Neonatal Outcomes by Pandemic Wave Among Pregnant Individuals with COVID-19 Infection
Julia M. Moyett, MS1*, Amanda M. Craig MD2, Colleen Judge-Golden MD, PhD2, Khaila Ramey-Collier BS1, Brenna L. Hughes MD, MSc2 and Sarah K. Dotters-Katz MD2
1Duke University School of Medicine; Durham, NC, USA
2Division of Maternal Fetal Medicine, Department of Obstetrics and Gynecology, Duke University Health System, Durham, NC, USA
Submission:January 10, 2023; Published:February 24, 2023
*Corresponding author:Julia M. Moyett, MS, 2608 Erwin Road, Suite 210, Durham, NC 27705, Tel: 919-668-7426
How to cite this article:Julia M. Moyett, MS, Amanda M. Craig MD, Colleen Judge-Golden MD, PhD, Khaila Ramey-Collier BS, Brenna L. Hughes MD, MSc, et al. Neonatal Outcomes by Pandemic Wave Among Pregnant Individuals with COVID-19 Infection. Acad J Ped Neonatol 2023; 12(2): 555895. 10.19080/AJPN.2023.02.555895
Abstract
Background:The impact of COVID variants on neonatal outcomes is not well understood. The objective of this study is to compare neonatal outcomes by wave of the pandemic.
Materials and methods: Single center retrospective cohort of neonates born to individuals infected with COVID in pregnancy from 3/2020-2/2022. Primary outcome was a neonatal composite of NICU admission, intubation/CPAP, NEC, IVH, sepsis, and death. Secondary outcomes included components of composite. Outcomes were compared between pandemic “waves,” including wildtype (WT) (5/2020-9/2020), alpha (11/2020-3/2021), delta (8/2021-10/2021), omicron (12/2021-2/2022).
Results:Of 527 pregnant individuals, 133 (25.3%) were infected with WT, 99 (18.8%) with alpha, 62 (11.8%) with delta, and 157 (29.8%) with omicron. Maternal race and ethnicity, insurance status, and symptomatic COVID differed by wave. Gestational age at delivery, mode of delivery, and IAI did not differ. Neonatal composite was similar across waves (Table), as were secondary neonatal outcomes. No neonates were infected with COVID. When controlling for race and ethnicity, insurance status, symptomatic COVID, cesarean delivery, vaccination, and gestational age at delivery, neonates in alpha, delta, and omicron waves had lower odds of adverse outcomes and NICU admission compared to those born to individuals infected with COVID during WT wave.
Conclusion: Odds of adverse neonatal outcome and NICU admission were lower among those born in the alpha, delta, and omicron waves compared to those born in WT wave.
Keywords: COVID-19, neonatal outcomes, viral variants
Introduction
Pregnancy is associated with increased risk for severe COVID-19 and higher rates of maternal morbidity and mortality [1]. Neonatal infections are less common, thus data are sparse investigating perinatal transmission, as well as the impact of severe maternal infection on neonatal outcomes. Maternal disease severity varied across pandemic waves for all populations, yet limited data exist on neonatal morbidity and mortality across viral variants [1]. This study aims to describe neonatal outcomes by COVID-19 pandemic waves.
Materials and Methods
Retrospective cohort study of pregnant individuals delivered in single healthcare system (3/2020-2/2022) performed after IRB approval (Pro00105162). Individuals included if diagnosed with COVID-19 infection with positive PCR or antigen test at any point during pregnancy. Demographic information, pregnancy, delivery, neonatal, COVID-19 infection, and vaccination details were abstracted from the electronic medical record (EMR).
The primary outcome was a neonatal composite including neonatal intensive care unit (NICU) admission, intubation or continuous positive airway pressure (CPAP) therapy, necrotizing enterocolitis (NEC) (grade 2/3), intraventricular hemorrhage (IVH) (grade 3/4), sepsis, and death. Secondary outcomes included individual components of the composite, and neonatal SARS-CoV-2 infection. The exposure of interest was pandemic “wave.” Pandemic waves were defined using Department of Health and Human services data to identify community peaks in Durham County, North Carolina [2]. Waves defined as wildtype (5/2020-9/2020), alpha (11/2020-3/2021), delta (8/2021-10/2021), and omicron (12/2021-2/2022). Individuals with infections between defined waves were excluded. Bivariate statistics used to analyze the data, with regression models used to control for potential confounders identified using p<0.05 on univariate analysis.
Results
Five-hundred twenty-seven pregnant individuals were included. One-hundred thirty-three (25.3%) patients were infected with wildtype, 99 (18.8%) with alpha, 62 (11.8%) with delta, and 157 (29.8%) with omicron. Maternal race and ethnicity, insurance status, and symptomatic COVID-19 differed by wave. Gestational age at delivery, mode of delivery, and intraamniotic infection did not differ by wave (Table1).
