High Dose Dexamethasone in Complicated Typhoid Fever: What Is the Evidence?
Zulquar Nain1*, Shaad Abqari1 and Shriyansh Kulshrestha2
1Department of Pediatrics, Jawaharlal Nehru Medical college, Aligarh Muslim University, Aligarh, Uttar Pradesh, India
2Department of Critical Care Medicine, Sanjay Gandhi Post-Graduate Institute, Lucknow, Uttar Pradesh, India
Submission:January 05, 2024;Published: January 17, 2024
*Corresponding author: Zulquar Nain, Department of Pediatrics, Jawaharlal Nehru Medical college, Aligarh Muslim University, Aligarh, Uttar Pradesh, India
How to cite this article: Zulquar N, Shaad A, Shriyansh K. High Dose Dexamethasone in Complicated Typhoid Fever: What Is the Evidence?. Acad J Ped Neonatol 2024; 13(3): 555920. 10.19080/AJPN.2024.13.555920
Questions:
i) Recommendation of using high dose (HD) dexamethasone in complicated enteric fever in the paediatric population from evidence-based systematic review(s) or meta-analysis?
ii) The ceiling dose of dexamethasone that would be prescribed in children, especially in adolescents.
1.1. Findings: The standard recommendation of giving a high dose of dexamethasone in severe typhoid fever, especially when complicated by neurological findings, lacks any systematic review or meta-analysis.
1.2. Meaning: High-dose dexamethasone should be considered as adjunctive therapy in severe cases of typhoid fever in pediatric patients, after careful consideration of the benefits and risks.
Abstract
Abstract
Importance and Objective: Severe typhoid fever can lead to neurological and systemic complications. This article reviews the evidence and rationale behind the recommendation of using dexamethasone, the maximum dose that can be given in such cases and compares the use of this high dose in other paediatric ailments.
Evidence Review: A literature review was done using PubMed with the keyword’s typhoid, enteric, dexamethasone, and paediatric. A few studies were also traced through the citation of recent papers, as they were not available in their original form in PubMed.
Findings: To date, no meta-analysis has proven the role of dexamethasone in complicated typhoid fever because of the lack of studies. Various studies have been conducted with their limitations to prove the efficacy of the regimen for severe typhoid fever. The recommendation is based on a single RCT, with its own limitations.
Conclusions and Relevance: No other study has supported this hypothesis. However, dexamethasone is still used as emergency rescue measure for patients with severe typhoid fever. This recommendation requires more robust support by incorporating trials enrolling large numbers of patients.
Keywords: Enteric Fever; Dexamethasone; Typhoid Fever; Pediatric; Inflammatory Syndrome
Abbreviations: HD: High Dose; ACTH: Adrenocorticotropic Hormone; MISC: Multisystem Inflammatory Syndrome in Children
Introduction
Typhoid fever is a tropical disease commonly encountered in countries with poor sanitation practices and a lack of access to pure water. This disease transmits mainly through the feco-oral route and is a major concern for morbidity among children in our country. Most of these cases are seen in outpatient departments and day-care settings, as they respond to oral antibiotics with rare complications. Furthermore, the irrational antibiotic prescription, especially in community settings, somehow decreased the incidence of morbidity associated with typhoid fever without even searching for laboratory evidence of the infection. If not treated promptly, the infection complicates itself over the course of the disease, leading to hospital admission and, rarely, mortality. The constellation of complications includes neurological manifestations, which are the most common, followed by gastrointestinal, haematological, bone and joint, respiratory, and cardiovascular manifestations [1]. Apart from timely and prompt administration of antibiotics, these complications can be abated conventionally by using steroids (usually I.V. HD dexamethasone) in very sick patients [2]. This article reviews the evidence and rationale behind the recommendation of using dexamethasone, the maximum dose that can be given in such cases and compares the use of this high dose in other paediatric ailments. The adverse effect of such a high dose of steroid for a very short period (<5 days) is debatable, as many adverse effects are not dose and duration-related. It is also to be noted that in cases of life-threatening situations, this dose of dexamethasone is imperative and given as a dire method, ignoring the adverse consequences. This is to bring to the kind attention of the pediatricians the dilemma of using very high doses of dexamethasone loading, especially in adolescents with a weight band of more than forty kilogram, without any background ceiling dose recommendations.
