emergency care are imprecise, hence the importance of protocolization. Because clinical pathology guidelines establish consistent diagnostic practice, the practice eliminates inconsistencies and improves diagnostic accuracy, which improves patient care [8].
Audits are potent tools for assessing diagnostic competency, particularly in emergency departments, which are characteristically liable to diagnostic mistakes. In pediatric emergency departments, audits enable the evaluation of compliance with guidelines, variability in diagnosis, and sources of blame. Research shows that scheduled audits in children’s facilities improve diagnosis and decrease misdiagnosis and subsequent incorrect treatment [9]. For example, Lorenzetti et al. [4] ‘Structured audit feedback and compliance with evidence-based clinical practice guidelines increased diagnostic yield across the emergency departments. Similar conclusions indicate the importance of evaluation and structured feedback on diagnostic practices promoting high care levels in pediatric emergency departments [10].
Nevertheless, several studies have revealed some deficits in diagnosing children in pediatric emergency care. Diagnostic inaccuracy and suboptimal patient outcomes are often discussed with the mismatch of diagnostic practices, absence of biomarkers, and inconsistencies in clinical guidelines application [9,11]. Another researcher pays attention to emergency radiologists’ active participation and cooperation with clinicians concerning diagnostics. Maximizing the rationality of diagnostic imaging in emergency departments, especially in a pediatric environment, could consequently improve general quality and safety, hence developing better patient satisfaction [6]. Solving these problems involves designing improved guidelines and diagnostic instruments for children, providing accurate diagnosis and efficient treatment [12].
Furthermore, there is limited empirical literature on pediatric emergency diagnostics, especially concerning disparities between age and gender. However, extensive literature examines the diagnostic accuracy of various imaging techniques, including radiography, CT, and ultrasound. A study by Baker and Woolridge [13] and Lodwick et al. [14] reveals that though imaging translates into greater diagnostic certainty, demographic variables also inform diagnoses and therapeutic interventions. For example, physiologic changes with ageing influence the symptoms and course of childhood diseases and how they are diagnosed and treated in emergencies. Filling this gap by looking at the interaction between imaging, clinical pathology, and demographics would improve the precision of diagnosis and clinical decision-making when managing children in emergencies [13,14].
Thus, while prior work has broadened the establishment of rules and conduct of the diagnostic audit to improve the accuracy of diagnosis in PAEDs, there is more work to be done to clarify diagnostic markers and the influence of demographic factors in childhood-tier treatment outcomes. Incorporating the designed clinical recommendations, audit routines, and demographics will enhance diagnostic credibility, increasing speed and patient care in pediatric emergency areas.
Methodology
Data was collected from June to December 2022 in Wad Medani Hospital in Gezira state, Sudan. The study increased diagnostic precision in children’s emergency care and facilitated evidence-based practice by bringing clinical pathology and imaging information together.
Population and Sample Selection
The research subjects were pediatric patients at this age or younger who needed clinical pathology or imaging during the emergency visit. This study used the particular frequency of these Pediatric Emergency Cases (PECs) in the hospital catchment are to make proper sample size. Out of 500 pediatric emergency patients, the study included 385 and excluded the rest of the 115 patients because of the following reasons: Incomplete clinical data, no imaging or biomarker test available for comparison. After pre-screening, reduction and data filtering the participants selected were 400 in number, half of which were females 194 and the other half were males 191. All cases that met the following inclusion criteria were included: It compared only those cases with full follow-up and complete secondary diagnostic information; cases for which such information was missing were excluded to maximize case reliability.
Data Collection Instruments
• Parent/Guardian Questionnaire: This structured
questionnaire captured primary demographic data and their
behaviours, the medical history of the patients, the onset of
their symptoms, treatment history, and exposure history. These
variables assisted in placing each patient’s clinical findings into
perspective and determining diagnosis issues.
• Clinical Checklist: To complete data collection, a clinical
checklist, developed to capture key patient information, was used
to record background characteristics, including age and gender,
physiological parameters, provenance of pathology/biomarkers,
radiology, primary diagnosis, and therapeutic consequences.
