Pediatric Amplified Musculoskeletal Pain Syndrome Complicated by a Fever of Unknown Origin
Justin Hovey1*, MD, Jennifer H. Ra1, BA and Nola Ernest2, MD, PhD
1Alabama College of Osteopathic Medicine, Dothan, Alabama, USA
2Dothan Pediatric Clinic, Dothan, AL, USA
Submission: September 20, 2022; Published: October 13, 2022
*Corresponding author: Justin Hovey, M.D, Alabama College of Osteopathic Medicine, Dothan, Alabama, 445 Health Sciences Blvd. Dothan, AL 36303, USA
How to cite this article:Justin Hovey, Jennifer H. Ra, BA, Nola Ernest, M. Pediatric Amplified Musculoskeletal Pain Syndrome Complicated by a Fever of Unknown Origin. Acad J Ped Neonatol 2022; 12(2): 555886. 10.19080/AJPN.2022.12.555886
Abstract
Amplified musculoskeletal pain syndrome (AMPS) is a rare diagnosis that is part of a broad spectrum of chronic pediatric musculoskeletal pain. Typically, females are more affected than males with an average age of onset of 9-15 years. The lower extremity is most often the primary site of injury and subsequent chronic pain. Labs and imaging studies are usually unrevealing. The various clinical presentations and psychosocial complexities of each patient commonly leads to delayed diagnosis. In this article, we present a nine-year-old female with no significant medical history who sustained a Salter-Harris type I fracture to her left ankle. After removal of her cast, she subsequently developed swelling and pain along with a fever of unknown origin. The fever persisted for 115 days and led to a comprehensive work-up. Following consultation with pediatric rheumatology, a diagnosis of AMPS was made. After the diagnosis was made, the patient underwent intense physical therapy, and her symptoms resolved. This case highlights the complications that arise with diagnosing AMPS when affected by an autonomic component leading to fevers. The prolonged nature of diagnosing AMPS stems from the complicated spectrum of clinical presentations and pathophysiological etiologies. The unique autonomic component of AMPS in this patient complicated and delayed the diagnosis. Future studies should focus on exploring the possible manifestations of AMPS when affected by seemingly unassociated symptoms, like fevers.
Increased knowledge and understanding of various clinical manifestations of AMPS can help physicians more quickly diagnose and treat the disease.
Article Summary: AMPS can present with a broad spectrum of clinical manifestations. This case highlights a unique presentation of AMPS complicated by FUO that lasted 115 days
Abbreviations: AMPS: Amplified Musculoskeletal Pain Syndrome; FUO: Fever of Unknown Origin
Introduction
Amplified musculoskeletal pain syndrome (AMPS) is a relatively rare diagnosis in children that encompasses a spectrum of pain syndromes. Children who are diagnosed with this condition describe musculoskeletal pain that is intense, can be localized or diffuse, and associated with functional disability despite the lack of extensive tissue damage [1]. Females are affected more often than males in a 3 to 1 ratio, and the typical age of onset is 9-15 years [2]. Affected children are typically of higher socioeconomic status, more mature than their counterparts, are accomplished in school and extracurricular activities, and are usually described as perfectionists. Major life stressors are frequently discovered with the presentation [3].
During childhood, the lower limb is most often the primary site of AMPS related disability [2]. Although most patients report continuous pain in an affected limb and can often recall exactly when it began, some children may have a more nebulous onset, and it may be difficult to localize the pain [3]. Approximately 14% of children affected by AMPS will have autonomic signs associated with more localized pain. When autonomic signs are present, the pain is more likely to be limited [1]. On the other hand, children without autonomic involvement are more likely to have pain involving multiple sites or joints [1,3].
Frequently, families make multiple visits to emergency departments and outpatient clinics before a diagnosis is made, leading to numerous and often duplicate tests being performed on symptomatic patients resulting in substantial costs to both the health care system and families [4]. Labs and imaging studies performed on patients with AMPS are typically unrevealing [3]. These factors, along with the various clinical presentations and psychosocial complexities of each patient, often lead to a delayed diagnosis [3]. Though AMPS is rare, the overall cost burden of this syndrome is nearly equivocal to the high cost of ADHD [4].