Methodology
A literature review was done using PubMed with the key-words typhoid, enteric, dexamethasone, and paediatric. A few studies were also traced through the citation of recent papers, as they were not available in their original form in PubMed. Rarely few reviews on the use of dexamethasone in various paediatric ailments have also been traced.
Review of Literature
Lewis and Page, 1949 (an animal-based study) [3]
Adrenalectomized rats were induced with typhoid toxin, and cortisone showed protective effects against the toxin's action.
Smadel and Jackson, 1951 (animal-based study) [4]
Investigating the anti-toxin action of cortisone and adrenocorticotropic hormone (ACTH) in normal mice inoculated with lethal amounts of the toxins of rickettsiae and Salmonella typhosa showed no protective effect.
Smadel and Ley 1951 (Case Control Study) [5]
Combined therapy with cortisone and an antibiotic (chloramphenicol) was superior to chloramphenicol alone in adults suffering from severe typhoid fever. Combined therapy resulted in a prompter clinical response than was previously observed with antibiotic treatment alone. Furthermore, patients (n=7) who received 300mg of cortisone on the first day had earlier defervescence of pyrexia as compared to patients who received 200mg of cortisone on the first day of treatment (mean febrile period of 15.5 hours vs 50.2 hours).
Wisseman 1953 (Case Control Study) [6]
Studied adults (18 patients) with typhoid fever and divided the study population into five groups. Group 1 received an average total dose of 10.7 mg/kg/day, while groups 2nd to 5th received an average total dose of 8.1 to 6.4 mg/kg/day of cortisone. The study also showed an escape phenomenon from cortisone, which was elaborated as the reappearance of fever, headache, and other toxic manifestations within 18-72 hours of illness. It was postulated that a given dose of cortisone may be less effective in controlling the febrile-toxic state on the third day than on the first day of treatment, resulting in the escape phenomenon. Bacteraemia control was quick in typhoid fever treated with the combined regimen and was comparable in all respects to cases treated with chloramphenicol alone. However, the incidences of relapse and of complications did not appear to be influenced by the inclusion of cortisone in the therapeutic regimen.
Woodward 1954 (Case Series) [7]
A case series of seven patients, including children ages 5, 7, and 11, had severe typhoid fever treated with chloramphenicol and cortisone. The adult dose was 200-300mg on day 1, followed by 200mg on day 2, and 100mg on day 3. The five-year-old kid (weight: 32.65 kilogrammes) received 450 mg (approximately equivalent to 14 mg of dexamethasone) over the course of four days. The seven-year-old kid (weight: 24.94 kilogrammes) received 300 mg (approximately equivalent to 10 mg of dexamethasone) over a similar course. The eleven-year-old kid (weight = 40.82 kilogrammes) received 450 mg (approximately equivalent to 14 mg of dexamethasone) over the same duration. (Conversion source: clinicalc.com) In all patients, there was definite bedside improvement within 24 hours, including fever, encephalopathy, and shock, irrespective of the severity of the illness at the time of beginning treatment. The article also mentioned a pregnant female with typhoid fever who had a milder presentation than expected. This raised the possibility that the patient was already enjoying a high degree of adrenal stimulation because of pregnancy and that this may have contributed to the mildness. However, the evidence lacked any laboratory confirmation. The researchers also concluded that the hormone produced symptomatic benefit for patients but did not show any antibacterial effect or hasten the disappearance of bacteria as seen through repeated cultures.
Woodward and Smadel, 1964 (Recommendations) [8]
A review article on the management of typhoid fever and its complications in adults concluded that steroids in enteric fever shorten the febrile stage, headache, and toxic signs. Cortisone, 200 to 300 mg daily, or prednisolone, 40 to 60 mg daily, is given for no more than 3 days, which is the appropriate dosing recommendation. These drugs were always to be administered along with chloramphenicol, and this combined therapy was indicated only for those patients with severe toxemia and pyrexia who might expire if the toxic febrile state is not brought under control promptly; it should not be used as a routine practice. The risk of intestinal hemorrhage due to steroids was also negated, as postulated in an older study [9]. Also, this steroid regimen should not be continued for more than three consecutive days.
