Use of an Expiratory Filter to Reduce Nosocomial Spread When Treating a COVID Positive Neonate with bCPAP: A Case Report
Noah Daniel1*, Ghassan Bou Saba1, Navid Roodaki2, Daisy Garcia2, Michelle Dundek1,3, Hena Wadhwa1, Ellie Ng1 and Thomas Burke1,3,4,5
1Vayu Global Health Foundation, Boston, Massachusetts, USA
2locos Training and Regional Medical Center, Department of Pediatrics, San Fernando City, La Union, Philippines
2Massachusetts General Hospital, Global Health Innovation Lab, Department of Emergency Medicine, Boston, Massachusetts, USA
2Harvard Medical School, Boston, Massachusetts, USA
2Harvard T.H. Chan School of Public Health, Boston, Massachusetts, USA
Submission: September 20, 2022; Published: October 13, 2022
*Corresponding author: Noah Daniel, Vayu Global Health Foundation, 22 Welgate Rd, Medford, MA, 02155, USA, Tel: (+1)7038221329
How to cite this article:Noah D, Ghassan Bou S, Navid R, Daisy G, Michelle D, et al. Use of an Expiratory Filter to Reduce Nosocomial Spread When Treating a COVID Positive Neonate with bCPAP: A Case Report. Acad J Ped Neonatol 2022; 12(2): 555887. 10.19080/AJPN.2022.12.555887
Abstract
The SARS-CoV-2 virus has caused COVID-19 infections in neonates. Although neonates are usually less severely affected by COVID-19 than adults, they are still at risk for respiratory compromise and transmission of COVID-19 to parents and health care workers. Continuous positive airway pressure (CPAP) is a promising alternative to invasive ventilation for the treatment of infants in respiratory distress due to COVID-19 and other etiologies. However, controlling respiratory virus transmission remains a challenge for neonatal intensive care units (NICUs), particularly those in resource constrained settings. To mitigate COVID-19 aerosol transmission, WHO recommends the use of expiratory filters on aerosol generating procedures such as when providing non-invasive ventilation with CPAP. Expiratory filters have routinely been used when treating neonates with invasive ventilation, but there is a dearth of evidence on the use of expiratory filters during the treatment of neonates with non-invasive ventilation. We describe the use of a novel bubble CPAP (bCPAP) system engineered with an expiratory filter to treat a COVID-19 positive neonate with respiratory distress at Ilocos Training and Regional Medical Center in the Philippines. This case raises awareness of the potential use of expiratory filters during treatment with bubble CPAP to mitigate respiratory virus transmission in resource constrained NICUs.
Keywords: CPAP, neonate, expiratory filter, nosocomial infection, COVID-19
Introduction
The SARS-CoV-2 virus has caused COVID-19 infections in neonates. Although neonates are usually less severely affected by COVID-19 than adults, they are still at risk for respiratory compromise and transmission of COVID-19 to parents and health care workers [1data describing the effect of SARS-CoV-2 in this group are scarce, and guidance is variable. We aimed to describe the incidence, characteristics, transmission, and outcomes of SARS-CoV-2 infection in neonates who received inpatient hospital care in the UK. METHODS: We carried out a prospective UK population-based cohort study of babies with confirmed SARS-CoV-2 infection in the first 28 days of life who received inpatient care between March 1 and April 30, 2020. Infected babies were identified through active national surveillance via the British Paediatric Surveillance Unit, with linkage to national testing, paediatric intensive care audit, and obstetric surveillance data. Outcomes included incidence (per 10 000 livebirths]. Continuous positive airway pressure (CPAP) is a promising alternative to invasive ventilation for the treatment of infants in respiratory distress due to COVID-19 and other etiologies [2-4].
In the age of the COVID-19 pandemic, treatment procedures are expected to work in tandem with infection control protocols. Aerosolized droplets are considered the primary transmission route of COVID-19 and contribute to high COVID-19 infection rates [5]. Therefore, NICU infection management protocols generally call for medical staff to wear PPE (personal protective equipment), use of expiratory filters during aerosol generating procedures (i.e. ventilation), and geographic isolation of suspected COVID-19 positive newborns in a designated COVID-19 ward [6-8].
Recommended transmission control measures have limited applicability for high volume and resource constrained settings. Practices such as geographic isolation of patients and assignment of medical providers solely dedicated to infected patients are often impractical, if not impossible, in overcrowded and understaffed hospitals [9,10]. Infections are exacerbated by shortages of PPE, which was already scarce in low resource settings before the pandemic [11]. Even if staff have access to advanced face masks, effective protection depends on a COVID-19 positive patient also wearing a face mask [12]. However, infection source control via face masks is not practical in newborns [13]. Successful source control of COVID-19 infected neonates has been achieved in some cases via expiratory filters placed on invasive ventilator circuits (i.e., mechanical ventilators). However, broad applicability in neonates with respiratory distress is limited since invasive ventilation is infrequently used [14].