Given the peculiar spectrum of AMPS, the understanding of the pathophysiology is ever evolving. Currently, a number of pathophysiological processes are theorized to be responsible for the development of the condition. Genetic predisposition, central sensitization, blood flow, abnormal cytokine production, and psychosocial factors all likely play a role in the development of AMPS. Central sensitization with dorsal horn activity is the primary abnormality driving the exaggerated pain responses seen in the disease process. Glutamate and Substance P are the two neurotransmitters that are in involved in this central sensitization and the amplified pain. Cytokine dysregulation produced peripherally may play a role in sensitization of the central nervous system as well. Furthermore, sympathetically maintained pain may cause regional ischemia that results in significant localized or widespread pain. Alterations in developing brains due to environmental influences probably play a role as well. Trauma and toxic stress can impact the developing brains of children and adolescents; particularly the networks concerned with reward, motivation/learning, and descending modulatory control for pain [5].
Despite the intense pain symptoms and loss of function associated with the syndrome, patients diagnosed with AMPS generally have good outcomes with exercise therapy alone. Psychotherapy may be added to physical therapy but is rarely needed. Re-establishing normal use of the affected limbs and returning to normal daily function with multidisciplinary therapy (physical therapy, occupational therapy, and cognitive behavioral therapy when needed) are the mainstays of AMPS treatment [2,5,6]. Typically, greater than 80-90% of children who are diagnosed regain full function and are without pain in one month. Around 5% of children will not improve and have to be referred for significant psychotherapy. Although the long-term prognosis is generally favorable, 15-30% of all children diagnosed will have a significant relapse within the first six months, most of which resolve with self-initiated exercise programs [2,3].
Here, we report on a 9-year-old female with fever of unknown origin and significant ankle pain following a left ankle fracture that lasted over a three-month period. The patient was diagnosed with Amplified Musculoskeletal Pain Syndrome with an autonomic component leading to her fevers. Fortunately, the patient responded well to intensive physical therapy and is now fever and pain free.
Case Presentation
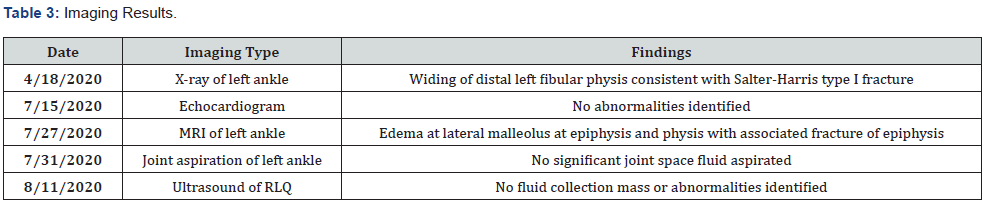
A 9-year-old female gymnast presented to the Emergency Department (ED) with a left ankle injury after getting her foot trapped on a caged pedal resulting in forced hyper-dorsiflexion of her foot while on a stationary bike. Upon arrival to the ED, x-rays of the left ankle were taken. Findings revealed widening of the distal left fibular physis consistent with a Salter-Harris type I injury with lateral soft tissue swelling. No major acute fractures or dislocations were noted at the time. Orthopedics assessed and casted the injured ankle with no complications. Patient and family were sent home with directions to follow-up with orthopedics. The cast was removed one month later.
