Survival Rate and Short-Term Outcomes of Extremely Preterm Infants: A Tertiary Care Center Experience from the Private Sector
Rafat Mosalli1,2*, Mohammed Al Matrafi1, Ahmed Hafez Mousa3, Ahmed Baabad1, Ahmed Binselm2, Meshal Hosni2, Mayada Mazroua2, Ahmed Shueai Salahi1, Mohammed Al Matrafi1, Douaa Alawi Alsaidi2 and Fahad Al Hazzani4
1Department of Pediatrics, Umm Al-Qura University, Makkah, Saudi Arabia
2Department of Pediatrics, International Medical Center, Jeddah, Saudi Arabia
3College of Medicine and Surgery, Batterjee Medical College, Jeddah, Saudi Arabia
4Department of Pediatrics, King Faisal Specialist Hospital and Research Center, Riyadh, Saudi Arabia
Submission: January 05, 2023; Published: February 20, 2024
*Corresponding author: Rafat Mosalli, Department of Pediatrics, Umm Al-Qura University, Makkah, International Medical Center, Jeddah, Saudi Arabia
How to cite this article: Rafat M, Mohammed Al M, Ahmed Hafez M, Ahmed B, Ahmed B, et al. Survival Rate and Short-Term Outcomes of Extremely Preterm Infants: A Tertiary Care Center Experience from the Private Sector. Acad J Ped Neonatol 2024; 13(4): 555923. 10.19080/AJPN.2024.13.555923
Abstract
Background: Premature birth is one of the leading causes of death in the world. The global incidence of prematurity ranges from 5 to 11 percent of all births.
Aim: The aim of this study was to assess the outcome of extremely preterm infants born below 29 weeks in our institution, with regard survival, and major short-term outcomes, and compare our results with national and international centers. This study is the first to be conducted in a private tertiary care hospital in Saudi Arabia.
Methods: This is a retrospective descriptive cohort study that reviewed the medical records of preterm infants admitted to the NICU at the international medical center, Jeddah, Kingdom of Saudi Arabia, between January 2014 and January 2020. We compared our results to the national data from King Faisal Specialist Hospital and Research Center-Riyadh (KFSH-R); King Abdulaziz Medical City-Jeddah and Riyadh (KAMC-J) and (KAMC-R), King Abdulaziz medical city Alhasa, the National Institute of Child Health and Human Development Neonatal Research Network (NICHD) and the Canadian neonatal network (CNN).
Results: A total of 92 preterm infants were included. 3, 8, 17, 17, 29, and 18 infants with a gestational age of 23 weeks, 24 weeks, 25 weeks, 26 weeks, 27 weeks, and 28 weeks, respectively. The mean gestational age was 25 weeks and 5 days. Fifty-four infants (58.7%) survived to hospital discharge. In terms of short-term outcomes, 13% had bronchopulmonbary dysplasia BPD, hemodynamically significant ductus arteriosus was present in 27 %, and retinopathy of prematurity ROP was found in 13 %, necrotizing enterocolitis NEC was diagnosed in 5.4 %, while late onset sepsis was reported in 23.9 % of infants.
Conclusion: In our population of our extreme premature infants, survival rates and complications of prematurity were comparable to national and international data. This data can be used as an add value cohort toward establishing country wide neonatal network to better plan regional resource allocation and utilization, facilitate ongoing audit, benchmarking and overall quality improvement initiatives.