Hoffmann 1984 and Punjabi 1988 (RCT) [2,10]
A landmark randomised controlled double-blind trial comprising twenty-eight patients (11 out of the 28 patients studied were under the age of 14 years) with complications of typhoid fever were included in the study. The intervention group (20 patients) received an initial dose of 3 mg of dexamethasone per kilogram, followed by eight doses of 1 mg per kilogram every six hours for a total treatment duration of 48 hours, while 18 patients received a placebo. The 10 percent case fatality rate in the dexa group was significantly lower than the 55.6 percent in the placebo group (p = 0.003). Hence, dexa-supportive therapy led to a reduction in the 45.6% case fatality rate as compared to placebo. A subsequent study, from the same group, included 15 additional children with severe typhoid fever who received dexamethasone in a nonrandomized fashion. Among the paediatric age group, the overall case fatality rate was 9.5% vs. 35% for the dexamethasone and non-dexamethasone groups, respectively [10]. It is worth noting that six of the 18 survivors in the dexa group (33%) had non-Salmonella bacteremia during hospitalization. The postulated mechanism was thought to be the suppression of monoclines, arachidonic acid and its metabolites, and free oxygen species from stimulated macrophages due to endotoxin release from the bacteria. This trial has been the basis for the standard recommendation of using dexamethasone in severe typhoid fever till date.
Rogerson, 1991 (RCT) [11]
Adult patients (n=41) with the case definition of severe typhoid fever were put in an intervention group by being given hydrocortisone 100 mg (for the first 23 patients) or 400 mg (for all subsequent patients) intravenously or intramuscularly every 6 hours for 12 doses. The data from the intervention group was compared with the hospital records of previously admitted patients with severe typhoid fever who did not receive any steroids. The team concluded that hydrocortisone had no effect on mortality in severe typhoid fever. This was in contrast with the previous Indonesian study [2] which implied that dexamethasone, which is about 15 and 20 times higher than the two hydrocortisone regimens, respectively, in glucocorticoid equivalents, decreased mortality. This incongruency led to the suggestion from the researchers to reduce the dosing of steroids from the previous recommendation made by Hoffman et al [2]. Also, it puts a question mark on the validity of the results from the previous study.
Girgisl 1993 (Case Series) [12]
A case series of using dexamethasone in the treatment of enteric fever complicated by cerebellar involvement. First case was of a fourteen-year-old male treated with dexamethasone (8 mg/dose) every 12 hours over 7 days, followed by tapering of the dose in the next week. Another similar case involved a 15-year-old patient who was given 12mg per dose of dexamethasone every 12 hours, and another involved a 13-year-old girl treated with 8mg every 12 hours of dexamethasone. The reduction of cerebral edema due to steroids was thought to be the reason for improvement in these cases of cerebellar complications of enteric fever.
7.10. Trevett, 1994 (correspondence) [13]
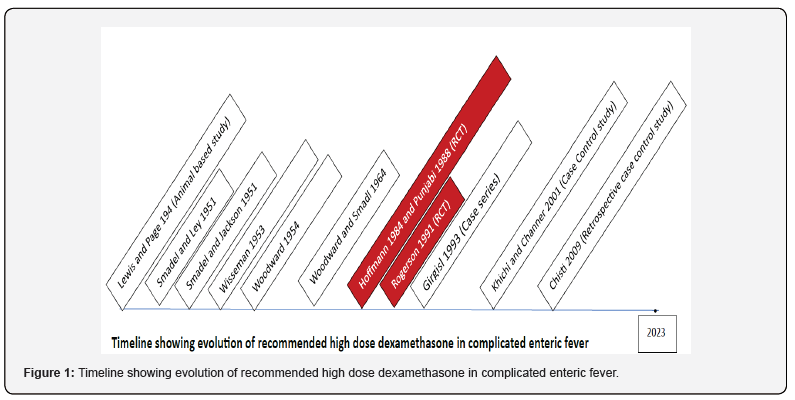
The author contradicts the standard recommendation of using dexamethasone as a part of therapy for neurological complications of severe typhoid fever in adult patients. Quoting other studies from the adult population, he concluded that only a few patients were treated with steroids along with antibiotics. The time course of the complications was comparable with that of the patients who did not receive any steroids. Also, the author indicates that the clinical features were not suggestive of cerebral edema in these patients, which is at odds with the belief that the steroids in these cases reduce cerebral edema (Figure 1).