• Biomarker Guidelines: Diagnostic biomarkers were
chosen according to the type of clinical situation frequently
encountered in children’s emergency departments. Thus, the
importance of inflammatory indicators, infection origin, and
organ-typical bio indicative markers for differential diagnostics
was emphasized. Routine criteriology was utilized to reduce
variability in biomarker interpretation and improve diagnostic
calibration.
• Data Validation Protocol: A data validation protocol
was followed to control data accuracy and validity. Each data
collector first received calibration regarding using checklists and
the meaning of biomarkers and imaging scans. Other clinicians
collected and checked the diagnostic data to enhance the opposed
results, while the weekly data reviewing helped monitor variability
and improve the data quality.
Since each clinician completed an approximately 2-hour intake interview with each participant, efforts were made to optimize diagnostic inter-observer agreement by providing extensive training to all clinicians and data collection staff. Two or more clinicians read imaging and pathology data for each case to get different views.
Statistical Analysis
Diagnostic performance was assessed for different study population subgroups and specific disease states based on sensitivity, specificity, Positive predictive value (PPV), and Negative predictive value (NPV). Frequency distributions for each age group and gender were also computed. Regarding each of the diagnostic metrics, 95% confidence intervals were obtained to give an estimate of accuracy. Logistic regression was used to analyze the changes in trends in sensitivity and specificity to evaluate the variation of diagnostic efficiency by age. Furthermore, other chisquare tests were employed to test the relationship between two or more categorical variables, such as the diagnostic outcomes and age brackets. All the data analysis was done using SPSS software, and a significance level of p < 0.05 was used to reinforce the results obtained. The goodness of fit of the regression models was checked, and diagnostic measure reliability across age groups was checked through purposive sensitivity analysis.
Assumed Consequences and Repercussions
The study expected to show that merging clinical pathology and image data optimizes clinical diagnosis in pediatric Pinpoint emergencies. The study was conducted to understand diagnostic patterns’ demographic and clinical correlates across age and gender. Based on research, studies are meant to contribute to custom prospective diagnostic plans for pediatric emergency environments to improve children’s clinical outcomes.
Ethics and Informed Consent
The study was approved by the Wad Medani Hospital’s Ethics Committee. Parents or legal guardians provided informed consent, and children were given permission. For the participant’s anonymity and privacy, data were deleted from their cloud storage and only used for analysis exclusively for research purposes as required by ethics.
Results
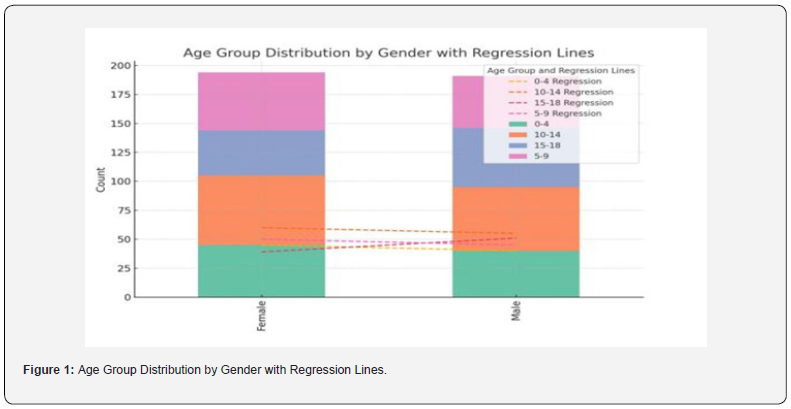
The demographic profile of the study sample is illustrated in Table 1 by gender and age. Among the female participants, the majority 60 were 10-14 years of age, and the rest 50 were 5-9 years of age. Male participants’ data were nearly equally distributed across the different age groups of participants, of which the largest number of males were from 15-18 years (n= 51). Such demographic stratification enables a differential evaluation of the extent of diagnostic accuracy across age and gender.