Keywords: Infant; Newborn; Preterm; VLBW, Outcome; Survival; Saudi Arabia
Abbreviations: KSFH-R: King Faisal Specialist Hospital and Research Center-Riyadh; KAMC-J: King Abdulaziz Medical City-Jeddah; KAH-A : King Abdulaziz Medical City – Alhassa; IMC: International Medical Center, Jeddah; NICHD NRN: National institute of child health and human development neonatal research network; CNN: Canadian Neonatal Network; ADHD: Attention Deficit Hyperactivity Disorder; NEC: Necrotizing Enterocolitis; ROP: Retinopathy Of Prematurity; BPD: Bronchopulmonary Dysplasia; NICU: Neonatal Intensive Care Unit; NEC: Necrotizing Enterocolitis; RDS: Respiratory Distress Syndrome; PDA: Patent Ductus Arteriosus; ROP: Retinopathy Of Prematurity; NICU: neonatal Intensive Care Unit; WHO: World Health Organization; IMC: International Medical Center; IVH: Intraventricular Hemorrhage
Background
Premature birth is one of the leading causes of death in the world [1]. The global incidence of prematurity ranges from 5 to 11 percent of all births [1]. Some studies estimated the rate reaches 15 million preterm cases annually [2]. The highest rates occurred in Africa and North America [3]. A study found the prevalence of prematurity in the Eastern province of Saudi Arabia to be 7.5% [4]. Several factors have been associated to increase the risk of prematurity such as multiple gestations, history of preterm infants, uteroplacental insufficiency [5]. The infants born at 25 weeks of gestation or less had poor outcomes. The high mortality rates are caused by severe life-threatening complications such as intraventricular hemorrhage (IVH), necrotizing enterocolitis (NEC), retinopathy of prematurity (ROP), and bronchopulmonary dysplasia (BPD) [6-9]. These complications cause longer hospitalization, and neonatal intensive care unit (NICU) admissions. Complications that were caused by long term hospitalization include septicemia, growth failure, neurodevelopmental deficit, and low survival rates which are directly related to gestational age and birth weight [10,11]. Few studies discussed the outcomes and morbidities associated with extreme prematurity. A cohort study included 164 premature neonates with gestational age less than 26 weeks, 51% of these neonates needed mechanical ventilation, 10% had IVH, and the mortality rate was 20% [12]. A study that included 24 hospitals and more than 4500 neonates born before 22 weeks, the survival rate with no comorbidities was 3.4% [7].
A large cohort study that included 88327 infants born between 24-28 weeks of gestational age, the overall survival rate was 87%, with 64.1% and 93.7% survival rate at 24 weeks and 28 weeks of gestational age, respectively [13]. A cohort article illustrated poor short-term outcomes and morbidity such as IVH, BPD, and ROP [14]. Another local prospective study assessed the short- and long-term outcomes, concluded that more than 60% of extremely low birth weight infants died. Long term assessment of neurodevelopment showed higher risk of attention deficit hyperactivity disorder (ADHD), developmental delay, and hyperactivity autistic behavior [8]. The aim of this study was to assess the outcome of extremely preterm infants born below 29 weeks in our institution over the course of 6 years, with regard survival, and major short-term outcomes, and compare our results with 3 governmental national centers and 2 international networks, the national institute of child health and human development neonatal research network (NICHD NRN), and the Canadian neonatal network (CNN).
Materials and Methods
This study was a retrospective descriptive cohort study that reviewed the medical records of all inborn preterm infants admitted to the NICU at the international medical center (IMC), Jeddah, Kingdom of Saudi Arabia between January 2014 and January 2020. IMC is a private hospital with a total of 25 NICU beds including 13 level 3 beds. Total deliveries from 2014-2020 were 27417 out of which 3629 were admitted in the NICU. The following variables were recorded: gestational age, birth weight, gender, nationality, antenatal care, antenatal steroids, mode of delivery, status at the discharge, survival rates, length of neonatal stay in the NICU, respiratory distress syndrome (RDS), use of surfactant, bronchopulmonary dysplasia (BPD), use of oxygen at discharge, pneumothorax, patent ductus arteriosus (PDA), intraventricular hemorrhage (IVH), retinopathy of prematurity (ROP), necrotizing enterocolitis (NEC), sepsis, and fungal infection. Standard Neonatal medicine definitions were used to diagnose these variables. The World Health Organization (WHO) defines extremely preterm infants as infants born alive, before 28 weeks of gestational age. Also, they classified preterm infants according to the birth weight to very low birth weight (less than 1500g), and extremely low birth weight (less than 1000g) [15]. According to the National Institute of Child Health and Human Development Neonatal Research Network (NICHD-NRN) classification of extremely preterm infants were born between 22- 28 weeks of gestation and very low birth weight were infants with birth weight between 401g to 1500 g [16]. Thus, we included all preterm infants born at 23 to 28 weeks of gestational age and had extremely low birth weight. The exclusion criteria were patients who had chromosomal and congenital anomalies.