With all the barriers to quality infection transmission control, it is not surprising that there have been reported cases of COVID-19 transmission from neonates to masked health care workers. In a NICU in Botswana, three masked healthcare workers contracted COVID-19 from interactions with an infant being treated with supplemental oxygen therapy [15]. Horizontal transmission to other infants in NICUs has been reported in the US [16].
Although, WHO urges the use of expiratory filters in adult and pediatric aerosol generating procedures, and there exists ample documentation of clinicians using invasive ventilators equipped with expiratory filters to treat neonates, to the best of our knowledge we present the first case of an infant diagnosed with COVID-19 who was treated with CPAP equipped with an expiratory filter [17-20].
Below, we describe the use of a novel bCPAP system engineered with an expiratory filter to treat a COVID-19 positive neonate with respiratory distress and reduce nosocomial infections at Ilocos Training and Regional Medical Center in the Philippines. The patient’s parents provided written informed consent to publish this case report.
Case Report/Case Presentation
A 28-year-old G1P1 COVID-19 positive mother delivered a 33-weekgestational age infant who was in respiratory distress immediately after birth. Birth weight was 1500 g and APGAR scores were seven and nine at one and five minutes of life. Moderate intercostal retractions and tachypnea developed shortly after delivery. The newborn was treated with one L/min of low-flow unblended oxygen and immediately transferred from a peripheral hospital to the Ilocos Training & Regional Medical Center’s (ITRMC) Neonatal Intensive Care Unit in La Union, Philippines. At ITRMC, an umbilical vein catheter was placed and blood laboratory analysis revealed mild anemia (12.6 g/dL) and thrombocytopenia (57,000). Arterial Blood Gases (ABGs) demonstrated a partially compensated metabolic acidosis with adequate oxygenation. Plain chest radiography identified infiltrates in the right lung field suggestive of pneumonia. The newborn was placed on ampicillin and gentamycin for possible sepsis, however COVID-19 infection was considered likely.
The newborn’s work-of-breathing steadily increased, eventually triggering treatment with a Vayu bCPAP system. Initial bCPAP settings included an FiO2 of 30% and pressure of five cmH2O. An electrostatic filter (Great Group Medical Vf-2160 series) with viral filtration efficiency of 99.99% was positioned immediately prior to the pressure generator in the expiratory limb of the respiratory circuit.
After being placed on a Vayu bCPAP system, the infant’s respiratory distress significantly improved. An RT-COVID-19 PCR test performed at 48 hours of life was positive. Additional laboratory tests at 48 hours included elevated procalcitonin (1.23 ng/mL) and C-reactive protein (3.17 mg/L) levels and a normal ABG. Upon testing positive for COVID the newborn was moved to an isolation area and infection control measures such as strict use of PPE were employed.
On the fourth day of hospitalization, abdominal distention, and coffee ground oro-gastric tube (OGT) output were noted. Tachypnea and retractions continued to improve. Abdominal radiographs demonstrated an ileus. Necrotizing enterocolitis was suspected, the infant was started on total parenteral nutrition (TPN) and antibiotics were shifted to Ceftazidime, Amikacin and Metronidazole.
Abdominal distention and all signs of respiratory distress resolved by day seven of life. The neonate was successfully weaned from the Vayu bCPAP system to room air and oral tube feeding was initiated.
By the tenth day of hospitalization a repeat COVID RT-PCR was negative and ABG’s were normal. The newborn fully recovered. As per hospital protocol during the COVID-19 surge, weekly COVID RT-PCR tests were administered to all healthcare workers and all of healthcare personnel that cared for the newborn tested negative.
The infant was discharged on the fourteenth day of life.
Discussion/Conclusion
In summary, we described the use of a novel bCPAP system engineered with a downstream filter to treat a COVID-19 positive neonate in respiratory distress. The filter was positioned on the expiratory limb of the breathing circuit to limit the nosocomial spread of infection to other patients and healthcare workers (Figure 1).

We speculate that there are several reasons this case is without precedent. First, there have been reports that actively heated and humidified CPAP systems equipped with expiratory filters may cause instability in the system’s delivered pressure and impose an increase in the work of breathing [21]. These effects are far more detrimental for infants than for adults or older children who have more developed respiratory systems [22-25]. Additionally, before the pandemic, infection control was less of a priority and this, in concert with the dearth of research on the effect of expiratory CPAP filters on infants, may have inhibited the use of CPAP system compatible filters when treating neonates [26].
