Correlation of Foot Length Measurements with Other Anthropometric Parameters in Newborn Babies
Nzeduba C.D1, Asinobi I.N2 and Eneh C.I3
1Lecturer and Senior Registrar, Department of Paediatrics, Enugu State University of Science and Technology and Enugu State University, Nigeria
2Senior Lecturer and Consultant Paediatrician, Department of Paediatrics, Enugu State University of Science and Technology and Enugu State University, Nigeria
3Senior Lecturer and Consultant Paediatrician, Department of Paediatrics, Enugu State University of Science and Technology and Enugu State University, Nigeria
Submission: September 12, 2022; Published: October 10, 2022
*Corresponding author: Eneh C.I, Senior Lecturer and Consultant Paediatrician, Department of Paediatrics, Enugu State University of Science and Technology and Enugu State University Teaching Hospital (ESUT-TH) Parklane, P.M.B. 1030, Enugu State, Nigeria
How to cite this article: Nzeduba C.D, Asinobi I.N, Eneh C.I. Correlation of Foot Length Measurements with Other Anthropometric Parameters in 002 Newborn Babies. Acad J Ped Neonatol 2022; 12(1): 555884. 10.19080/AJPN.2022.12.555884
Abstract
Background: Anthropometric parameters are widely used in paediatrics, they are especially useful in the assessment of newborn babies where they can be used to determine gestational age as well as identify babies who are inappropriate for gestational age.
Methods: A cross-sectional, descriptive study conducted over a six-month period (February to July, 2020) in Enugu State University Teaching Hospital, Enugu. Gestational age was determined using the New Ballard Scoring System (NBS). Foot-length (FL) measurements were made from the heel to the tip of the big toe using a hard transparent plastic ruler. Chest circumference (CC) was measured at the level of the nipple, at the end of expiration, to the nearest 0.1 cm using a non-elastic, flexible measuring tape. Occipito-frontal circumference (OFC) was measured as the maximum circumference of the head to the nearest 0.1cm with a non-elastic, flexible, measuring tape passing above the supra-orbital ridges and over the maximum occipital prominence. All the newborns were weighed naked on a Waymaster infant spring weighing scale to the nearest 50 grams. Gestational age assessment was done using the New Ballard Scoring system. Data were documented on a pretested proforma designed by the researcher, for this study.
Results: Of the 235 infants enrolled, 201(86%) were term and 34(14%) were preterm. Majority of the subjects (51%) were males while the rest (49%) were females. The median foot-length in the study population was 8.00cm (0.50) and the range was 5.10–9.00cm. The occipito-frontal circumference ranged from 25.50–37.20cm and the median was 35cm (2.00). The median birthweight was 3300g (800.00) and the range was 1000.00- 4000.00g. The median chest circumference was 33cm (2.00) and the range was 23.00-35.60cm. There was a strong significant positive correlation between newborn foot-length and GA, BW, CC and OFC with correlation coefficients (r) of 0.845, 0.826, 0.783 and 0.801 respectively (p<0.001).
Conclusion: The findings in this study show that foot length is a good proxy for birth weight. Therefore, foot-length measurements can be used in settings where weighing scale and the expertise required for the measurement of other anthropometric parameters are not available to identify high-risk infants who require urgent life-saving interventions.
Recommendations: Foot-length measurements may be included in the routine anthropometric assessment of newborn babies. The use of foot-length measurement may be promoted for use when weighing scale and the expertise required for the measurement of other anthropometric parameters are not available especially among traditional birth attendants.
