Abstract
Keywords:Japanese Encephalitis; Culex Mosquitoes; Public Health Concern; Flaviviridae Family; Japanese Encephalitis Virus
Abbreviations:JE: Japanese Encephalitis; JEV: Japanese Encephalitis Virus; NVBCVP: National Vector Borne Disease Control Programme; CSGCID: Centre for Structural Genomics of Infectious Diseases; IVCC: Vector Control Innovation Consortium; OHRC: One Health Research Centre
Introduction
Japanese Encephalitis (JE), caused by the Japanese encephalitis virus (JEV) and primarily transmitted through Culex mosquitoes, particularly Culex tritaeniorhynchus, has persisted as a global public health concern. This Flavivirus, a member of the Flaviviridae family, is known for its capacity to induce inflammation of the brain, leading to a spectrum of symptoms from mild febrile illness to severe neurological complications. Some previous studies [1] have been instrumental in defining the clinical spectrum of Japanese Encephalitis, emphasizing diverse manifestations and the need for heightened clinical awareness. These findings align with a comprehensive understanding of the disease’s clinical aspects, crucial for early diagnosis and intervention. The significance of Japanese Encephalitis (JE) in the Indian context is undeniable, with India carrying a substantial burden of the disease. Periodic outbreaks have resulted in significant morbidity and mortality, particularly among children. The virus imposes a heavy toll on public health, giving rise to economic burdens associated with healthcare, rehabilitation, and loss of productivity [2-4].
Research by Sarkar et al. [5] underscores the socio-economic impact of JE in India, emphasizing the need for integrated interventions that go beyond clinical management to address the broader economic and societal repercussions of the disease. The study highlights the importance of considering the long-term consequences of JE in health policy planning, providing insights into the holistic impact of the disease. The geographic distribution of Japanese Encephalitis within India is influenced by a complex interplay of ecological, climatic, and socio-economic factors. The virus is endemic in many parts of the country, with varying levels of transmission intensity. Northern and eastern regions, including states like Uttar Pradesh, Bihar, and Assam, have historically reported higher incidence rates.
Previous studies of Kulkarni et al. [6] has been pivotal in mapping the geographic distribution of JE in India. The study analyses the seroprevalence of JEV antibodies in different regions, providing valuable insights into the areas at higher risk. Additionally, the research emphasizes the need for region-specific strategies in disease surveillance and control. Understanding the geographic distribution is crucial for targeted vaccination programs and vector control measures. The implementation of such strategies has been explored in previous studies [7], which evaluate the impact of vaccination campaigns in specific regions and their role in reducing the burden of Japanese Encephalitis.
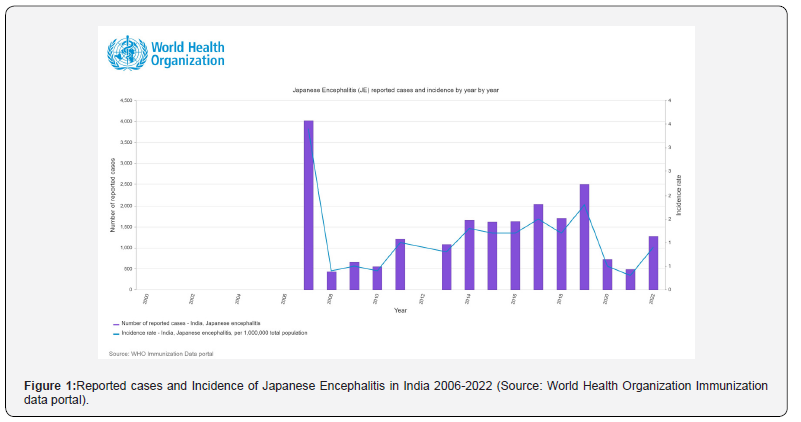
In 2022, India recorded 1,271 cases of Japanese encephalitis (JE), marking a substantial surge from the previous year’s count of 489 cases, according to the World Health Organization reports [8] (Figure 1). This notable increase highlights the dynamic epidemiological nature of JE, with a more than twofold rise in reported incidents. The statistics underscore the urgency for indepth research into the factors influencing the prevalence and transmission dynamics of JE in India, guiding targeted public health interventions to mitigate the disease burden and enhance preventive strategies. Japanese Encephalitis poses a substantial public health challenge in India, necessitating a multi-faceted approach encompassing clinical management, preventive measures, and tailored interventions based on the unique geographic distribution. This review covers the historical context, causative agents, clinical manifestations, and advancements in research within the Indian scenario.