Findings from our lab are consistent with Davis et al’s conclusion that expiratory filters positioned before a pressure generator significantly increase the delivered pressures in actively heated bCPAP systems [21]. However, we found that the delivered pressure in a Vayu bCPAP system did not significantly change when an expiratory filter (Great Group Medical Vf-2160 series) was positioned before the pressure generator. When set to 8 cm H2O of pressure, the mean pressures delivered by a Vayu system after 24 hours with a filter and without were 8.00 ± 0.05 cm H220 and 7.95 ± 0.03 cm H2O respectively (Figure 2). These results are consistent with our lab’s previously reported findings that the Vayu bCPAP system’s delivered pressure remains stable and accurate when used with an expiratory filter [27].
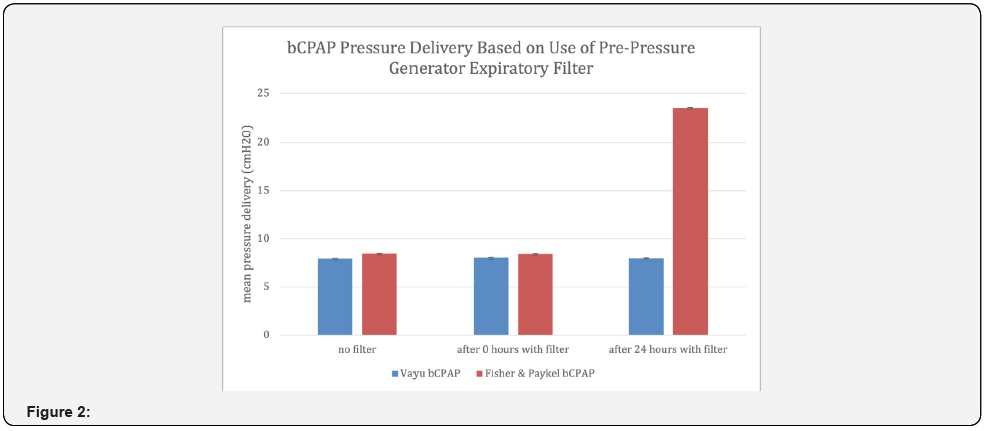
The varying effects of expiratory filters on delivered pressures across different bCPAP systems are likely attributed to the presence or absence of condensate in the exhalation limbs and within the expiratory filters of bCPAP systems. We observed persistent condensate formation in the expiratory limb of a Fisher & Paykal bCPAP device (which had an increase in delivered pressures), but no condensate formation in a Vayu bCPAP system (which had no change in delivered pressure) over a 24-hour test period. Further investigation identified that the condensation was caused by the heater in the Fisher Paykel bCPAP circuit. In contrast, the Vayu bCPAP system is innovative in that it uses the heat from a warmer or incubator to provide an ideal mixed gas temperature. Our findings were similar to Davis et al who reported that the delivered pressure is more stable in a Fisher & Paykel bCPAP device when an expiratory filter is placed after the pressure generator rather than before. When an expiratory filter is placed before the pressure generator it can become saturated with water [21]. Our findings are consistent with Donaldsson et al’s investigation that reported no significant changes in delivered pressures of bCPAP devices in a non-humidified environment [28].
The Vayu bCPAP system has the potential to mitigate virus transmission from infants in NICUs with COVID-19 and other respiratory infections such as respiratory syncytial virus (RSV) [29]. Since newborns are obligate nose breathers and properly fitted bCPAP devices are essentially closed systems, the expiratory filter on a Vayu bCPAP system may help protect healthcare workers and others that come in contact with infected newborns by channeling expiratory gases through the expiratory filter [30]. Despite decades of infection control quality improvement efforts, respiratory transmission rates remain high for hospitalized infants who come in contact with RSV infected patients [29]. Subsequently, nosocomial respiratory viral infections remain a leading cause of morbidity and prolonged hospital stay among preterm newborns [31,32]. The burden of respiratory nosocomial infections is even higher in resource constrained settings where NICU outbreaks are more frequent and mortality rates greater [9].
In bCPAP systems without condensation, expiratory filters appear to have little effect on pressure delivery and are a relatively affordable modification for thwarting nosocomial infections compared to building isolation rooms or hiring specialized staff. Furthermore, as of January 2022 the NICU at Ilocos Regional Training Medical Center routinely uses novel expiratory filters that have reusable filter housings. The filter disks of these novel filters can be replaced every 24 hours at a cost of $0.18 USD. While expiratory filters for neonates are typically single use and designed for mechanical ventilators, this case and the development of reusable filters may help pave the way for exploring use of expiratory filters with neonatal CPAP systems more broadly [2,33- 35].