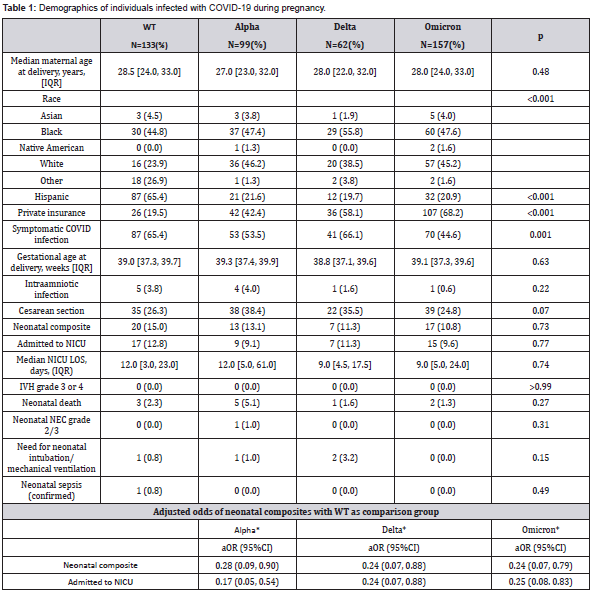
WT, wildtype wave; IQR, inter-quartile range; LOS, length of stay
*controls for race, ethnicity, insurance status, intraamniotic infection, cesarean delivery, vaccination status, and gestational age at delivery.
Neonatal composite did not differ between waves (p=0.73), nor did secondary neonatal outcomes (Table 1). Median NICU length of stay was 12 days for wildtype (IQR:3,23) and alpha (IQR:5,61) waves and 9 days for delta (IQR:4.5,17.5) and omicron (IQR:5,24) (p=0.77). Overall, neonatal NEC occurred in one neonate, neonatal intubation in four neonates, and death in 11. No neonates tested positive for SARS-CoV-2, had IVH grade 3 or 4, or had confirmed cases of sepsis. In adjusted analyses, neonates born to individuals with COVID-19 infection during pregnancy had lower odds of composite adverse outcome during the alpha (adjusted odds ratio (aOR) 0.28, 95% confidence interval (CI:0.09,0.90)), delta (aOR 0.24, 95%CI:0.07,0.88), and omicron (aOR 0.24, 95%CI:0.07,0.79), when compared to those born to individuals infected during wildtype wave. Neonates had lower odds of being admitted to the NICU during alpha (aOR 0.17, 95%CI:0.05,0.54), delta (aOR 0.28, 95%CI:0.09,0.95), and omicron (aOR 0.25, 95%CI:0.08,0.83) when compared to those born to individuals infected during the wildtype.
Discussion
In this population, neonates born to individuals following COVID-19 infection in pregnancy had higher risk of adverse neonatal outcome in the wildtype wave compared to alpha, delta, or omicron pandemic waves. This is consistent with the illness severity observed for the general population in the wildtype wave. Interestingly, neonatal outcomes were not worse during the delta wave, despite increased maternal disease severity in that wave [3]. This is also consistent with recent findings that the omicron wave was associated with reduced risk of maternal and neonatal outcomes in intensive care unit admission, preterm birth, and low birth weight [4].
This study is limited by several factors. We only included individuals who delivered in a single health system in the Southeast United States, limiting generalizability. Additionally, individuals who fell outside of our specifically defined waves were excluded. While we adjusted for vaccination status in our analyses, we did not look at impact of vaccination status on neonatal outcomes. Recent studies into safety of COVID-19 vaccination are reassuring for low risk of adverse neonatal outcomes following vaccination during pregnancy [5]. Lastly, we did not assess long-term infant adverse outcomes. Despite these limitations, our findings emphasize the importance of understanding neonatal impacts by wave as we anticipate ongoing COVID-19 variants, as well as the potential need for long term follow-up in neonates born to individuals with COVID-19.
Conflict of Interest
The authors report no conflicts of interest. Julia Moyett was awarded a Travel Scholar grant by the Infectious Diseases Society for Obstetrics & Gynecology to attend the 2022 annual meeting where this data was presented in preliminary form.
References
- Alefishat E, Jelinek HF, Mousa M, Tay GK, Alsafar HS (2022) Immune response to SARS-CoV-2 variants: A focus on severity, susceptibility, and preexisting immunity. J Infect Public Health 15(2): 277-288.
- Adhikari EH, MacDonald L, SoRelle JA, Morse J, Pruszynski J, et al. (2022) COVID-19 Cases and Disease Severity in Pregnancy and Neonatal Positivity Associated with Delta (B.1.617.2) and Omicron (B.1.1.529) Variant Predominance. JAMA 327(15): 1500-1502.
- Adhikari EH, SoRelle JA, McIntire DD, Spong CY (2022) Increasing severity of COVID-19 in pregnancy with Delta (B.1.617.2) variant surge. Am J Obstet Gynecol 226(1): 149-151.
- Yamaguchi T, Makino Y, Mabuchi Y, Okuda K, Hayashi H, et al. (n/a) Severity of SARS-CoV-2 infection in pregnant women and their neonates during the Omicron period compared to the pre-Omicron period: A retrospective cohort study. Journal of Obstetrics and Gynaecology Research doi:10.1111/jog.15610.
- Ding C, Liu Y, Pang W, Zhang D, Wang K, Chen Y. Associations of COVID-19 vaccination during pregnancy with adverse neonatal and maternal outcomes: A systematic review and meta-analysis. Front Public Health. 2023;11:1044031. doi:10.3389/fpubh.2023.1044031






