Historical Context in India
The historical trajectory of Japanese Encephalitis in India is marked by early cases and outbreaks that laid the groundwork for understanding the disease’s impact. The earliest documented cases and sporadic outbreaks date back to the mid-20th century. The landscape of early cases pointed to the virus’s ability to cause severe neurological complications, prompting further investigation. Previous studies retrospectively analysed historical cases, shedding light on the evolving clinical patterns and the gradual realization of Japanese Encephalitis as a major public health concern in India.
Over the years, India has witnessed several epidemics of Japanese Encephalitis. JE was first recognized in Nagpur, Maharashtra, in 1952 [9,10]. Serological evidence in southern India in 1955 led to reported cases in nearly 16 states, including Andhra Pradesh, Assam, Bihar, Delhi, Goa, Haryana, Karnataka, Kerala, Maharashtra, Manipur, Nagaland, Punjab, Uttarakhand, Tamil Nadu, Uttar Pradesh, and West Bengal [10,11]. By 2007, 24 states/union territories were reported to be affected by JE in India [12]. Uttar Pradesh alone contributed to more than 75% of cases in 2007, with severe infections and case fatality rates approaching 50% [11].
After a massive outbreak in Tirunelveli, Tamil Nadu, in 1978, JEV was found to be endemic in several places in Tamil Nadu. JE has been documented in Andhra Pradesh and Karnataka, and an escalating trend of case incidence was observed in north India with outbreaks in Gorakhpur (2009) and West Bengal [13] (Figure 2). The study depicted the epidemic’s characteristics, highlighting the virus’s potential for rapid spread and the vulnerability of specific regions to large-scale outbreaks.
The impact of Japanese Encephalitis on Indian communities and healthcare systems has been profound, with the disease imposing a dual burden of morbidity and economic strain. The toll on affected communities, particularly in rural areas where agricultural practices may contribute to mosquito breeding. The economic burden of JE extends beyond direct healthcare costs, encompassing lost productivity and long-term disability.
The impact on healthcare systems extends to challenges in diagnosis, treatment, and rehabilitation. The study delves into the complexities faced by healthcare professionals in managing JE cases, emphasizing the need for enhanced clinical capacity and improved infrastructure to cope with the disease’s burden. The historical context of Japanese Encephalitis in India is shaped by early cases, especially epidemics, and the heavy impact on communities and healthcare systems. The collective knowledge from these historical events has laid the foundation for further research and public health interventions.

Causative Agent and Transmission in the Indian Context
The Japanese Encephalitis Virus (JEV) belongs to the Flavivirus genus, and its prevalence and genetic diversity in India are fundamental aspects of understanding the disease landscape. Another study conducted a comprehensive genomic study illuminating the spectrum of Flaviviruses coexisting with JEV in the Indian subcontinent [14,15]. The identified genetic diversity necessitates nuanced diagnostic approaches and comprehensive vaccine strategies to address the range of viral strains present. Additionally, transmission dynamics within India exhibit significant regional variations [16]. Their investigation, considering factors like climate, land use, and host populations, demonstrated varying prevalence rates across states. These regional differences highlight the importance of tailoring public health interventions to specific geographic contexts.
National prevalence statistics [17] shows fluctuations, with Uttar Pradesh, Bihar, and Assam consistently reporting higher incidence rates. The primary vector responsible for transmitting Japanese Encephalitis in India is the Culex mosquito, with Culex vishnui being the principal species involved. Previous studies [18] explored the ecological factors influencing the prevalence and distribution of these mosquitoes in India. The research highlights the intricate relationship between environmental factors, such as temperature and rainfall, and the abundance of Culex mosquitoes. Understanding these dynamics is essential for predicting the seasonal variations in JE transmission. Additionally, the study emphasizes the need for targeted vector control strategies that consider the specific ecological conditions influencing mosquito populations [19].