Khichi and Channer (2001) (Case Control Study) [14]
Eighty-four culture-proven children with typhoid fever were randomly distributed into 2 groups; the first group received only chloramphenicol, while the other group received dexamethasone and chloramphenicol combination therapy. The dose of dexamethasone was 3 mg/kg stat, followed by 1.5 mg/kg intravenously every six hours. In the beginning, the time of defervescence was 52.5 days versus only 24 hours in combination therapy. The steroid group reported a 100% response within 24 hours. Three cases (7.14%) relapsed with fever within 24 hours of the stoppage of steroid therapy, which was not an uncommon finding as reported previously (the escape phenomenon) in an initial study [14].
Hosoglu 2009 (Case report) [15]
The author reported the positive effect of dexamethasone in a 21-year-old patient presented with massive enteric bleeding in typhoid fever. The patient received dexamethasone at 3mg/kg/day on the first day, followed by 2mg/kg/d, 1mg/kg/d and 0.5mg/kg/d over subsequent days.
Chisti & Bardhan 2009 (Retrospective case-control study) [16]
Twenty-three patients with a mean age of 17.5±5.3 months met the inclusion criteria and were assessed retrospectively about the administration of high-dose dexamethasone in encephalopathy associated with typhoid fever. Among the patients, 20 received steroids during their illness, while 3 patients received only antibiotics. The survivors were more likely to have received high-dose dexamethasone (100% vs. 0%, P < 0.001) and less likely to have hypoglycemia (6% vs. 67%, P = 0.045) versus patients who died.
Brosset 2016 (Case Report) [17]
The author reported a teenager with salmonella-induced septic shock and severe acute respiratory distress syndrome who started on high-dose dexamethasone at an initial dose of 3 mg/kg, followed by 1 mg/kg every 6 hours for a total of 48 hours. There was subsequent improvement, and the patient was weaned off from respiratory support and discharged later.
Laps 2020 (Case Report) [18]
It is a case report of a nine-year-old American male with a travel history to India who was diagnosed with typhoid fever-associated encephalopathy and treated with high-dose dexamethasone therapy at 1mg/kg every 6 hourly for 48 hours. Overall clinical improvement was seen within 48 hours of initiating dexamethasone therapy. The patient was discharged with a normal neurological examination.
Result and Discussion
The standard recommendation of giving a high dose of dexamethasone in severe typhoid fever, especially when complicated by neurological findings, lacks any systematic review or meta-analysis. The minimal randomised evidence from two trials [2] which was later disputed by another trial [11] in a tropical disease with a high incidence and a high rate of complications, is debatable. The trial by Hoffman et a. excluded the very high-risk randomized patients who died within 6 h, even though the trial specifically aimed to study high-risk patients. Based on subsequent results from blood and bone marrow culture came out to be typhoid fever these cases were excluded initially. In fact, 68 patients had been randomized in that trial, but only 38 were analyzed. For 2 of the 68 cases, it is not even stated which arm they were randomized to. For the other 66 patients, the death difference was not statistically significant (10 ⁄ 33 vs. 18 ⁄ 33, P =0.057). These data are over 25 years old, and this regimen has not been redemonstrated to be effective for adults or children in any recent or updated trials. The indication is also expanded in severe ARDS (COVID and non-COVID), septic shock, multisystem inflammatory syndrome, and other innumerable diseases where pulse therapy is the getaway for rapidly progressive inflammation. Adult studies in COVID with severe hypoxemia demonstrated that even 6mg/d sufficed to keep the patient without life support [19]. In children, there are reports showing recovery in multisystem inflammatory syndrome in children (MISC), the erstwhile pediatric inflammatory multisystem syndrome in temporal association with COVID-19, with dexamethasone administered at 0.2 mg/kg/d [20]. A dose of 27 mg/m2/d has been reported in a trial where dexamethasone was added to prevent chemotherapy induced nausea and vomiting in highly emetogenic therapies [21].