Keywords: Foot length, Birth weight, Chest circumference, Occipito-frontal circumference
Introduction
Neonatal mortality remains a major contributor to under-five mortality(U-5MR) worldwide especially in many countries in South Asia and Sub-Saharan Africa [1]. Globally, attention has been focused on childhood survival more than neonatal survival. WHO’s Levels and Trends in child mortality published in 2017 reveals that between 2000 and 2016, the overall U-5MR reduced from 9.9 million deaths to 5.6 million respectively, whereas the proportion of under- five deaths in the newborn period increased from 41 to 46% in the same period. Out of the five countries contributing to half of all global newborn deaths, Nigeria ranks third (9%), preceeded by countries such as India (24%) and Pakistan (10%). Nigeria is thus a major contributor to global newborn mortality [1]. The major contributors to neonatal mortality worldwide are severe infections (36%), pre-term birth (28%) and perinatalasphyxia (23%). Others include low birth weight (LBW) and birth trauma. LBW is an underlying factor in about 70% of neonatal deaths in developing countries [2]. LBW is associated with prematurity (birth weight is directly related to gestational age), increased risk of infections, respiratory difficulties, hypothermia and feeding problems.
Birth weight (BW) is a major determinant of fetal growth and duration of gestation and serves as an empirical indicator of maturity and neonatal survival [3]. However, weight measurements are affected by changes in water, carbohydrate, fat, protein and mineral levels [4]. It is important to consider some of the inaccuracies in weighing scales plus observer error such as parallax. Similarly, weighing scales are not available in many rural settings and not portable when attending deliveries at home, church or TBAs [5]. Other anthropometric measurements such as head circumference (HC), chest circumference (CC) and crown heel length (CHL) have also been used as surrogates to BW. These surrogates are affected by factors such as malnutrition leading to underestimation of growth [6,7]. These anthropometric parameters are also affected by changes in body water, carbohydrate, fat, protein and mineral levels [8].
With all these limitations, the identification and evaluation of low cost and simple assessment methods to determine gestational maturity has been ranked the number one research priority to reduce global mortality from prematurity and low birth weight [2].
Foot-length measurement has been studied as a tool for determination of gestational maturity [2,9]. In 2012, the WHO stated that simplified approaches such as foot length to identify preterm babies, were required for early identification and management of such babies [9]. Foot-length is measured from the heel to the tip of the big toe using a hard transparent ruler. The landmarks are easy to identify and do not require special skills. Furthermore, the foot is easily accessible, and its measurement is quick and efficient even in very ill neonates, such as those nursed in the incubator, without exposing them to the risk of hypothermia. In addition, it is not influenced by subcutaneous fat or sex. However, variations across nations and ethnic groups do occur [10].10
This study intends to determine the relationship between foot-length and other anthropometric parameters especially birth weight. This will aid in the detection of neonates who may either benefit from early and simple life-saving interventions, or require referral for more specialized care.
. Aim
The aim of this study was to establish a correlation between foot-length and other anthropometric parameters.
Method
The subjects were newborn babies: term and preterm whose weights were appropriate for GA delivered in ESUTH or admitted into the Special Care Baby Unit (SCBU) of ESUTH and who met the criteria for recruitment. Preterm and term babies who were delivered in ESUTH or were referred to ESUTH from other hospitals and babies who were within 96 hours of age were included in the study. Babies with congenital anomalies of the foot, neuromuscular disorders, congenital anomalies of the chest or skeletal abnormalities and babies with disorders that distorted respiratory rhythm and congenital skeletal abnormalities were excluded. The Lubchenco growth chart was then used to determine appropriateness for GA and babies who were SGA or LGA were similarly excluded. Babies with suspected chromosomal abnormalities and cardiovascular system disorders and babies with suspected intra uterine infections (Toxoplasmosis, Rubella, Cytomegalovirus and Syphilis) were also excluded from the study.
Ethical approval was obtained from Enugu State University Health Research Ethics Committee, Enugu. Written informed consent was obtained from parent after due explanation of the study using the parent’s desired language. Every step in the study was explained to the parents and they were assured that no adverse effects were expected. Only babies whose parents gave consent were recruited into the study.
Gestational age was noted from the obstetric admission notes as calculated by LMP (GALMP) and/or early antenatal ultrasound (GAUSS). Based on the gestational age, the babies were grouped as preterm and term. The reference standard for gestational age was the New Ballard Score (NBS). The NBS was done by the principal researcher within 96 hours of birth.
