A Case of Proteinuria in A Growth Restricted Preterm
Sruthi Nair1, Sai kiran Deshabotla2*, Venkatakeshwarlu varadhelli2 and Tejo Pratap Oleti1
1Head of the Department, Department of Neonatology, Fernandez hospital, India
2Consultant Neonatologist, Fernandez hospital, India
Submission: December 06, 2023; Published: January 03, 2024
*Corresponding author: Sai kiran Deshabotla, Consultant Neonatologist, Fernandez hospital, India
How to cite this article: Sruthi N, Sai kiran D, Venkatakeshwarlu v, Tejo Pratap O. A Case of Proteinuria in A Growth Restricted Preterm. Acad J Ped Neonatol 2024; 13(3): 555918. 10.19080/AJPN.2024.13.555918
Abstract
Background: A growth restricted preterm infant presented with ascites at 4 weeks of age.
Case: A 29-week male infant with features of intrauterine growth restriction was born by emergency cesarean section in view of Doppler compromise in utero with birth weight of 800 g. Antenatal history was suggestive of early onset of fetal growth restriction noted at 28 weeks of gestation. On the 30th day of life, bilateral hydrocele along with ascites and bilateral inguinal hernia was noted which progressively worsened. There were no clinical features of coagulopathy, encephalopathy or shock.
Intervention: Evaluation was suggestive of postnatal CMV infection, hence was treated for the same.
Conclusion: Cytomegalovirus infection can have varied presentations. Hence with the background of growth restriction, cytomegalovirus infection must be considered. The consent has been obtained from the patient for representation of case report and the confidentiality of the patient has been maintained.
Keywords: Intrauterine Growth Restriction; Proteinuria; Cytomegalovirus (CMV) Infection; Oligohydramnios or polyhydramnios; Nephrotic syndrome
Abbreviations: CMV: Cytomegalovirus; PCR: Polymerase Chain Reaction
Case Report
29-week male infant was born by emergency cesarean section in view of doppler compromise in utero with birth weight of 800 g (7th percentile on Fenton chart) and head circumference of 24 cm (3rd percentile on Fenton chart). Mother was a 33-year-old primi gravida. The couple was a 3rd consanguineous couple. She had a history of treatment with anti-tubercular medication 10 years prior to the conception. She conceived this pregnancy after an in vitro fertilization procedure with donor egg and sperm from her partner. There was no history of gestational hypertension, gestational diabetes and autoimmune disorders. The serology for HIV and syphilis was negative. There was no history of smoking, tobacco use or substance abuse in the mother. The first trimester screening and targeted imaging for fetal anomalies were normal. There was no history of oligohydramnios or polyhydramnios.
Her antenatal history was suggestive of early onset of fetal growth restriction noted at 28 weeks of gestation. Antenatally steroid and magnesium sulphate were given to the mother to improve the neonatal outcome. The APGAR score was 7/9/9 at 1,5,10 minutes respectively. In view of fetal growth restriction placenta was sent for histopathology. On gross examination placenta appeared normal. The histopathology of placenta was suggestive of features of hypoxia/maternal vascular malperfusion. There was no dysmorphism noted. Initial course in neonatal intensive care unit was suggestive of transient tachypnea of newborn for which baby received respiratory support for 3 days. The hemogram performed after birth was normal. On day 7 of life the baby had features of sepsis. Blood culture was suggestive of Coagulase negative staphylococcal sepsis for which treatment was given with appropriate antibiotics. Meningitis was ruled out by CSF analysis. Oral feed was started on day 2 of life and baby reached full feeds on day 7. Total parenteral nutrition was given for 6 days and fed fortification was started on day 10 of life to provide adequate calories and protein. Baby regained birth weight on day 11 of life. On the 30th day of life, bilateral hydrocele along with ascites and bilateral inguinal hernia was noted. There was poor weight gain noted from the 4th week of life. There were worsening ascites over the period of next one week and hepatosplenomegaly was also noted. Due to massive ascites the baby developed respiratory distress for which respiratory support was restarted. The chest X-ray done at this point of time was normal. Screen echocardiography performed revealed good cardiac function. There were no clinical features of coagulopathy, encephalopathy or shock. The stool colour was monitored which was normal. Serial sugars monitored were normal.