The diagnostic performances of the utilized testing protocols are highlighted in Table 2, providing results on sensitivity, specificity, probability of a positive outcome (PPV), and probability of negative results (NPV). The sensitivity rate from the analysis turned out to be 87%, which shows an excellent performance of the diagnostic tests in detecting actual positives. Specificity was also high at 92%, proving the model’s accurate negative sample identification efficiency. Moreover, the overall accuracy in the form of PPV and NPV was 90% and 89%, respectively, implying that the diagnostic strategies effectively narrowed down the range of diagnosis while ruling out some of those that were negative.



Table 3 provides diagnostic performance analysis with age split into categories: age group 0-4 years, age group 5-9 years, age group 10-14 years, and age group 15-18 years. Sensitivity values varied between 89.7% among those in the 5-9 age category and 92.8% among children aged 10-14 years, suggesting that the diagnostic tests produced highly acceptable levels of correct identification of cases by age group. Regarding the scores for specificity, the variation was noted. In contrast, the highest score was pointed out in the 15-18 age group study (specificity of 89.8% implies specificity of diagnostic procedures in this age range). The overall PPV and NPV stayed high and had minimum fluctuations in all age groups. Sensitivity confidence intervals also contributed to assessing the reliability of the diagnostic metrics, making further contributions. These findings show that diagnostic accuracy does not decrease over childhood, implying that the diagnosis-related protocols used here are appropriate for children of different developmental ages.
Table 4 describes the diagnostic performance of the proposed method for predicting the presence of a particular clinical condition: sepsis, non-sepsis, meningitis, and non-meningitis. The highest sensitivity and specificity were observed in the cases of meningitis, with a sensitivity level equaling 93.0% and a specificity of 86.5 %. This implies that the diagnostic protocol presented is very efficient in identifying cases of meningitis, which is crucial because of the enormous need to identify such critical illnesses correctly. The sensitivity of non-sepsis cases was slightly lower (88.5%), yet the specificity was still high (84.5%). Thus, robust diagnostic discrimination in non-sepsis cases was established as well. The values of PPV and NPV across the conditions support the testing accuracy of the protocols, with values above 85% pointing to the stability and reliability of the testing scenarios of different pediatric emergency conditions. The Confidence intervals for sensitivity offered statistical enhancement, underpinning the diagnostic performance in the conditions examined.
Figure 1 shows the number of male and female participants by age group and the regression lines representing trends in each age group: 0-4, 5-9, 10-14, and 15-18 years. The bars alongside the y-axis are proportional to the number of people in each gender and age group. Each age has regression lines showing similar patterns in distribution, and they indicate that female players dominate the 10-14 age group while male participants increase in the 15-18 age bracket. This figure also states that there should be balance within the sample, demonstrating what can be offered for subsequent age- and gender-stratified analyses.
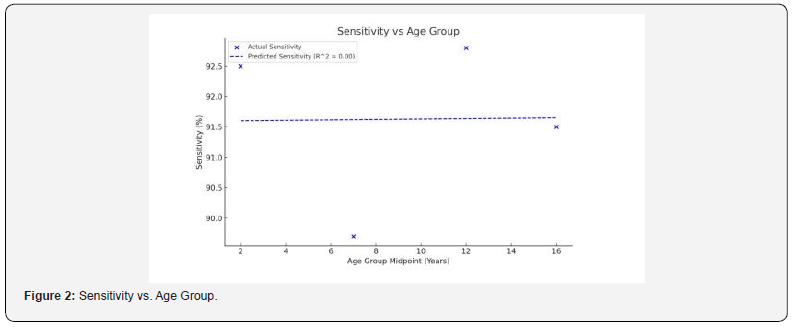
In Figure 2, the sensitivity percentages are given as a percentage of the total, specifically for different age brackets, namely at each midpoint of each age group. Sensitivity is equally retained relatively high among all age groups, and it does not go high or low at any particular time since the regression line shows that it is flat (R² = 0.00). These findings indicate that diagnostic accuracy in terms of sensitivity is invariant with age variations for the pediatric study sample. This consistency demonstrates the effectiveness of a highly reliable diagnostic protocol to identify true positives regardless of age.