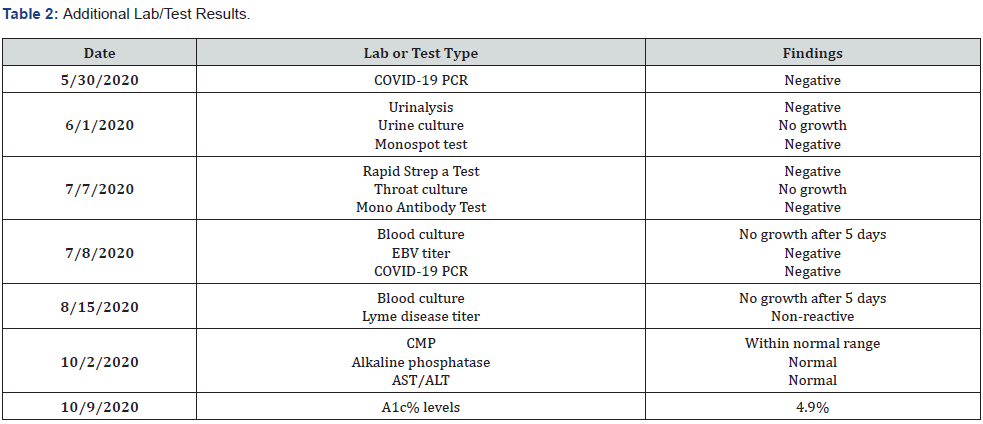
Following removal, the patient began to experience arthralgia and edema to the left ankle. She also developed a fever at the moment of cast removal (100.4 F). Her symptoms persisted for two weeks. A CBC, CRP, ESR, UA, and monospot were ordered and all labs were unrevealing (Tables 1 and 2). The fevers continued to persist a week following the initial presentation to her pediatrician. On the second visit, a murmur was found on exam, thus an echocardiogram was ordered. ECHO findings were negative for endocarditis and other cardiac abnormalities. The patient started naproxen following the negative work-up, which only provided transient relief for fever and pain.
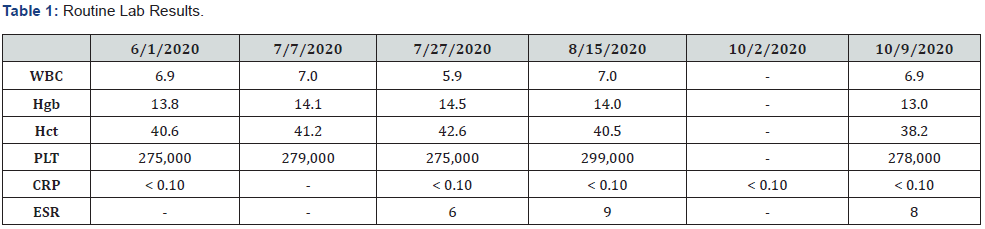
WBC: white blood cells; Hgb: hemoglobin; Hct: hematocrit; PLT: platelets; CRP: C-reactive protein; ESR: erythrocyte sedimentation rate
After visiting her pediatrician, the patient was no longer able to bear weight on left ankle and her fever persisted. She was seen in consultation by orthopedics, where she received a magnetic resonance imaging (MRI) without IV contrast of her left ankle. MRI findings revealed edema at the lateral malleolus at the epiphysis and physis with an associated fracture of the epiphysis, which were consistent with a Salter-Harris type I fracture and a tear to the anterior talofibular ligament. With written parental consent, the patient also received fluoroscopic-guided joint aspiration, which revealed no fluid, major infections, or abnormalities. Repeat CBC, CRP, ESR showed no abnormalities. She was re-casted about one week later following consultation with a pediatric orthopedic physician.
During the four-week casting period, the patient did not experience any ankle pain nor fever. Shortly after the 2nd cast was removed, she again was unable to bear weight and began experiencing the same symptoms of arthralgia and fever (100.9 F). Around the time of cast removal, she began to complain of right lower quadrant pain. The patient again returned to her primary pediatrician, and an abdominal ultrasound was ordered. The ultrasound findings revealed no fluid collection, mass, appendix abnormalities, or other abnormalities. Repeat labs were unrevealing. At this point, the patient’s family sought consultation with pediatric infectious disease and hematology/oncology. Repeated labs and imaging ordered by those consultants found no abnormalities (Tables 1 and 3).
A few weeks after consulting infectious disease and hematology/oncology, the patient was referred to pediatric rheumatology. She started intensive physical therapy (PT) for her left ankle, which included therapeutic exercises & activities, gait training, neuromuscular rehabilitation, manual therapy, patient education, and self-care. Over 17 PT sessions, the patient’s symptoms began to improve. At the end of PT, the patient had successfully met goals of walking on ground level, squatting, tumbling, and bar work. She is pain and fever free as well.