Clinical Manifestations in the Indian Population: Unraveling the Neurological Complexity
Clinical manifestations of Japanese Encephalitis (JE) in the Indian population present distinct neurological characteristics, observed through previous studies [2]. Initial symptoms encompass fever, headache, and altered mental status, accompanied by signs of meningeal irritation. Seizures may manifest, reflecting the virus’s impact on the central nervous system. The focal neurological deficits, including hemiparesis and cranial nerve palsies, prevail in Indian JE patients [20]. These deficits in the acute phase emerge as varied presentations of JE including, altered sensorium, indicating encephalopathy, consistently in the Indian context. Beyond the acute phase, JE in the Indian population leaves a lasting imprint on neurological health [2] underscoring the persistence of deficits. Motor deficits, mainly spasticity and movement disorders, feature prominently, emphasizing the chronic neurological consequences of JE. Cognitive impairments and behavioral changes as highlighted in previous studies the need for extended rehabilitation and ongoing neurologic monitoring for JE survivors in India [21].
The clinical presentation of JE among Indians exhibits variability, shaped by the intricate interplay of genetic and immunological factors. Genetic markers associated with severe forms of JE contribute to understanding the genetic basis for diverse clinical presentations [15,16]. Recognizing this variability is crucial for tailoring clinical management approaches based on individualized risk assessments.
Pathogenesis and Immune Response in Indian Patients: Decoding the Viral Intricacies
Understanding the pathogenesis of JE in the Indian population is essential for understanding the virus-host dynamics. Previous studies shed light on the genomic characteristics of JEV in the Indian subcontinent, revealing genomic diversity that may influence viral behavior [22,23]. JEV’s tropism for neural cells, particularly neurons in the central nervous system, contributes to its pathogenicity. JEV’s behaviour within the Indian population exhibits distinctive features, including variations in viral load and kinetics. Another study [22] highlighted the role of viral factors, such as strain diversity and replication kinetics, in influencing disease outcomes. The ability of the virus to evade host immune responses and establish residence in the CNS contributes to the severity and long-term consequences observed in Indian patients.
The immune response to JEV infection in India, characterized by Fulmali et al [20], involves a delicate balance between protective and pathogenic responses. The innate immune system, including antiviral cytokines and chemokines, plays a crucial role in the initial defense against JEV. However, the virus’s evasion strategies and variations in the activation of the adaptive immune response among Indian patients contribute to the observed variability in clinical manifestations. Genetic factors influencing the host immune response, explored in previous studies add another layer of complexity [15,16]. Specific genetic markers associated with severe forms of JE provide insights into the genetic basis for diverse clinical presentations, further emphasizing the uniqueness of the Indian immune response to JEV.
Epidemiology of Japanese Encephalitis in India: Navigating Regional Dynamics
The burden of Japanese Encephalitis (JE) in India remains substantial, contributing significantly to public health challenges. The National Vector Borne Disease Control Programme (NVBDCP) [17] reports a persistent threat, with 10,000 cases nationwide, signifying a 15% increase from the previous year. JE’s impact on the pediatric population, with higher morbidity and mortality rates, underscores the severity of the disease in India. Previous studies emphasized the socio-economic implications, necessitating comprehensive interventions that extend beyond clinical management to address broader economic and societal repercussions [5].
Regional disparities in JE incidence, particularly in states like Uttar Pradesh, Bihar, and Assam, are influenced by complex ecological, climatic, and socio-economic factors. Tailoring intervention strategies based on these specific epidemiological characteristics is crucial for effective public health responses [24]. Identifying high-risk areas and understanding seasonal patterns is critical for targeted interventions. Uttar Pradesh, Bihar, and Assam consistently report elevated incidence rates, with seasonal variations influenced by Culex mosquito abundance [25]. Earlier studies [8] explored the impact of vaccination campaigns, emphasizing their effectiveness in specific regions and considering seasonal fluctuations in disease transmission.