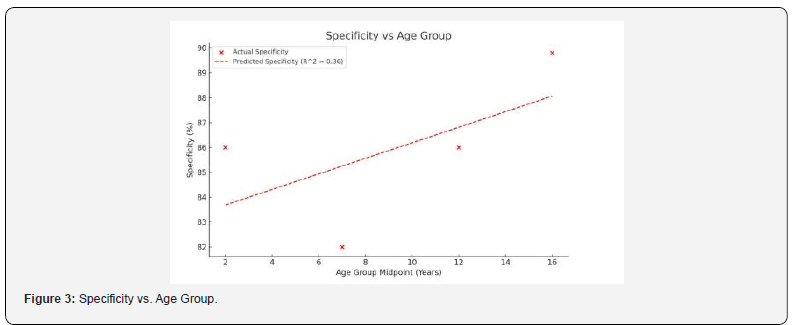
Figure 3 shows the specificity estimates for different age groups and specifies the y-axis as the age group midpoint. The trend is positive, and the specificity values augment with age, as evidenced by a higher regression line showing a positive correlation though a weak positive correlation (R² = 0.36). The diagnostic tests are more proficient in accurately identifying true negatives in the other age classes of the older populations. Such variability can mean that specificity decreases with age and that the nature of diagnostic work at different ages may differ due to developmental changes.
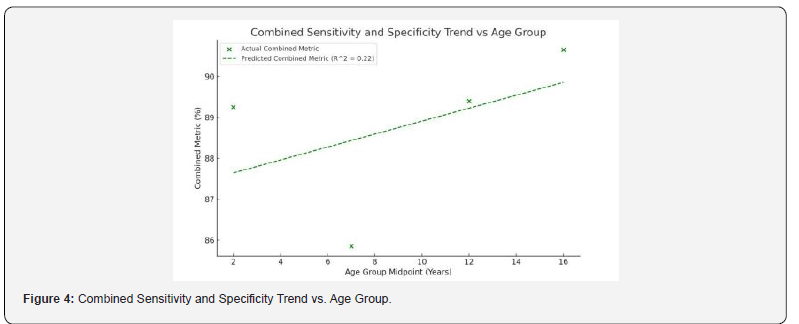
Figure 4 combines sensitivity and specificity as a diagnostic performance of the computer model based on the age group midpoints. The regression line shows that overall, there is a slight tendency of improved combined diagnostic accuracy with increasing age; in other words, increasing age is associated with higher overall test performance for the older pediatric groups (R² = 0.22). This composite measure accentuates the general strength of the diagnostic strategy in all the progressive age strata and postulates an additional advantage in diagnostic accuracy among the later participants.
Discussion
This case highlights the critical aspects of diagnosing and managing MPSIVA, emphasizing the importance of early detection and genetic testing in providing targeted treatment and improving patient outcomes. Ongoing research and advancements in therapies are essential for better management and potentially extending the life expectancy of individuals with Morquio syndrome.
This study’s integration of clinical pathology and imaging data revealed high diagnostic performance, with sensitivity and specificity values of 87% and 92%, respectively. This multi-modal approach aligns with existing evidence that combines diagnostic methods to enhance accuracy in complex cases, particularly in pediatric emergency settings where rapid and accurate diagnosis is critical [15]. Previous research highlights those integrated approaches, especially those involving both biomarkers and imaging, can improve the detection of critical conditions while reducing misdiagnoses, an outcome essential for improving patient outcomes in high-stakes environments [16].
The comparable fluctuations in sensitivity across different age groups show that the diagnostic algorithm isolates actual positives reliably. The present study is in line with Francesca et al., who revealed a weak correlation between age and sensitivity values because high standards of sensitivity require global compliance with diagnostic criteria, and false negative rates do not depend on age [17]. Our study, however, recorded a slight improvement in specificity with increasing age, hinting at an improved ability to classify actual negative cases in older children correctly. This trend may be due to physiological and developmental changes. As children grow older, symptoms might be more transparent, which is also evident from the fact that diagnostic accuracy increases when patients are close to adolescence [18].
