Congenital Multilocular Pancreatic Cyst Originating from Head and Body of The Pancreas: A Challenging Diagnosis and Successful Total Cyst Excision
Mohamed Gaber Elsayed*
Jazan University, Faculty of Medicine, Department of Surgery, Saudi Arabia
Submission: February 13, 2023; Published: February 24, 2023
*Corresponding author: Mohamed Gaber Elsayed, Jazan University, Faculty of Medicine, Department of Surgery, Saudi Arabia
How to cite this article:Mohamed Gaber Elsayed. Congenital Multilocular Pancreatic Cyst Originating from Head and Body of The Pancreas: A Challenging Diagnosis and Successful Total Cyst Excision. Acad J Ped Neonatol 2023; 12(3): 555894. 10.19080/AJPN.2023.12.555894
Abstract
Congenital true pancreatic cysts are seldom findings among other abdominal cysts in children. Diagnosis can be delayed for a few months after birth until the infant presents with an abdominal mass, abdominal distension, or vomiting due to gastric outlet obstruction, total excision of the cyst is the treatment of choice but this is not always feasible. In this article, we report a 3-month -old boy with histologically proven true pancreatic cyst. The cystic mass was located in the right upper quadrant of the abdomen, and total cystectomy was performed without complication.
Keywords: Congenital; Pancreatic cyst; Pancreatic pseudocyst; Infant; total cystectomy
Introduction
Congenital pancreatic cysts may be coincide with systemic diseases or other inherited conditions such as von HippelLindau syndrome, polycystic kidney disease, Ivemark syndrome, trisomy 13 and trisomy 15 [1]. A congenital pancreatic cyst should be thought of if the fetus has an abdominal cyst without a definite origin. Early diagnosis with evaluation of the accompanying disease is required and significant to prevent fatal complications such as cholangitis, pancreatitis, cyst rupture, and peritonitis [1,2].
Case Presentation
A 3-month-old boy was admitted to our institution with an abdominal distention and non-bilious vomiting. This was present since birth but increased significantly 1 week prior to admission. On the physical examination a large, soft, non-tender epigastric mass was palpable. Laboratory studies were within normal range except for slightly elevated level of serum amylase which was 115 IU/ml (normal: 30-110). The abdominal ultrasound (AUS) study showed right upper cystic mass with well-defined walls, measuring 9 x 10 cm. The body of the pancreas was not visualized. Abdominal computed tomography (CT) and Magnetic resonance imaging (MRI) showed a thick wall cystic swelling about 7x 8 x 9 cm seen mainly in the right side of the abdomen extending from the anterior abdominal wall towards the right kidney. The pancreatic head is distorted by the swelling with no communication to the biliary system or pancreatic duct. The swelling displacing the transverse colon and the adjacent bowel loops inferiorly and to the left.
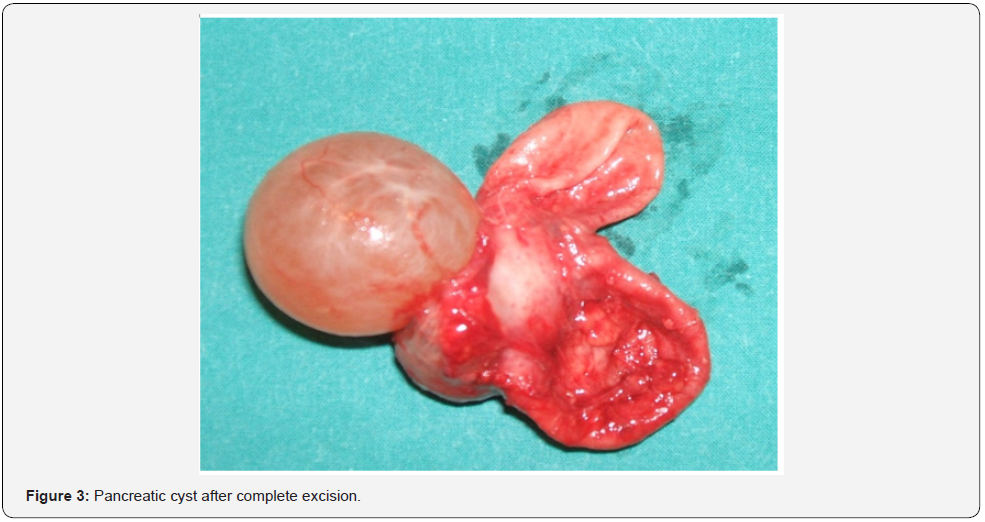
Patient underwent laparotomy through right supraumbilical transverse abdominal incision; which revealed a giant, retroperitoneal multilocular cyst originating from head and body of the pancreas (Figure 1). It was completely excised after being dissected from the pancreas going through its full length within the pancreatic tissue (Figure 2,3).


Postoperative course was uneventful, and the patient was sent home 5 days after the operation, with a serum amylase of less than 30 IU/ml. Follow up for six months after surgery showed that routine physical examination and laboratory investigations were normal and baby has continued on normal feeds and bowel motion.
The histology of the specimen showed multilocular cyst 7cm x 8cmx 9cm in size (Figure 2). The cyst contained 500 ml of serous, clear fluid with an amylase level of 300 IU/ml. The cyst wall consisted of dense, fibrous connective tissue lined by a few epithelial cuboidal cells and there was no communication with the pancreatic duct.
Discussion
Symptoms of pancreatic lesions vary from abdominal pain, distention, obstructive symptoms, nausea, vomiting and jaundice [3-5].