Discussion
Amplified musculoskeletal pain syndrome (AMPS) is a relatively rare diagnosis in children that encompasses a spectrum of pain syndromes. Typically, females are more affected than males with an average age of onset of 9-15 years. In most cases, the lower extremity is the primary site of injury and subsequent chronic pain [2].
About 14% of children with AMPS will have autonomic signs associated with more localized pain, while those without autonomic signs tend to have pain at multiple sites or joints [1,3]. The prolonged nature of diagnosing AMPS stems from this complicated spectrum of clinical presentations and pathophysiological etiologies. The inability to diagnose AMPS more efficiently often results in families making multiple visits to the ED or outpatient clinics, which leads to numerous and often duplicate tests being performed on symptomatic patients and substantial costs to both the healthcare system and families [4]. In addition, the deterioration of quality of life in patients cannot be disregarded.
In this case, a 9-year-old female presented significant ankle pain and swelling with fever of unknown origin of 115 days. The unique autonomic component of AMPS in this patient complicated and prolonged her diagnosis. Like most patients affected by AMPS, she was subjected to numerous repeat blood tests, imaging studies, and multi-specialty consults. For 115 days, patient was in pain and unable to enjoy her favorite activities like gymnastics. Eventually, intense physical therapy improved her symptoms to the point where she was fever and pain free.
As past studies and this case reveal that intense physical therapy is a highly effective treatment for AMPS, the issue remains identifying AMPS in a timely fashion. The ability to diagnose AMPS efficiently can potentially prevent prolonged disease in patients and allow them to return to normal daily life more quickly. Therefore, future studies should focus on further exploring the possible manifestations of AMPS, especially when affected by seemingly unassociated symptoms, like fevers, so that AMPS can be better diagnosed and treated.
Conclusion
Here, we report a patient with AMPS complicated by fevers. AMPS is a rare and difficult condition to diagnose because of the broad spectrum of clinical presentations and pathophysiology. Increased knowledge and understanding of various clinical manifestations of AMPS can help physicians more quickly diagnose and treat the disease.
Conflict of Interest Disclosures (Includes Financial Disclosures)
Dr. Hovey consults with GSK for COPD education. Ms Ra and Dr. Ernest do not have any conflict-of-interest disclosures.
Contributors’ Statement Page
Dr. Hovey treated the patient and collected data for the manuscript. He also drafted, reviewed, and revised the manuscript.
Ms. Ra and Dr. Ernest treated the patient, collected data, drafted, reviewed, and revised the manuscript.
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
References
- Sherry DD, Sonagra M, Gmuca S (2020) The spectrum of pediatric amplified musculoskeletal pain syndrome. Pediatr Rheumatol Online J 18(1): 77.
- Sherry DD, Wallace CA, Kelley C, Kidder M, Sapp L (1999) Short- and long-term outcomes of children with complex regional pain syndrome type I treated with exercise therapy. Clin J Pain 15: 218-223.
- Sherry DD (2000) An overview of amplified musculoskeletal pain syndromes. J Rheumatol Suppl 58: 44-48.
- Tian F, Guittar P, Moore-Clingenpeel M, Higgins G, Ardoin SP, et al. (2018) Healthcare Use Patterns and Economic Burden of Chronic Musculoskeletal Pain in Children before Diagnosis. J Pediatr 197: 172-176.
- Hoffart CM, Wallace DP (2014) Amplified pain syndromes in children: treatment and new insights into disease pathogenesis. Curr Opin Rheumatol 26(5): 592-603.
- Gmuca S, Weiss PF, McGill M, Xiao R, Ward M, et al. (2022) The Feasibility and Acceptability of Resilience Coaching for Adolescent Chronic Musculoskeletal Pain: A Single-Arm Pilot Trial. Children 9: 1432.






