Foot length measurements were from the heel to the tip of the big toe using a hard transparent plastic ruler. The foot was placed in a lateral position while the ankle was held and a finger placed at the foot dorsum to avoid eliciting the grasp reflex which would shorten the measurement [9]. Care was taken to ensure that no pressure was exerted on the soft tissue. Both feet were measured. Measurements were performed by the researcher only to ensure a consistent measurement technique. Intra observer error was minimized by taking three measurements and then documenting the mean. Occipito-frontal circumference was measured as the maximum circumference of the head between the glabellas anteriorly and along the occipital prominence posteriorly using a non-extendable measuring tape (Appendix VII). The measurement was done to the nearest 0.1cm using a non-elastic measuring tape. The average of three measurements was taken to minimize intra observer error.
Chest circumference (CC) was measured at the level of the nipple, at the end of expiration, to the nearest 0.1 cm using a non-elastic, flexible, measuring tape according to standard techniques described by Forfar in 1984 (Appendix VIII). The average of three CC measurements was taken to minimize intra-observer error
All the newborns were weighed naked on a Waymaster® infant spring weighing scale (Precision Engineering Co. {Reading} Ltd., England) to the nearest 50 grams (Appendix IX). This scale was always set to zero point before each use and standardized at weekly intervals using a known 5kg weight.
Lubchenco intra-uterine growth chart (Appendix IV) was used to determine growth appropriateness for gestational age. All information obtained was recorded in the proforma (Appendix III) designed for the study
Data collated was coded, entered and analyzed using International Business Machine Statistical Package for Social Sciences (IBM-SPSS version 22 Chicago). Descriptive statistics such as frequency and percentages were used to summarize categorical variables (such as sex), while median and interquartile range were used to describe foot length because of non-normality of the data. Comparison of the foot length between term and preterm babies was done using Mann-Whitney U-test due to non-normality of data. The association between foot length, birth weight and gestational age (categorized into extreme preterm, very preterm, moderate-late preterm and term) was analysed using Kruskal-Wallis test. Post-Hoc pairwise comparison was used to identify the areas of significant relationship between the categories of BW. All tests of significance were two-tailed at 95% confidence interval. A p-value score of < 0.05 is considered significant. Results were presented as prose, tables and figures as appropriate.
Results
This study was conducted over a six (6) month period, from February to July 2020, with two hundred and thirty- five (235) participants enrolled. Three hundred and twenty- five (325) mothers were approached during the study period, thirty- two (32) refused consent while two hundred and ninety- three (293) gave consent. Twenty-seven (27) of the babies were either SGA or LGA, 28 were more than 96 hours at the time of measurements and three had congenital malformations. Eventually, 235 newborn babies who met all the inclusion criteria were recruited for the study. One hundred and ninety three babies (82.1%) were recruited from the maternity ward, while forty two (17.9%) were recruited from the Special Care Baby Unit both of ESUTH.
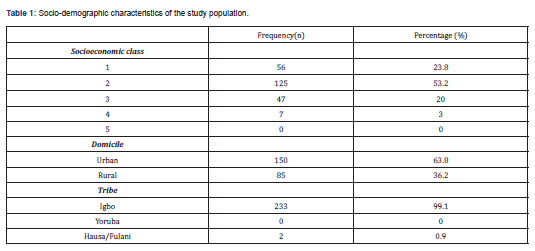
Socio-demographic characteristics of the study population.
The dominant socio-economic class was class two (53.2%), with 3% and 0% in class four five respectively. Mothers of 150 (63.8%) babies reside in urban areas while mothers of 85 (36.2%) babies reside in rural areas. Majority (99.1%) of the study participants were of the Igbo tribe, while 0.9% were of the Hausa/Fulani tribe (Table 1).
Gestational age andsex distribution of the study population.
The gestational ages ranged from 26–42 weeks (Table 2) with a mean (SD) of 37.0(3.4) weeks. Thirty- four (14.5%) were preterm while 201 were term. Amongst the 34 preterms, twenty-two (64.7%) were moderate to late. There were 121 males (51%) and 114 females (49%) giving a male to female ratio of 1.1:1 (Table 2).