Variables and Definitions
Gestational age was determined either by the last menstrual period of the mother or the earliest ultrasound examination or both. Extremely preterm infants were defined as infants born alive, before 29 weeks of gestational age. Infants born with birth weight less than 1500g were considered as very low birth weight infants, and infants born with birth weight less than 1000g were considered as extremely low birth weight infants, according to the WHO classification [15,17,18]. Active care refers to managing the preterm neonate with one of the following: surfactant, epinephrine, intubation, chest compressions, mechanical ventilation, positive airway pressure, bag valve mask ventilation, or parenteral nutrition. While comfort care refers to not managing the preterm infant with any of the active care therapies and interventions. RDS was diagnosed based on the clinical finding and the features of RDS in chest x-ray, which include decrease in lung expansion, ground-glass or diffuse, reticular granular appearance, and air bronchogram in both lungs. BPD was diagnosed if an infant needs oxygen supplementation at 36 weeks postmenstrual age. Pneumothorax was diagnosed mainly if the chest radiograph revealed hyperlucency, air in the pleural space, and diminished vascular and lung marking. IVH mainly diagnosed with cranial ultrasound, the severity was determined by the location and extent of the hemorrhage. PDA was confirmed by echocardiography if there was a clinical suspicion of the disease. ROP was considered severe if surgery or laser intervention was performed. NEC diagnosis was clinically based on the characteristic finding of bilious vomiting, abdominal distention, and the presence of blood in the stool, in addition to the abdominal radiograph signs which include sentinel bowel, pneumoperitoneum, and pneumatosis intestinalis. Sepsis was diagnosed if there were positive cultures either from the blood or cerebrospinal fluid. If the sepsis occurred at the first three days of life, it was considered early-onset sepsis [19].
Statistical Analysis
We used descriptive analysis to assess the out- comes of the complications of prematurity. Continuous variables were summarized using mean and standard deviation, while categorical variables were summarized as frequency and percentages.
National and International Comparisons
We compared our survival rate by gestational age, as well as short-term morbidities to the following reported national and international published data:
Morbidities from the following centers were compared with our data:
i. National institute of child health and human development neonatal research network (NICHD NRN).
ii. Canadian neonatal network (CNN).
iii. King Faisal Specialist Hospital and Research Center- Riyadh.
iv. King Abdulaziz Medical City-Jeddah.
v. King Abdulaziz University Alhassa.
Mortalities from the following centers were compared with our data:
1. KSFH-R: King Faisal Specialist Hospital and Research Center-Riyadh
2. KAMC-J: King Abdulaziz Medical City-Jeddah.
3. KAH-A: King Abdulaziz Medical City – Alhassa.
4. IMC: International Medical Center, Jeddah.
5. National institute of child health and human development neonatal research network (NICHD NRN).
6. Canadian neonatal network (CNN).
7. Results
a. Demographics of infants
A total of 92 inborn preterm infants were included. The mean gestational age was 25 weeks and 5 days. The birth weight of more than half of the infants 62(67.4%) was less than 1000g. Fifty (54.3%) infants were males. A total of 36(39.1%) of the infants were a product of multiple gestation. Antenatal steroids were given to 60 out of 92 infants (65.2%). Detailed demographic data are reported in table 1.
b. Survival rates. morbidities and mortalities
Fifty-four infants (58.7%) survived hospital discharge. The mortality rate was 33.7 % in infants with a birth weight of less than 1000g, and 7.6% in infants with a birth weight between 1001g- 1499g. Approximately, two thirds of the total deaths were reported in male infants 24(26.1%), while in female infants the mortality rate was 14(15.2%). Survival rate by gestational age, with and without major morbidities is reported in table 2.
c. Short-term morbidities
Surfactant was used in 81(88%) infants, and BPD was documented in 13(14.1%) infants. NEC developed in 5(5.4%) infants, and 23(25%) infants were diagnosed with IVH and had grade III-IV of IVH (Tables 1-4).
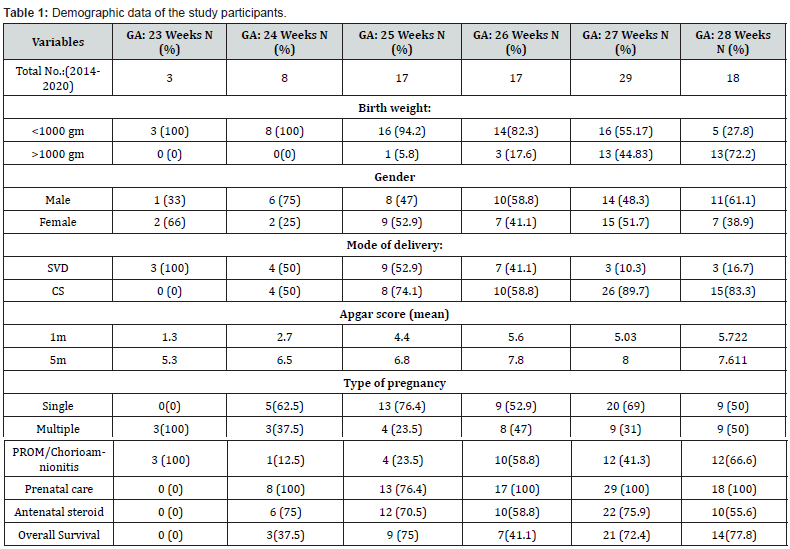
Abbreviations: Gm: grams, SVD: spontaneous vaginal delivery, CS: cesarean section.