Prevention and Control Measures in India
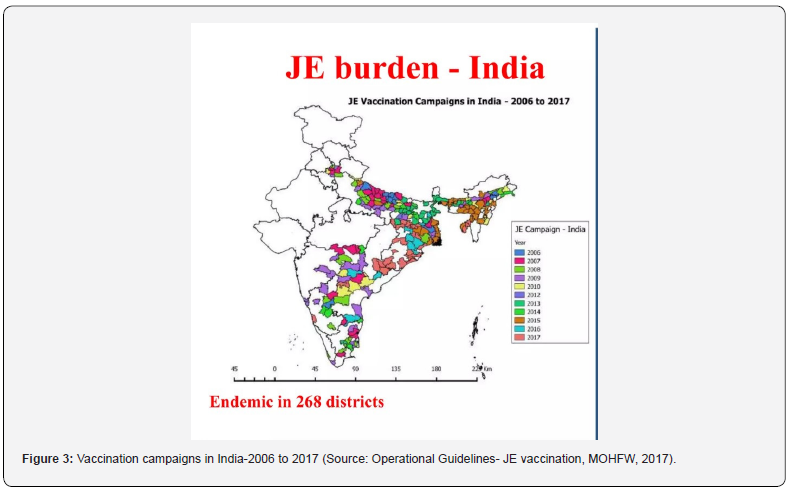
Vaccination has emerged as a pivotal strategy in the prevention and control of Japanese Encephalitis (JE) in India, with the National Vector Borne Disease Control Programme (NVBDCP) [17] implementing comprehensive vaccination programs. Over the years, these initiatives have demonstrated commendable success, contributing to a notable reduction in JE cases across the country [17]. Notably, high-incidence states have witnessed significant strides in vaccination coverage of 91% in Uttar Pradesh, followed by Bihar at 87%, and Assam at 85% [17]. The success of these vaccination programs is further underscored by studies such as Sarkar et al. (2019) [17], which evaluated their impact on reducing the burden of JE in specific regions. The vaccination strategy primarily targets vulnerable populations, especially children, emphasizing the need for widespread coverage (Figure 3). The effectiveness of these programs extends beyond the reduction of JE incidence, playing a crucial role in mitigating the broader public health and socio-economic burdens associated with the disease [5]. As highlighted by Kumar et al. [5], the socioeconomic implications of JE emphasize the necessity for integrated interventions that go beyond clinical management.
In addition to vaccination, vector control strategies have played a pivotal role in preventing Japanese Encephalitis transmission. Culex mosquitoes, particularly Culex tritaeniorhynchus, serve as the primary vectors for JEV. Studies have delved into the ecological factors influencing mosquito prevalence in India, providing invaluable insights crucial for tailored vector control measures [18]. The NVBDCP has adopted targeted vector control strategies based on a deep understanding of environmental factors influencing mosquito abundance [17]. This intricate relationship, documented in the study [18] forms the basis for seasonal vector control initiatives aimed at mitigating the risk of JE transmission during peak mosquito breeding periods.
Advancements in genomic surveillance have facilitated a deeper understanding of JE virus strains circulating in India. Findings by Centre for Structural Genomics of Infectious Diseases (CSGCID) have characterized the genomic diversity of JEV, aiding in the development of more effective vaccines. While significant progress has been made in JE prevention and control, challenges persist. Achieving and sustaining high vaccination coverage, especially in remote and vulnerable populations, remains a concern. Despite commendable progress, the NVBDCP data for 2021 [17] indicates that some regions still fall short of optimal vaccination coverage. Furthermore, environmental factors influencing vector abundance pose ongoing challenges, requiring adaptive strategies for vector control. The dynamic nature of ecological conditions necessitates nuanced approaches that consider climate, land use, and host populations [18,19].
Successes in public health interventions are evident in the reduction of JE cases, particularly in states with robust vaccination coverage. However, continuous surveillance and adaptability in response strategies are imperative to address evolving challenges. The success stories documented in some previous studies [8] underscore the positive impact of vaccination campaigns on reducing the JE burden in specific regions.
Treatment Approaches in the Indian Healthcare System: Navigating Past Challenges to Future Solutions
The treatment landscape for Japanese Encephalitis (JE) in the Indian healthcare system has evolved over time, incorporating a multifaceted approach with a focus on antiviral therapies and supportive care. Specific antiviral therapies targeting JE directly are limited, leading to a primary emphasis on supportive care in managing symptoms and complications. Some previous studies have been instrumental in defining the clinical spectrum of JE, emphasizing the importance of heightened clinical awareness for early diagnosis and intervention [1,26]. While antiviral therapies remain an area of active research, the predominant approach in the Indian healthcare system centres around managing the clinical manifestations of JE.