The present paper also tested whether gender had any effect on diagnostic accuracy, and it was observed that there were no striking differences between the two genders. As Lindsay and Kolne also pointed out, gender-blind protocols do not erode diagnostic reliability in children’s experiences, similar to that in adults, where diagnostic tools are calibrated to reflect the inherent variability of children’s presentations of their condition. Similarly, the uniformity of the diagnostic performance regarding genders shows that the multi-modal approach might not require changes in different genders and different children’s populations, meaning that the technique is applicable across different subpopulations of pediatric clients without particular modifications [19].
A breakdown of diagnostic efficiency by condition showed acute meningitis achieving near impressive sensitivity of 93%. This high sensitivity is essential in emergency conditions; for example, detection of central nervous system infections should be done within the shortest time so that the patient can be treated immediately. Sources revealed that in diagnosing central nervous system infection, integrating biomarkers with imaging data is helpful because it decreases the possibility of missing a case and increases certainty [20]. Lower sensitivity was determined in the non-sepsis group probably because sepsis diagnosis can be pretty straightforward, whereas other diseases manifest as a wide range of subtle symptoms. Singh and Sittig also mentioned that non-specific presentations could lead to low diagnostic sensitivity, improving diagnostic markers among such patients to increase their sensitivity [21].
The gradual increase in specificity with age implies that agerelated criteria could be used more in pediatric emergencies. Immune Thrombocytopenic Purpura (ITP) is more common in younger children who may not show apparent signs, making differentiating between the disease and other conditions difficult and increasing false favorable rates. In a similar study, Jain et al. identified that a systematic approach in a protocol for diagnostics could minimize false positives, particularly among young patients, and potentially improve sensitivity in elder children who present unique clinical manifestations [22]. Our study aligns with this view, suggesting that with children’s development, diagnostic specificity is high, perhaps attributable to variation in clinical characteristics in older age groups of children.
The high PPV and NPV across conditions also support the diagnostic protocol’s robustness. High PPV and NPV are important in clinical practice because they give clinicians an estimate of the extent of disease and non-disease, which aids in decision-making, ruling out conditions that are unnecessary to treat. This concurs with Apostolopoulos et al. [23], whereby multivariate diagnosis frequently yields high PPV and NPV to offer convincing evidence of the disease’s presence or absence [23].
The strength of this study is that subjects were selected and grouped based on age and gender, reducing sample bias in the pediatric population. Moreover, incorporating clinical pathology and imaging harmonizes clinical pathways with best diagnostics practices in children’s emergency centers and lays a strong precedent for accurate diagnosis. Therefore, the limitation arising from the single-center study is that the results cannot be applied to other centers with different population mixes or staffing levels. Subsequent multicenter research investigations may, therefore, corroborate these observations in different healthcare settings to establish the generalizability of the protocol.
Future studies should also look at the protocol’s performance when used in uncommon conditions in which demographic and clinical characteristics may affect the accuracy of the test. For example, situations involving diseases that are not commonly diagnosed or manifested through some symptoms can be described as cases when conventional diagnostic methods decrease the probability of success, and certain adjustments are needed to enhance diagnostic effectiveness. These findings underscore the ongoing improvement of diagnostic algorithms so that they are applicable across the broad spectrum of pediatric emergencies, as noted by [24].
Hence, this study augments the literature in support of clinical and imaging data combinations in the evaluation of children. Constant sensitivity and high specificity established in crosssectional design conform to the usefulness of this approach in accurately diagnosing critical ailments among people of different ages and genders. The increase of specificity with age also indicates the possible need for age-related criteria to improve diagnostic accuracy, especially in the youngest children, where there seems to be a higher sum of overlapping diagnostics. In agreement with Reilly & Evans, age-related modifications might improve diagnostic precision and decrease intragrant variability, contributing to the enhanced guarding of the children’s welfare in emergency departments [25].