This high dose of dexamethasone has its own complications, even if it is given for a very short time (<5days). This includes hyperglycemia and neurobehavioral adverse effects [22]; the usual adverse effects like rash, hypersensitivity, and idiosyncratic reactions are also reported. With the increasing incidence of obesity, especially among teenagers, it is relevant to discuss the maximum dose that can be given, even if the clinicians follow the standard recommendation. The evidence of using high dose dexamethasone misses this important clinical aspect encountered at bedside. It is a point of discussion among the clinicians when dexamethasone in the dosage of 120mg is prescribed to a 40-kilogram weight teenager and 15 vials of dexamethasone are used (one vial of dexamethasone that is usually marketed contains 8mg of drug). In precedence, a retrospective review of lower-dose dexamethasone uses in severe typhoid fever showed no survival benefit, suggesting that a strong anti-inflammatory effect provided at higher doses is required [11]. If the usual mechanism postulated in treating the complication of typhoid fever involves inhibition of the acute inflammatory cascade, can this steroid regimen be used in other gram-negative sepsis or is this effect of dexamethasone is only limited to the toxin of Salmonella?
Conclusion
Younger adults have greater neuropsychiatric morbidity during typhoid fever than older adults, which highlights the importance of initiating corticosteroid treatment before patients decompensate [23] and delays in steroid administration may lead to increased mortality or relapse [24]. Hence, dexamethasone is not needed for most patients with typhoid fever but is still recommended for those who are delirious, obtunded, stuporous, comatose, or in shock, for whom this intervention may be lifesaving. Despite the limited data on safety and efficacy, high-dose dexamethasone should be considered as adjunctive therapy in severe cases of typhoid fever in pediatric patients, after careful consideration of the benefits and risks. Many case reports describe the management of severe typhoid fever with the standard recommendation of using dexamethasone in encephalopathy. These cases have improved with dexamethasone administration. It is a challenge for future trials as the culture results are unknown at the time of randomization in a setting with life-threatening complications where urgent intervention is sought. In an ideal condition, patient tailored treatment is needed, and evaluation of the baseline cortisol level is pre-emptive to guide dexamethasone-based therapy in these patients. Robust clinical trials with many participants are needed to further strengthen the recommendations.
Disclosure
A short summary of this review has been published in some correspondence.
References
- Iftikhar A, Bari A, Jabeen U, Bano I (2018) Spectrum of complications in childhood Enteric Fever as reported in a Tertiary Care Hospital. Pak J Med Sci 34(5): 1115-1119.
- Hoffman SL, Punjabi NH, Kumala S, Moechtar MA, Pulungsih SP, et al. (1984) Reduction of mortality in chloramphenicol-treated severe typhoid fever by high-dose dexamethasone. N England J Med 310(2): 82-88.
- Lewis LA, Page IH (1949) Studies on the protective power of adrenal extract and steroids against bacterial toxins in adrenalectomized rats. Ann N Y Acad Sci 50(6): 547-551.
- Jackson EB, Smadel JE (1951) The Effects of Cortisone and ACTH on Toxins of Rickettsiae and Salmonella Typhosa. J Immunol 66(5): 621-625.
- Joseph Smadel BE, Ley HL, Diercks FH (1951) Treatment of typhoid fever. I. Combined therapy with cortisone and chloramphenicol. Ann Intern Med 34(1): 1-9.
- Wisseman Cl, Paterson PY, Smadel JE, Diercks FH, Ley Hl (1954) Studies on cortisone and antibiotics for prompt therapeutic control of typhoid fever and scrub typhus. J Clin Invest 33(2): 264-275.
- Woodward TE, Hall He, Dias-Rivera R, Hightower JA, Martinez E, et al. (1951) Treatment of typhoid fever. II. Control of clinical manifestations with cortisone. Ann Intern Med 34(1): 10-19.