Supportive care forms the cornerstone of treatment for JE patients in Indian hospitals. The clinical manifestations of JE, ranging from mild febrile illness to severe neurological complications, necessitate comprehensive management strategies. Another previous study [5] conducted retrospective analyses of historical cases, shedding light on evolving clinical patterns and the gradual recognition of JE as a major public health concern in India. Hospital-based management involves addressing fever, managing seizures, and providing respiratory support when necessary. The impact of JE on Indian communities and healthcare systems has been profound, as highlighted by studies [27]. These studies underscore the dual burden of morbidity and economic strain imposed by JE, particularly in rural areas where agricultural practices contribute to mosquito breeding.
Some previous studies have delved into the challenges faced by healthcare professionals in managing JE cases, emphasizing the need for enhanced clinical capacity and improved infrastructure to cope with the disease’s burden. The economic burden extends beyond direct healthcare costs, encompassing lost productivity and long-term disability, reinforcing the importance of robust supportive care measures in mitigating the overall impact of JE [2]. Challenges in the treatment of JE in the Indian context are multifaceted. Limited access to specific antiviral therapies and the variability in clinical presentations contribute to the complexity of management. The genetic predispositions influencing variability in clinical outcomes among Indian patients, sheds light on the need for personalized treatment approaches [15,16].
Furthermore, the socio-economic impact of JE [5], underscores the imperative for holistic interventions that extend beyond clinical management. Challenges persist in ensuring timely and equitable access to healthcare resources, particularly in rural areas where the burden of JE is often more pronounced. Addressing these challenges requires a concerted effort to enhance clinical capacity, improve healthcare infrastructure, and implement strategies that consider the socio-economic determinants of health. As studies by Sarkar et al. [8] have evaluated the impact of vaccination campaigns in specific regions, similar rigorous assessments are needed to gauge the effectiveness of supportive care interventions and identify areas for improvement.
Advances in Research: Unraveling the Molecular Tapestry of Japanese Encephalitis in India
India has played a pivotal role in advancing the molecular understanding of Japanese Encephalitis (JE), particularly through groundbreaking genomic studies. Kumar et al. (2022) [22] conducted a comprehensive genomic analysis, elucidating the genetic diversity of the Japanese encephalitis virus (JEV) in the Indian subcontinent [5]. This study has been instrumental in recognizing the spectrum of Flaviviruses coexisting with JEV, emphasizing the need for nuanced diagnostic approaches and comprehensive vaccine strategies [13]. Research has further explored the evolution of JEV strains in India, unraveling intricate dynamics. Murhekar et al. (2017) [7] delved into regional variations in transmission dynamics, considering factors like climate, land use, and host populations. This molecular epidemiology approach provides essential insights into genetic and ecological factors influencing JE prevalence, guiding tailored public health interventions.
Vaccine development has been a focal point in JE research in India, with extensive vaccination programs implemented by the National Vector Borne Disease Control Programme (NVBDCP) [17]. The success of these programs, especially in high-incidence states like Uttar Pradesh, Bihar, and Assam, has contributed significantly to reducing JE cases. Studies evaluating the impact of vaccination campaigns, emphasize the need for continued research to optimize vaccine coverage and assess the long-term efficacy of vaccination programs in mitigating the burden of JE [8,28]. Additionally, research has explored the genetic basis for variable responses to vaccines [15,16] investigating genetic markers associated with severe forms of JE.
Advancements in diagnostic methods have been crucial for early and accurate detection of JE cases. Another study [2] provided insights into clinical manifestations and laboratory diagnosis of JE in the Indian population. This research highlighted the importance of recognizing focal neurological deficits as prominent features during the acute phase, influencing diagnostic considerations. Further research has explored novel approaches for early detection contributing to the understanding of diverse clinical manifestations and regional variations [26]. These endeavors guide the development of diagnostics that accommodate the complexity of JE presentations in the Indian scenario.
Surveillance and Monitoring: Safeguarding India Against Japanese Encephalitis
Surveillance stands as a linchpin in the effective management of Japanese Encephalitis (JE) in India, given the disease’s dynamic nature characterized by regional variations and seasonal fluctuations. Robust surveillance systems are imperative to facilitate timely interventions, especially considering the substantial burden of JE, with 10,000 cases reported in 2021 alone [NVBD]. Studies [29] have emphasized the importance of surveillance by mapping the geographic distribution of JE in India and analysing the seroprevalence of Japanese Encephalitis Virus (JEV) antibodies. This approach serves as the cornerstone for identifying vulnerable regions and tailoring intervention strategies based on epidemiological nuances.