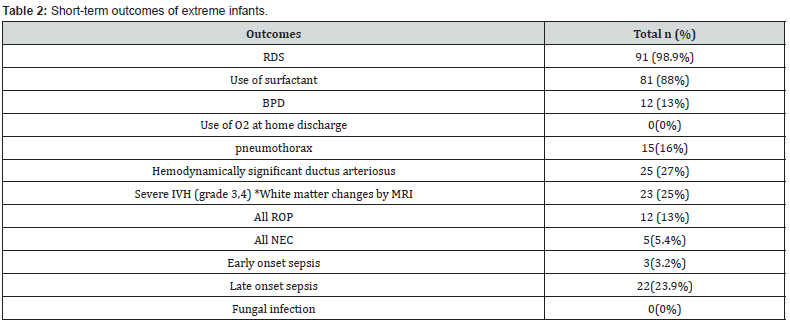
Abbreviations: RDS: respiratory distress syndrome, BPD: bronchopulmonary dysplasia, MV: mechanical ventilation, PDA: patent ductus arteriosus, ROP: retinopathy of prematurity, NEC: necrotizing enterocolitis, *White matter changes by MRI.
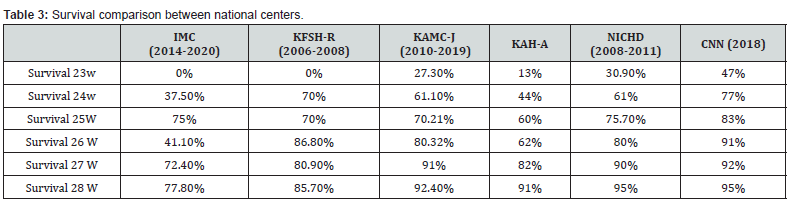
Abbreviations: KSFH-R: King Faisal Specialist Hospital and Research Center-Riyadh; KAMC-J: King Abdulaziz Medical City-Jeddah; KAH-A: King Abdulaziz Medical City – Alhassa; IMC: International Medical Center, Jeddah.
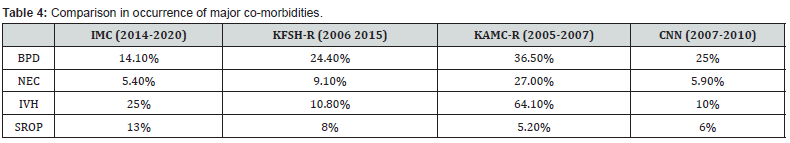
Abbreviations: KSFH-R: King Faisal Specialist Hospital and Research Center-Riyadh; KAMC-R: King Abdulaziz Medical City-Riyadh; IMC: International Medical Center, Jeddah.
Discussion
In this single-center study, we reported survival and short-term outcome of preterm infants born with gestational ages ranging from 23 to 28 GA from a private hospital. Preterm birth is defined as birth before 37 completed weeks gestation, and it is estimated that each day, across the world over 41,000 infants are born before this gestational age [20]. The prevalence of preterm and post-term birth in Saudi Arabia is like the prevalence in other high-income countries [21]. Survival rates in our cohort were highest for infants at the age of 28 weeks followed by 25 weeks. Meanwhile survival at 24 weeks was lower than the international figures. We do not have any surviving infants at 23 weeks gestation [6,8,18]. In terms of morbidities our center had the lowest rates of necrotizing enterocolitis (NEC). The values were better compared to both the national and international data [19]. Our study limitation is that it is a single-center study, so its results cannot be generalized to the whole country. The results of this study could serve as data for national trends for survival and in the short-term will be useful source at the institution level for family counselling incorporating informed patients’ preferences. In the future we hope that more national data will be available at different institutional and regional level in in addition further studies should be directed towards describing long-term outcomes of extremely preterm infants to provide standardized consensus guidelines regarding management approach of Extreme premature infants and facilitate unbiased and balanced family decision making.
Conclusion
In conclusion, we report the survival and incidence of shortterm complication of prematurity over a period of 7 years, which was comparable to the international data. This data can be used as an add value cohort toward establishing country wide neonatal network to better plan regional resource allocation and utilization, facilitate ongoing audit, benchmarking and overall quality improvement initiatives.