Neonatal bCPAP device manufacturers should strongly consider engineering and testing modifications that allow incorporation of downstream filters similar to the Vayu bCPAP system in order to better prepare NICUs worldwide for both the current and future pandemics.
Statements
Statement of Ethics
This case reports is in compliance with the guidelines for human studies accordance with the World Medical Association Declaration of Helsinki.
Study approval statement: the Institutional Review Board of Ilocos Training & Regional Medical Center does not require approval for case reports.
Consent to publish statement: Informed consent was obtained from the parents of the patient for publication of the details of their medical case and any accompanying images. Information that could possibly identify the patient in this case report were avoided.
Conflict of Interest Statement
No conflict of interest reported.
Funding Sources
No funding was needed for this case report.
References
- Gale C, Quigley MA, Placzek A, Knight M, Ladhani S, et al. (2021) Characteristics and outcomes of neonatal SARS-CoV-2 infection in the UK: a prospective national cohort study using active surveillance. Lancet Child Adolesc Health 5(2): 113-121.
- Flannery DD, O’Donnell E, Kornhauser M, Dysart K, Greenspan J, et al. (2016) Continuous Positive Airway Pressure versus Mechanical Ventilation on the First Day of Life in Very Low-Birth-Weight Infants. Am J Perinatol 33(10): 939-944.
- Shalish W, Lakshminrusimha S, Manzoni P, Keszler M, Sant’Anna GM. (2020) COVID-19 and Neonatal Respiratory Care: Current Evidence and Practical Approach. Am J Perinatol 37(8): 780-791.
- Sagheb S, Lamsehchi A, Jafary M, Atef-Yekta R, Sadeghi K (2020) Two seriously ill neonates born to mothers with COVID-19 pneumonia- a case report. Ital J Pediatr 46(1): 137.
- Bazant MZ, Bush JWM (2021) A guideline to limit indoor airborne transmission of COVID-19. Proc Natl Acad Sci U S A 118(17): e2018995118.
- De Rose DU, Piersigilli F, Ronchetti MP, Santisi A, Bersani I, et al. (2020) Novel Coronavirus disease (COVID-19) in newborns and infants: what we know so far. Ital J Pediatr 46(1): 56.
- Cavicchiolo ME, Trevisanuto D, Priante E, Moschino L, Mosca F, et al. (2022) Italian neonatologists and SARS-CoV-2: lessons learned to face coming new waves. Pediatr Res 91(3): 513-521.
- CDC (2020) Evaluation and Management Considerations for Neonates At Risk for COVID-19 [Internet].
- Haas JP, Trezza LA (2002) Outbreak investigation in a neonatal intensive care unit. Semin Perinatol 26(5): 367-378.
- Baley J, COMMITTEE ON FETUS AND NEWBORN (2015) Skin-to-Skin Care for Term and Preterm Infants in the Neonatal ICU. Pediatrics 136(3): 596-569.
- Mc Mahon DE, Peters GA, Ivers LC, Freeman EE (2020) Global resource shortages during COVID-19: Bad news for low-income countries. PLoS Negl Trop Dis 14(7): e0008412.
- Ueki H, Furusawa Y, Iwatsuki-Horimoto K, Imai M, Kabata H, et al. (2020) Effectiveness of Face Masks in Preventing Airborne Transmission of SARS-CoV-2. mSphere 5(5): e00637-20.
- Esposito S, Principi N. (2020) To mask or not to mask children to overcome COVID-19. Eur J Pediatr. 179(8): 1267-1270.
- Behnke J, Lemyre B, Czernik C, Zimmer KP, Ehrhardt H, et al. (2019) Non-Invasive Ventilation in Neonatology. Dtsch Arzteblatt Int 116(11): 177-183.
- Nakstad B, Kaang T, Gezmu AM, Strysko J (2021) Nosocomial SARS-CoV-2 transmission in a neonatal unit in Botswana: chronic overcrowding meets a novel pathogen. BMJ Case Rep 14(6): e242421.
- Bhargava S, Lumba R, Mally P, Bailey S, Verma S (2021) Horizontal Transmission of COVID-19 in a 24-Week Premature Infant and Post-discharge Follow-Up. Cureus 13(10): e18455.
- World Health Organization (2020) Technical specifications for invasive and non-invasive ventilators for COVID-19: Interim guidance. Who, Geneva.