- Woodward TE, Smadel JE (1964) Management of typhoid fever and its complications. Ann Intern Med 60: 144-157.
- Rowland HA (1961) The Complications of Typhoid Fever. J Trop Med Hyg 64(6): 143-152.
- Punjabi NH, Hoffman SL, Edman DC, Sukri N, Pulungsih SP, et al. (1988) Treatment of severe typhoid fever in children with high dose dexamethasone. Pediatr Infect Dis J 7(8): 598-600.
- Rogerson SJ, Spooned VJ, Smith TA, Richens, Base J (1991) Hydrocortisone in chloramphenicol-treated severe typhoid fever in Papua New Guinea. Trans R Soc Trop Med Hyg 85(1): 113-116.
- Girgisl NI, Faridl Z, Sultan2 Y, Hibbsl RG (1993) Use of dexamethasone in treatment of enteric fever complicated by cerebellar involvement. Trans R Soc Trop Med Hyg 87(6): 690-691.
- Andrew Trevett (1994) Transactions of The Royal Society of Tropical Medicine and Hygiene. RSTMH 88(3): 364.
- Khichi Q, Channer M (2001) Parenteral chloramphenicol versus chloramphenicol plus dexamethasone in the treatment of typhoid fever. Pak Pediatr J 25(2): 55-58.
- Hosoglu S, Ustun C, Geyik MF (2009) The efficacy of dexamethasone treatment in massive enteric bleeding in typhoid fever. Trop Doct 39(1): 53-54.
- Chisti Mohammod J, Bardhan PK, Sayeed H, Wasif Ali K, Ali Miraj K, et al. (2009) High-dose intravenous dexamethasone in the management of diarrheal patients with enteric fever and encephalopathy. Southeast Asian J Trop Medi Public Health 40(5): 1065-73.
- Brosset Ugas M, Carroll T, Kovar L, Chavez-Bueno S (2016) Salmonella typhi-induced septic shock and acute respiratory distress syndrome in a previously healthy teenage patient treated with high-dose dexamethasone. J Investig Med High Impact Case Rep 4(2).
- Laps AM, Foster CB, Laurens MB (2020) High-dose Dexamethasone in a Child with Enteric Encephalopathy Caused by Salmonella enterica serovar Typhi. Pediatr Infect Dis J 39(5): 49-51.
- Munch MW, Myatra SN, Vijayaraghavan BKT, Saseedharan S, Benfield T, et al. (2021) Effect of 12 mg vs 6 mg of Dexamethasone on the Number of Days Alive without Life Support in Adults with COVID-19 and Severe Hypoxemia: The COVID STEROID 2 Randomized Trial. JAMA 326(18): 1807-1817.
- Meena P, Pallavi, Mishra D, Jhamb U, Aggarwal M (2021) Low-Dose Dexamethasone Following IVIG in Pediatric Inflammatory Multisystem Syndrome in Temporal Association with COVID-19 (PIMS-TC). Indian J Pediatr 88(3): 301-302.
- Bakhshi S, Batra A, Biswas B, Dhawan D, Paul R, et al. (2015) Aprepitant as an add-on therapy in children receiving highly emetogenic chemotherapy: a randomized, double-blind, placebo-controlled trial. Supportive Care in Cancer 23(11): 3229-3237.
- Warris LT, Van Den Akker ELT, Aarsen FK, Bierings MB, et al. (2016) Predicting the neurobehavioral side effects of dexamethasone in pediatric acute lymphoblastic leukemia. Psychoneuroendocrinology 72: 190-195.
- Leung DT, Bogetz J, Itoh M, Ganapathi L, Pietroni MAC, et al. (2012) Factors associated with encephalopathy in patients with Salmonella enterica serotype typhi bacteremia presenting to a diarrheal hospital in Dhaka, Bangladesh. American Journal of Tropical Medicine and Hygiene 86(4): 698-702.
- Cooles P (1986) Adjuvant steroids and relapse of typhoid fever. J Trop Med Hygiene 89(5): 229-231.






