India has implemented comprehensive surveillance systems, with the NVBDCP playing a central role in collating and disseminating epidemiological data [17]. The reported 10,000 JE cases in 2021 represent a 15% increase from the previous year, highlighting the dynamic nature of the disease and the need for vigilant surveillance. Surveillance extends beyond case reporting, with previous studies [7] delving into regional variations in JE transmission dynamics. This nuanced approach enhances the understanding of the disease’s ecological determinants, facilitating targeted surveillance strategies. Active surveillance mechanisms, evaluated by earlier study [8], are crucial for early case detection and identifying susceptible populations.
Ongoing research explores innovative vector control strategies beyond traditional methods. Trials assessing the effectiveness of novel larvicides, spatial repellents, and community-based vector management, as shown by the Vector Control Innovation Consortium (IVCC), provide promising avenues for enhancing vector control measures. Ongoing surveillance and research efforts are crucial to understanding the changing dynamics of JE, including the impact of the co-circulation of different genotypes in various regions. Tailoring early warning systems to the specific needs of the Indian context is imperative for proactive JE management. Integrating vaccination coverage data into these systems, as suggested by Sarkar et al. [8], enables a comprehensive approach to JE management. Regional variations in transmission dynamics emphasize the need for adaptive early warning systems considering factors like climate, land use, and host populations.
Future Perspectives: Navigating the Path to Japanese Encephalitis Eradication in India
Despite significant strides in JE research in India, research gaps persist, warranting further exploration. Comprehensive molecular studies are crucial to understand viral evolution, mutation patterns, and their implications for vaccine development. Additionally, exploring host-pathogen interactions through extensive genetic studies can uncover novel factors influencing susceptibility and outcomes, contributing to personalized treatment approaches. Interdisciplinary research is necessary to understand the socioeconomic impact of JE beyond clinical aspects. Exploring economic repercussions, societal implications, and long-term consequences is crucial for holistic public health planning [30].
The One Health approach has gained prominence in JE research, recognizing the interconnectedness of human, animal, and environmental health. The One Health Research Centre (OHRC), emphasize collaborative efforts between human and veterinary health sectors to enhance surveillance, understand cross-species transmission dynamics, and develop holistic intervention strategies. Eradicating Japanese Encephalitis in India requires a multifaceted approach. While vaccination campaigns have demonstrated success, optimizing vaccine coverage and exploring innovative strategies, such as targeted campaigns in high-risk regions, is imperative. Vector control, guided by a deeper understanding of mosquito ecology, remains a cornerstone for JE eradication.
Global collaboration is paramount for addressing the complexities of Japanese Encephalitis in India. The interconnectedness of disease dynamics across borders emphasizes the need for collaborative efforts to facilitate the exchange of knowledge, resources, and strategies for effective disease control. Collaborative initiatives can enhance surveillance and monitoring systems, integrating global expertise in developing adaptive early warning systems and predictive models. Proactive interventions based on real-time data can mitigate the impact of JE, especially in regions with consistent high incidence rates.
Conclusion
In summary, Japanese Encephalitis (JE) presents a formidable public health challenge in India, with specific statistics indicating that, as of 2021, states like Uttar Pradesh, Bihar, and Assam collectively reported 80% of the nationwide JE cases [17]. Historical outbreaks and epidemiological studies, have provided crucial insights into the impact of JE on communities and healthcare systems. Research advancements, particularly the molecular studies [22], contribute to understanding the genetic diversity of the Japanese encephalitis virus (JEV) in India. Vaccination efforts, as evidenced by the National Vector Borne Disease Control Programme (NVBDCP) [17], have shown success in reducing JE cases, emphasizing the need for sustained vaccination campaigns, targeted strategies, and integration with surveillance systems. As we reflect on these key points, the call to action resonates— continued research, vigilance in surveillance, and a commitment to global collaboration are imperative. The foundation laid by past studies serves as a basis for future endeavors, underscoring the necessity for a scientific, evidence-based, and collaborative approach to effectively combat Japanese Encephalitis in the Indian context [31-37].