- Moreno-Duarte I, Evans AS, Alder AC, Vernon MC, Szmuk P, et al. (2021) An unexpected COVID-19 diagnosis during emergency surgery in a neonate. Paediatr Anaesth 31(5): 613-615.
- Terheggen U, Heiring C, Kjellberg M, Hegardt F, Kneyber M, et al. (2021) European consensus recommendations for neonatal and paediatric retrievals of positive or suspected COVID-19 patients. Pediatr Res 89(5): 1094-1100.
- Trevisanuto D, Weiner G, Lakshminrusimha S, Azzimonti G, Nsubuga JB, et al. (2020) Management of mothers and neonates in low resources setting during covid-19 pandemia. J Matern Fetal Neonatal Med 35(12): 2395-2406.
- Davis JW, Pillow JJ, Cooper MN, Dahl MJ (2020) Electrostatic Filters to Reduce COVID-19 Spread in Bubble CPAP: An in vitro Study of Safety and Efficacy. Neonatology 117(6): 736-741.
- Alkan OS, Soysal B, Calkavur S, Gökmen Yıldırım T, Kemet E, et al. (2020) Is respiratory syncytial virus infection more dangerous than COVID 19 in the neonatal period? J Matern Fetal Neonatal Med 35(22): 4398-4403.
- Landry SA, Mann DL, Djumas L, Messineo L, Terrill PI, et al. (2020) Laboratory performance of oronasal CPAP and adapted snorkel masks to entrain oxygen and CPAP. Respirology 25(12): 1309-1312.
- Winck JC, Ambrosino N (2020) COVID-19 pandemic and non invasive respiratory management: Every Goliath needs a David. An evidence based evaluation of problems. Pulmonology 26(4): 213-220.
- Sundaram M, Ravikumar N, Bansal A, Nallasamy K, Basavaraja GV, et al. (2020) Novel Coronavirus 2019 (2019-nCoV) Infection: Part II - Respiratory Support in the Pediatric Intensive Care Unit in Resource-limited Settings. Indian Pediatr 57(4): 335-342.
- Temsah MH, Al Huzaimi A, Alrabiaah A, Alamro N, Al-Sohime F, et al. (2021) Changes in healthcare workers’ knowledge, attitudes, practices, and stress during the COVID-19 pandemic. Medicine (Baltimore) 100(18): e25825-e25825.
- L Dundek M, Ng EK, M Brazil A, DiBlasi RM, Poli JA, et al. (2021) Evaluation of a Bubble CPAP System for Low Resource Settings. Respir Care 66(10): 1572-1581.
- Donaldsson S, Naver L, Jonsson B, Drevhammar T (2020) COVID-19: minimising contaminated aerosol spreading during CPAP treatment. Arch Dis Child Fetal Neonatal Ed 105(6): 669-671.
- Kulkarni H, Smith CM, Lee DDH, Hirst RA, Easton AJ, et al. (2016) Evidence of Respiratory Syncytial Virus Spread by Aerosol. Time to Revisit Infection Control Strategies? Am J Respir Crit Care Med 194(3): 308-316.
- Trabalon M, Schaal B (2012) It Takes a Mouth to Eat and a Nose to Breathe: Abnormal Oral Respiration Affects Neonates’ Oral Competence and Systemic Adaptation. Lau C, editor. Int J Pediatr 2012: 207605.
- Comas-García A, Aguilera-Martínez JI, Escalante-Padrón FJ, Lima-Rogel V, Gutierrez-Mendoza LM, et al. (2020) Clinical impact and direct costs of nosocomial respiratory syncytial virus infections in the neonatal intensive care unit. Am J Infect Control 48(9): 982-986.
- Gill CJ, Mwananyanda L, MacLeod WB, Kwenda G, Pieciak R, et al. (2022) Infant deaths from respiratory syncytial virus in Lusaka, Zambia from the ZPRIME study: a 3-year, systematic, post-mortem surveillance project. Lancet Glob Health 10(2): e269-277.
- Thukral A, Sankar MJ, Chandrasekaran A, Agarwal R, Paul VK (2016) Efficacy and safety of CPAP in low- and middle-income countries. J Perinatol Off J Calif Perinat Assoc 36(Suppl 1): S21-S28.
- Mahase E (2021) Covid-19: CPAP reduces need for invasive mechanical ventilation in patients requiring oxygen, study finds. BMJ 374: n1950.
- Chakkarapani AA, Adappa R, Mohammad Ali SK, Gupta S, Soni NB, et al. (2020) “Current concepts of mechanical ventilation in neonates” - Part 1: Basics. Int J Pediatr Adolesc Med 7(1): 13-18.






