Consequently, the research outcomes of the current study highlight the real-world importance of the combined diagnostic strategy in pediatric emergencies. The protocol integrated clinical and imaging data and showed high diagnostic accuracy in various pediatric patients and in diagnosing severe pathologies such as meningitis. In emergency clinical situations, these findings support the utilization of multi-modal diagnostics and propose that age-specific criteria might enhance the diagnostic outcomes even more. Such research should be replicated in other centers, and other condition-specific markers should also be identified to fine-tune the approach used to diagnose these young patients.
Conclusion
The results of this study show how integrating diagnostic data from CP and imaging may enhance the diagnostic performance of cases presented in pediatric emergency departments. The overall percentage score of the protocol was 78%; sensitivity = 87% and specificity = 92%, suggesting an acceptable level of reliability in identifying true positive and true negative cases in different ages and genders. Specificity was comparable but marginally higher in the older children, hence the possibility of enhancing sensitivity more dramatically and performing even optimally in younger children who often present with vague symptoms. Again, since the analysis is done based on conditions, the high sensitivity for meningitis reveals that the protocol is useful in establishing invaluable conditions in the first instance, especially in emergency settings requiring quick diagnosis. However, these findings point towards further diagnostic strategies in multimodal procedures, and the regional nature of this study urges further studies in a multi-center design. The investigators in this study recommend that using age-adjusted criteria derived from these findings might enhance diagnostic accuracy, decrease the likelihood of falsepositive diagnoses, and augment patients’ quality and survival outcomes in pediatric emergency departments.
Limitations and Future Recommendations
One of the major limitations of this work reflects its focus on the single center, which would limit the ability to generalize findings to other pediatric populations or different clinical settings. Furthermore, though the protocol yielded impressive accuracy, some diseases with ambiguous or similar symptoms may endanger the specificity of diagnosis in children. As such, future work should focus on analyzing such protocols concerning multiple sites to increase the external validity of its conclusions.
Enhanced and continued research is encouraged to refine diagnostic markers and characteristics specific to each age category, especially for conditions with minimal manifestation or nonspecific signs and symptoms. Further adjusting these diagnostic tools according to specific age-related physiological changes could help enhance accuracy and, ultimately, the variable nature of pediatric emergencies.
Declaration and Statements
Funding: This study was made possible thanks to financial support from 10Scholars Academy. The researchers are grateful for the grant that enabled data collection and analysis. Notably, the funders were not involved in the study design, data interpretation, or manuscript preparation, ensuring the objectivity of the research outcomes.
Acknowledgments: The authors sincerely thank the Wad Medani Hospital and Gezira University staff for their invaluable support throughout the study. We gratefully acknowledge the clinicians and technicians who contributed to data collection and the participants whose data enabled this research. Special thanks are owed to 10Scholars Academy for their generous funding and support. Additionally, the authors recognize the insightful feedback from colleagues and reviewers, which significantly enhanced the clarity and quality of this manuscript.
Conflict of Interest Disclosure: The authors affirm that they have no potential conflicts of interest related to this study’s research, authorship, or publication. All data interpretations and conclusions are solely the authors’ responsibility and were conducted independently of the funding source.
References
- Vinson DR (2002) Treatment patterns of isolated benign headache in US emergency departments. Annals of emergency medicine 39(3): 215-222.
- Shaw KA, Cutler DJ, Okou D, Dodd A, Aronow BJ, et al. (2019) Genetic variants and pathways implicated in a pediatric inflammatory bowel disease cohort. Genes & Immunity 20(2): 131-142.
- Okubo Y, Nochioka K, Testa MA (2018) The impact of pediatric obesity on hospitalized children with lower respiratory tract infections in the United States. The clinical respiratory journal 12(4): 1479-1484.
- Lorenzetti DL, Quan H, Lucyk K, Cunningham C, Hennessy D, et al. (2018) Strategies for improving physician documentation in the emergency department: a systematic review. BMC emergency medicine 18(1): 1-12.
- Arora R, Kannikeswaran N (2018) Radiology callbacks to a pediatric emergency department and their clinical impact. Pediatric Emergency Care 34(6): 422-425.
- Mills AM, Raja AS, Marin JR (2015) Optimizing diagnostic imaging in the emergency department. Academic Emergency Medicine 22(5): 625-631.