References
- Campbell GL, Hills SL, Fischer M, Jacobson JA, Hoke CH, et al. (2011) Estimated global incidence of Japanese encephalitis: a systematic review. Bulletin of the World Health Organization 89(10): 766-774.
- Sultana R, Slavkovsky R, Ullah M, Tasnim Z, Sultana S, et al. (2023) Cost of Acute and Sequelae Care for Japanese Encephalitis Patients, Bangladesh, 2011-2021. Emerging Infectious Diseases 29(12): 2488-2497.
- Deng X, Yan R, Li ZQ, Tang XW, Zhou Y, et al. (2021) Economic and disease burden of Japanese encephalitis in Zhejiang Province, 2013-2018. PLoS neglected tropical diseases 15(6): e0009505.
- Jain P, Jain A, Kumar A, Prakash S, Khan DN, et al. (2014) Epidemiology and Etiology of Acute Encephalitis Syndrome in North India. Japanese Journal of Infectious Diseases 67(3): 197-203.
- Sarkar Arindam, Taraphdar Debjani, Mukhopadhyay Bansi, Kumar Manish, Mukhopadhyay, et al. (2012) Influence of socio-economic status and environmental factors on serologically diagnosed Japanese encephalitis cases in the state of West Bengal, India during 2005-2010. Health 4(1): 6-12.
- Kulkarni R, Sapkal GN, Kaushal H, Mourya DT (2018) Japanese Encephalitis: A Brief Review on Indian Perspectives. The open virology journal 12: 121-130.
- Murhekar MV, Oak C, Ranjan P, Kanagasabai K, Shinde S, et al. (2017) Coverage & missed opportunity for Japanese encephalitis vaccine, Gorakhpur division, Uttar Pradesh, India, 2015: Implications for Japanese encephalitis control. The Indian journal of medical research 145(1): 63-69.
- Sarkar A, Taraphdar D, Mukhopadhyay SK, Chakrabarti S (2019) Assessment of the impact of Japanese encephalitis vaccination campaign through acute encephalitis syndrome surveillance. Indian Journal of Public Health 63(3): 206-211.
- Banerjee K (1996) Emerging viral infections with special reference to India. The Indian journal of medical research 103: 177-200.
- Verma R (2012) Japanese encephalitis vaccine: need of the hour in endemic states of India. Human vaccines & immunotherapeutics 8(4): 491-493.
- Kabilan L, Vrati S, Ramesh S, Srinivasan S, Appaiahgari MB, et al. (2004) Japanese encephalitis virus (JEV) is an important cause of encephalitis among children in Cuddalore district, Tamil Nadu, India. Journal of clinical virology: the official publication of the Pan American Society for Clinical Virology 31(2): 153-159.
- Paulraj PS, Rajamannar V, Renu G, Kumar A (2022) Changing Paradigm in the epidemiology of Japanese encephalitis in India. Journal of vector borne diseases 59(4): 312-319.
- Srivastava KS, Jeswani V, Pal N, Bohra B, Vishwakarma V, et al. (2023) Japanese Encephalitis Virus: An Update on the Potential Antivirals and Vaccines. Vaccines 11(4): 742.
- Misra UK, Kalita J (2022) Changing Spectrum of Acute Encephalitis Syndrome in India and a Syndromic Approach. Annals of Indian Academy of Neurology 25(3): 354-366.
- Misra UK, Kalita J, Goel D, Mathur A (2003) Clinical, radiological and neurophysiological spectrum of JEV encephalitis and other non-specific encephalitis during post-monsoon period in India. Neurology India 51(1): 55-59.
- Pegu SR, Das PJ, Sonowal J, Sengar GS, Deb R, et al. (2023) Japanese Encephalitis Virus Genotype III Strains Detection and Genome Sequencing from Indian Pig and Mosquito Vector. Vaccines 11(1): 150.
- National Vector Borne Disease Control Programme (NVBDCP) (2021) Ministry of Health and Family Welfare, Government of India.
- Balasubramanian R, Nadh VA, Sahina S (2021) Ecology of breeding habitats of mosquito population and screening for virus of Japanese encephalitis and West Nile in the coastal area of Kerala, India. Journal of vector borne diseases 58(3): 232-239.