Differential Diagnosis
1. Hypothyroidism
2. Urinary tract infection
3. Tubulopathy
4. Congenital nephrotic syndrome
5. Intrauterine infection- CMV
6. Portal vein thrombosis
7. Sepsis
Further Course and Diagnosis
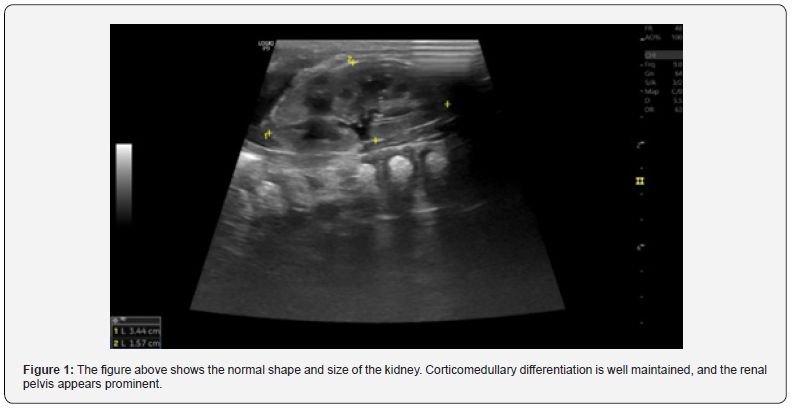
The hemogram and liver function test performed was suggestive of anemia and hypoalbuminemia respectively. There was no hepatitis or cholestasis noted. Anemia was corrected with packed cell volume transfusion. Urine analysis was normal. There was no hypertension noted on serial blood pressure monitoring. Hypoalbuminemia was corrected with albumin transfusion (Figure 1). Despite the treatment of hypoalbuminemia ascites persisted. Expanded newborn screening done was normal. The thyroid function test done was normal. Ascitic fluid tap was done analysis of which was transudative in nature. Under a presumed diagnosis of congenital nephrotic syndrome, baby was further evaluated with 24-hour urinary protein which was suggestive of nephrotic range proteinuria (>4mg/kg/hour). However, to confirm the diagnosis whole exome sequence was sent which was normal. In view of poor weight gain, worsening ascites and hepatosplenomegaly with antenatal history suggestive of early onset fetal growth restriction, cytomegaloviral infection was considered as a secondary cause on nephrotic syndrome, hence urine cytomegalovirus (CMV) qualitative assessment was done which was positive. Following the initiation of treatment of CMV infection with valgancyclovir, ascites resolved within 9 days. Hence the diagnosis of secondary nephrotic syndrome due to CMV infection was considered. Fundus examination showed no evidence of chorioretinitis. Neurosonogram performed was normal. The neonate got discharged at 36 weeks of corrected age on oral valgancyclovir. During treatment with valgancyclovir baby was monitored for its potential adverse effects as and when indicated. Currently the baby is asymptomatic and thriving well. The hearing screening done on follow up was normal.
Discussion
Nephrotic syndrome is a relatively rare disorder that may be caused by several diseases. The congenital variant manifests within the first 3 months of life. The presence of placentomegaly (i.e., placental weight >25% of the newborn weight) can point towards the genetic etiology of nephrotic syndrome. The prognosis of nephrotic syndrome secondary to genetic etiology is grave with high mortality rate within the first 6 months of life and most of the neonates are stillborn. Intrauterine infections have been frequently implicated as one of the etiological factors for secondary congenital nephrotic syndrome. However, CMV-related nephrotic syndrome is extremely rare. Nephrotic syndrome of infectious aetiology responds to specific treatment and does not require treatment with corticosteroids, while genetic forms tend to be steroid resistant and respond poorly to immunosuppressive agents and have grave prognosis. In our case, there was resolution of the symptoms after initiation of treatment of the CMV infection. Clinical manifestations of CMV infection can vary as it can be asymptomatic or associated with fever, respiratory tract infection, hepatosplenomegaly or loose stools.
The diagnosis of CMV is based on polymerase chain reaction (PCR), histopathological features and serological analysis. In our case the diagnosis was made on the basis of qualitative urinary CMV PCR analysis. The diagnosis of CMV by PCR is more reliable because findings can be quantified and response to treatment monitored. Low CMV DNA (5000 copies/mL) may suggest the development of end-stage organ disease [1]. In CMV congenital nephrotic syndrome, CMV-specific IgM antibodies are positive in 20–70% of infected newborns; however, if CMV is positive beyond 2-3 weeks of age, it could also be owing to postnatally acquired infection, such as through breast-milk [2,3]. The mechanism of CMV-induced glomerular injury and podocytopathy is ill defined. However, some studies imply that tissue injury is caused directly by the virus, that the insult is mediated by the T-cell response, and that the immune complex is formed because of the insult [4]. CMV infection can co-exist with mutational defects, and antiviral therapy is still indicated for extrarenal manifestations of CMV. Sinha et al describes that concomitant genetic mutations are present in significantly large number (23%) of the patients with CNS [5]. Since in our case the whole exome sequencing was normal, the genetic cause of congenital nephrotic syndrome could be ruled out. It has been postulated that CMV can directly injure the kidney tissue as well as trigger an immune response that leads to kidney damage [6]. Treatment of CMV nephrotic syndrome includes initial intravenous ganciclovir for up to 8 weeks, then changed to oral valganciclovir 30 mg/kg in two divided doses for at least 6 weeks which can be extended up to 6 months.
Lessons for the Clinician
1. Nephrotic syndrome may be the sole manifestation of CMV disease.
2. Genetic analysis is crucial to exclude congenital nephrotic syndrome, signifying the importance of timely and complete diagnostic workup.
Even though the role of 24-hour urinary protein needs to be explored in neonates, the results can give a clue for further evaluation.
References
- Kraft CS, Armstrong WS, Caliendo AM (2012) Interpreting quantitative cytomegalovirus DNA testing: understanding the laboratory perspective. Clin Infect Dis 54(12): 1793-1797.
- Revello MG, Gerna G (2002) Diagnosis and management of human cytomegalovirus infection in the mother, fetus, and newborn infant. Clin Microbiol Rev15(4): 680-715.
- Schleiss MR (2006) Acquisition of human cytomegalovirus infection in infants via breast milk: natural immunization or cause for concern? Rev Med Virol 16(2): 73-82.
- Stańczyk M, Tkaczyk M (2015) Nephrotic syndrome secondary to cytomegalovirus infection in an infant. Case report. Pediatr Med Rodz 11(2): 215-219.
- Sinha R, Vasudevan A, Agarwal I, Sethi SK, Saha A, et al. (2020) Congenital Nephrotic Syndrome in India in the Current Era: A Multicenter Case Series. Nephron144(1): 21-29.
- Platt JL, Sibley RK, Michael AF (1985) Interstitial nephritis associated with cytomegalovirus infection. Kidney Int 28(3): 550-552.






