- Tamelytė E, Vaičekauskienė G, Dagys A, Lapinskas T, Jankauskaitė L (2019) Early blood biomarkers to improve sepsis/bacteremia diagnostics in pediatric emergency settings. Medicina 55(4): 99.
- Whiting P, Rutjes AW, Reitsma JB, Glas AS, Bossuyt PM, et al. (2004) Sources of variation and bias in studies of diagnostic accuracy: a systematic review. Annals of Internal Medicine 140(3): 189-202.
- Mahajan P, Grubenhoff JA, Cranford J, Bhatt M, Chamberlain JM, et al. (2023) Types of diagnostic errors reported by paediatric emergency providers in a global paediatric emergency care research network. BMJ open quality 12(1): e002062.
- Foy R, Skrypak M, Alderson S, Ivers NM, McInerney B, et al. (2020) Revitalizing audit and feedback to improve patient care. BMJ, pp. 368.
- Zanetto L, van de Maat J, Nieboer D, Moll H, Gervaix A, et al. (2022) Diagnostic variation for febrile children in European emergency departments. European journal of pediatrics 181(6): 2481-2490.
- Scaglione M, Masala S, Iacobellis F, Tonerini M, Sica G, et al. (2023) Imaging in non-traumatic emergencies. Tomography 9(3): 1133-1136.
- Baker N, Woolridge D (2013) Emerging concepts in pediatric emergency radiology. Pediatric Clinics of North America 60(5): 1139-1151.
- Lodwick DL, Cooper JN, Lawrence AE, Kelleher KJ, Minneci PC, et al. (2019) Factors affecting emergency department computed tomography use in children. Journal of Surgical Research 241: 294-301.
- Ball JR, Miller BT, Balogh EP (2015) Improving diagnosis in health care. Washington (DC): National Academies Press, USA.
- Abi-Dargham A, Horga G (2016) The search for imaging biomarkers in psychiatric disorders. Nature medicine 22(11): 1248-1255.
- Francesca S, Francesca M, Fabio C, Lucia L, Fabrizio F, et al. (2019) Pediatric drug hypersensitivity: which diagnostic tests? Acta Bio Medica: Atenei Parmensis 90(Suppl 3): 94-107.
- Stuart HC, Prugh DG (1960) The healthy child: his physical, psychological, and social development. Harvard University Press 6(1): 124-125.
- Lindsay S, Kolne K (2022) Understanding clinicians’ strategies for providing gender-sensitive care: an exploration among pediatric rehabilitation health care providers. Disability and Rehabilitation 44(11): 2437-2447.
- Bharucha T, Gangadharan B, Kumar A, de Lamballerie X, Newton PN, et al. (2019) Mass spectrometry-based proteomic techniques to identify cerebrospinal fluid biomarkers for diagnosing suspected central nervous system infections. A systematic review. Journal of Infection 79(5): 407-418.
- Singh H, Sittig DF (2015) Advancing the science of measurement of diagnostic errors in healthcare: the Safer Dx framework. BMJ quality & safety 24(2): 103-110.
- Jain S, Williams DJ, Arnold SR, Ampofo K, Bramley AM, et al. (2015) Community-acquired pneumonia requiring hospitalization among US children. New England Journal of Medicine 372(9): 835-845.
- Apostolopoulos ID, Papathanasiou ND, Apostolopoulos DJ, Papandrianos N, Papageorgiou EI (2024) A Multi-Modal Machine Learning Methodology for Predicting Solitary Pulmonary Nodule Malignancy in Patients Undergoing PET/CT Examination. Big Data and Cognitive Computing 8(8): 85.
- Guttmann A, Razzaq A, Lindsay P, Zagorski B, Anderson GM (2006) Development of measures of the quality of emergency department care for children using a structured panel process. Pediatrics 118(1): 114-123.
- Reilly BM, Evans AT (2006) Translating clinical research into clinical practice: impact of using prediction rules to make decisions. Annals of Internal Medicine 144(3): 201-209.






