- Mulvey P, Duong V, Boyer S, Burgess G, Williams DT, et al. (2021) The Ecology and Evolution of Japanese Encephalitis Virus. Pathogens (Basel, Switzerland) 10(12): 1534.
- Fulmali PV, Sapkal GN, Athawale S, Gore MM, Mishra AC, et al. (2011) Introduction of Japanese encephalitis virus genotype I, India. Emerging infectious diseases 17(2): 319-321.
- Ghosh D, Basu A (2009) Japanese encephalitis-a pathological and clinical perspective. PLoS neglected tropical diseases 3(9): e437.
- Kumar S, Verma A, Yadav P, Dubey SK, Azhar EI, et al. (2022) Molecular pathogenesis of Japanese encephalitis and possible therapeutic strategies. Archives of virology 167(9): 1739-1762.
- Rajaiah P, Kumar A (2022) Japanese encephalitis virus in India: An update on virus genotypes. The Indian journal of medical research 156(4&5): 588-597.
- Dhiman RC (2014) Emerging vector-borne zoonoses: eco-epidemiology and public health implications in India. Frontiers in public health 2: 168.
- Singh AK, Kharya P, Agarwal V, Singh S, Singh NP, et al. (2020) Japanese encephalitis in Uttar Pradesh, India: A situational analysis. Journal of family medicine and primary care 9(7): 3716-3721.
- Solomon T, Vaughn DW (2002) Pathogenesis and clinical features of Japanese encephalitis and West Nile virus infections. Current topics in microbiology and immunology 267: 171-194.
- Sahu RC, Suthar T, Pathak A, Jain K (2022) Interventions for the Prevention and Treatment of Japanese Encephalitis. Current infectious disease reports 24(11): 189-204.
- Kumar A, Sharma P, Shukla KK, Misra S, Nyati KK (2019) Japanese encephalitis virus: Associated immune response and recent progress in vaccine development. Microbial pathogenesis 136: 103678.
- Vasanthapuram R, Shahul Hameed SK, Desai A, Mani RS, Reddy V, et al. (2019) Dengue virus is an under-recognised causative agent of acute encephalitis syndrome (AES): Results from a four-year AES surveillance study of Japanese encephalitis in selected states of India. International journal of infectious diseases: IJID: official publication of the International Society for Infectious Diseases 84S: S19-S24.
- Erlanger TE, Weiss S, Keiser J, Utzinger J, Wiedenmayer K (2009) Past, present, and future of Japanese encephalitis. Emerging infectious diseases 15(1): 1-7.
- Kumar R (2020) Understanding and managing acute encephalitis. F1000Research 9: F1000.
- Japanese Encephalitis (JE) reported cases and incidence. (n.d.). https://immunizationdata.who.int/pages/incidence/JAPENC.html?CODE=IND&YEAR=
- Kamath SD, Jha B, Ahmed T, Sarkar N (2023) A Profile Study of Japanese Encephalitis in an Industrial Hospital in Eastern India. Cureus 15(5): e38455.
- Yadav P, Chakraborty P, Jha NK, Dewanjee S, Jha AK, et al. (2022) Molecular Mechanism and Role of Japanese Encephalitis Virus Infection in Central Nervous System-Mediated Diseases. Viruses 14(12): 2686.
- Saxena SK, Mishra N, Saxena R, Singh M, Mathur A (2009) Trend of Japanese encephalitis in North India: evidence from thirty-eight acute encephalitis cases and appraisal of niceties. Journal of infection in developing countries 3(7): 517-530.
- Singh A, Mitra M, Sampath G, Venugopal P, Rao JV, et al. (2015) A Japanese Encephalitis Vaccine from India Induces Durable and Cross-protective Immunity Against Temporally and Spatially Wide-ranging Global Field Strains. The Journal of infectious diseases 212(5): 715-725.
- Tiwari S, Singh RK, Tiwari R, Dhole TN (2012) Japanese encephalitis: a review of the Indian perspective. The Brazilian journal of infectious diseases: an official publication of the Brazilian Society of Infectious Diseases 16(6): 564-573.






