Pancreatic cysts are rare in the paediatric age group and consists of subtypes which are congenital-developmental cysts, retention cysts, duplication cysts, pancreatic pseudocysts, neoplastic cysts, and parasitic cysts. The first three types are named true cysts because these cysts have true epithelial lining [4,6]. Although the etiology of congenital pancreatic cysts remained idiopathic, persistence or failure of embryonic pancreatic ducts to regress or when they became obstructed, fluid-filled cystic lesions form [3,7].
True pancreatic cysts can arise from any part of the pancreas but the majorities are frequently localized in the tail or neck of the pancreas (62%). While cysts in 32% of cases arise from the head of the pancreas [5,8].
Differential diagnosis for congenital pancreatic cysts is duplication cyst of the stomach, pancreatic pseudocysts, choledochal cyst or duplication cyst of the duodenum. Congenital pancreatic cyst aspirated fluid was reported to be with low amylase level. This can be used to differentiate it from retention cysts in which amylase was reported to be considerably high (1000- 3000 IU/L) [7,9]. Duplication cyst may be distinguished from a congenital cyst by its symptomatic presentation, while congenital pancreatic cysts are more likely to be asymptomatic [8,10]. Histologically, both are lined by true epithelium, however duplication cysts are usually singular compared to the complexity of congenital pancreatic cysts [4,9].
Abdominal ultrasound can evaluate the nature of the mass whether solid or cystic. While, it has limitations to evaluate the origin of the cyst and the relations between it and adjacent tissues. Congenital pancreatic cyst usually presents by US as upper abdominal fluid-filled cystic lesions, abdominal magnetic resonance imaging and computed tomography are more valuable and usually show a well-defined homogenous unilocular cyst. MR imaging is however more superior to abdominal CT for evaluating the origin and relations of the cysts which is useful in preoperative planning [10-12].
Endoscopic retrograde cholangiopancreatography (ERCP) can distinguish any communication of the cyst with pancreatic duct or biliary tree, but being an invasive procedure, we didn’t consider it as a diagnostic modality in our case.
Surgical excision of these cysts with enucleation, or resection being the typical approaches [3,10,11]. This however is not always possible and it depends on the size and location of the cyst. Total excision is possible for those cysts located in the body and tail of the pancreas which may necessitate distal pancreatectomy [5,6,11]. Cysts located in the head of the pancreas are difficult to be completely excised and better managed via internal drainage either cystoduodenostomy or Roux-en-Y cystojejunostomy [7,12]. In current patient, total excision with preservation of the pancreas was performed.
Conclusion
Congenital pancreatic cyst is a seldom finding in paediatric age group and should be thought about in the differential diagnosis of cystic lesions of the upper abdomen in infants and children. Preoperative diagnosis is difficult especially in huge cysts and MRI alone or with CT abdomen are considered in these cases. The ideal management is complete surgical excision but this not always possible so internal drainage should be done in such cases.
Declarations
Ethics approval and consent to participate
The study has a retrospective nature and was conducted ethically.
Consent for publication
A written informed consent to publish these information was obtained from the parent of the child.
Authors’ contributions
Mohamed Gaber: conception of the all work, data collection analysis and interpretation, drafting the article.
References
- Eun Mi K, Jaeho S, Ga Won J (2019) Multiple Congenital Pancreatic Cysts in a Neonate. Neonatal Medicine 26(2): 117-120.
- Shi J, Wang C, Lv F (2020) Congenital Pancreatic Pseudocyst. Journal of Pediatric Surgery Case Reports 56: 101422.
- Brungardt JG, Schropp KP (2020) In-utero pancreatic cyst with postnatal resolution. Journal of Pediatric Surgery Case Reports 54: 101396.
- Thien HH, Son NH, Xuan NT, Hieu MT, Cuong PN, et al. (2021) Giant congenital pancreatic cyst in a neonate. Journal of Pediatric Surgery Case Reports 71: 101906.
- Castellani C, Zeder SL, Spuller E, Höllwarth ME (2009) Neonatal congenital pancreatic cyst: diagnosis and management. J Pediatr Surg 44(2): e1-4.
- Bawazir OA, Al-Salem AH, Bawazir AO (2017) Congenital pancreatic cyst: preoperative diagnosis and management. Journal of pediatric surgery case reports 25: 16-21.
- Warnock WT, Khoshnam N, Bird KM, Schaffer LR, Lou LH, et al. (2016) Congenital cyst of the pancreas: a case report and review of literature. Fetal Pediatr Pathol 35(4): 265-271.
- Shahid M, Javed Z, Usman M, Iltaf S (2018) True Congenital Pancreatic Cyst: A Rare Entity. Cureus 10(9): e3318.
- Cadili L, Cullen KL, Finn NJ, Singh A, Webber E, et al. (2022) A rare case of a congenital pancreatic duplication cyst in an infant complicated by an upper GI bleed, pancreatitis, cyst infection and gastric outlet obstruction. J Surg Case Rep 2022(7): rjac326.
- Sarcon AK, Horst KK, Bendel EC, Polites SF (2022) A large congenital pancreatic cyst mimicking a macrocytic lymphatic malformation. Radiol Case Rep 17(7): 2542-2549.
- Farina R, Foti PV, Iannace FA, Conti A, Pennisi I, et al. (2022) True congenital multicystic disease of the pancreas in the infant: a very rare case. J Ultrasound 25(3): 721-723.
- Zani-Ruttenstock E, Zani A (2023) Pancreatic Disorders. In Pediatric Surgery: Diagnosis and Management. Cham: Springer International Publishing, Pp. 1155-1171.






