Declarations
d. Ethics approval and consent to participate.
An informed consent was obtained from all the participating individuals, all the participants had the right to withdraw from the study at any time.
e. Availability of data and material
Data supporting the findings of the study are available upon request from the corresponding author.
f. Authors contributions
All authors approve the final manuscript as submitted and agree to be accountable for all aspects of the work.
References
- Mandy GT, Weisman L, Kim M (2017) Incidence and mortality of the preterm infant. Massachusetts.
- Purisch SE, Gyamfi-Bannerman C (2017) Epidemiology of preterm birth. Semin Perinatol. 41(7): 387-391.
- Beck S, Wojdyla D, Say L, Betran AP, Merialdi M, et al. (2010) The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull World Health Organ 88: 31-38.
- Al-Qurashi FO, Yousef AA, Awary BH (2016) Epidemiological aspects of prematurity in the Eastern region of Saudi Arabia. Saudi Med J 37(4): 414.
- Goldenberg RL, Culhane JF, Iams JD, Romero R (2008) Epidemiology and causes of preterm birth. Lancet 371(9606): 75-84.
- Al Hazzani F, Al-Alaiyan S, Hassanein J, Khadawardi E (2011) Short-term outcome of very low-birth-weight infants in a tertiary care hospital in Saudi Arabia. Ann Saudi Med 31(6): 581-585.
- Rysavy MA, Li L, Bell EF, Das A, Hintz SR, et al. (2015) Between-hospital variation in treatment and outcomes in extremely preterm infants. N Engl J Med 372: 1801-1811.
- Abolfotouh MA, Al Saif S, Altwaijri WA, Al Rowaily MA (2018) Prospective study of early and late outcomes of extremely low birthweight in Central Saudi Arabia. BMC pediATR 18(1): 1-9.
- Horbar JD, Badger GJ, Carpenter JH, Fanaroff AA, Kilpatrick S, et al. (2002) Trends in mortality and morbidity for very low birth weight infants, 1991-1999. Pediatr 110(1): 143-151.
- Patel RM (2016) Short-and long-term outcomes for extremely preterm infants. Am J perinatal 33(03): 318-328.
- Fanaroff AA, Stoll BJ, Wright LL, Carlo WA, Ehrenkranz RA, et al. (2007) Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol 196(2): 147-e1.
- Mehler K, Grimme J, Abele J, Huenseler C, Roth B, Kribs A (2012) Outcome of extremely low gestational age newborns after introduction of a revised protocol to assist preterm infants in their transition to extrauterine life. Acta Paediatr 101(12): 1232-1239.
- Helenius K, Sjörs G, Shah PS, Modi N, Reichman B, et al. (2017) Survival in very preterm infants: an international comparison of 10 national neonatal networks. Pediatr 140(6): e20171264.
- Al Hazzani F, Al Alaiyan S, Jabr MB, Binmanee A, Shaltout M, et al. (2021) Decisions and outcome for infants born near the limit of viability. Int J Pediatr Adolesc Med 8(2): 98-101.
- Engle WA (2006) A recommendation for the definition of “late preterm” (near-term) and the birth weight–gestational age classification system. InSeminars in perinatology. WB Saunders 30(1): 2-7.
- Su BH, Hsieh WS, Hsu CH, Chang JH, Lien R, et al. (2015) Neonatal outcomes of extremely preterm infants from Taiwan: comparison with Canada, Japan, and the USA. Pediatrics & Neonatology 56(1): 46-52.
- Shah PS, Lui K, Sjo ̈rs G, Mirea L, Reichman B, et al. (2016) Neonatal outcomes of very low birth weight and very preterm neonates: An international comparison. J Pediatr 177: 144-152.
- Al-Alaiyan S, Al-Hazzani F (2009) The need for hospital-based neonatal palliative care programs in Saudi Arabia. Ann Saudi Med 29(5): 337-341.
- Regev RH, Lusky A, Dolfin T, Litmanovitz I, Arnon S, et al. (2003) Excess mortality and morbidity among small- for-gestational-age premature infants: A population-based study. J Pediatrics 143: 186-191.
- Platt MJ (2014) Outcomes in preterm infants. Public Health 128(5): 399-403.
- Fayed A, Wahabi HA, Esmaeil S, Elmorshedy H, AlAniezy H (2022) Preterm, early term, and post-term infants from Riyadh mother and baby multicenter cohort study: The cohort profile. Front Public Health 10: 928037.






