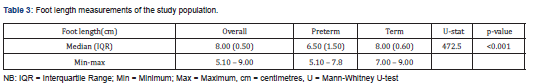
Foot length measurements of the study population
The foot length of the study population ranged from 5.10cm to 9.00cm with a median (IQR) foot length of 8.00cm (0.50). The median (IQR) foot length in the preterm and term subjects were 6.50cm (1.50) and 8.00cm (0.60) respectively (Table 3).
Birth weight, occipito-frontal circumference and chest circumference of the study population.
The birth weight of the subjects ranged from 1000g to 4000g with a median (IQR) birth weight of 3300g (800.00). The median (IQR) birth weight was 1500g (1000) amongst preterms and 3500g (700) among term babies. This was statistically significant (p<0.001)
The occipito – frontal circumference of the study population ranged from 25.50 – 37.20cm with a median (IQR) of 35cm (2.00cm). While preterm babies had a median (IQR) OFC of 30.00(6.13), term babies had a median (IQR) of 35cm (2.00). This was also significant (p<0.001)
The chest circumference ranged from 23.00–37.00 and the median (IQR) was 33cm (2.00). The median (IQR) chest circumference of 26.00cm (6.13) and 33.5cm (2.95) in the preterm and term subjects respectively also showed statistical significance (p<0.001).
There was a significant increase in the anthropometric variables (e.g. birth weight, OFC and CC) as gestational age increased. This was such that, term babies had significantly higher scores in all the anthropometric variables compared with preterm babies (p < 0.001) (Table 4).

Relationship between foot length and birth weight, occipito-frontal circumference and chest circumference.
The relationship between foot length and birth weight, occipito-frontal circumference and chest circumference are presented below
a. Relationship between foot length and birth weight
Figure 1 demonstrates a positive significant correlation between foot length and birth weight (rhos= 0826, p < 0.001). There is a linear relationship between the two variables (figure 1) with a coefficient of determination (R2 = 0.682).
b. Association between birth weight categories and foot length
The median foot length for very low birth weight, low birth weight, and normal neonates were 6.00cm, 6.75cm and 8.00cm, respectively. There is statistically significant difference in foot length among birth weight categories (p < 0.001). Post hoc pairwise comparison shows that the difference was between very low birth weight and low birth weight (p < 0.001), very low birth weight and normal birth weight (p < 0.001), and low birth weight and normal birth weight (p < 0.001) (Table 5).

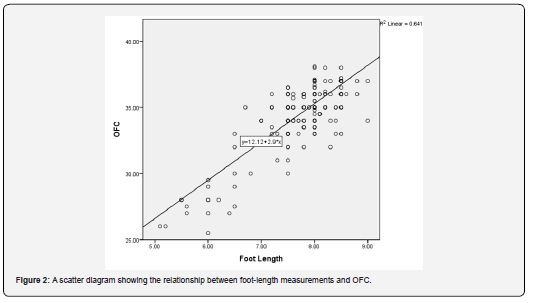
c. Relationship between foot length and occipito-frontal circumference
There is apositive significant correlation between foot length and occipito-frontal circumference (rhos= 0.801, p < 0.001). The scatter plot shows a linear relationship between the two variables (Figure 2) with a coefficient of determination (R2 = 0.641) (Figure 2).
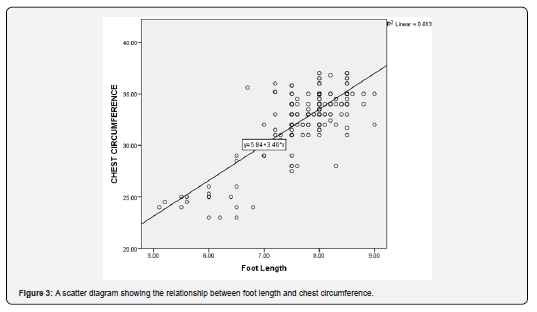
d. Relationship between foot length and Chest circumference
Figure 3 shows a positive significant correlation between foot length and chest circumference (rhos= 0.783, p < 0.001). The scatter plot shows a linear relationship between the two variables (Figure 3) with a coefficient of determination (R2 = 0.613).

Discussion
The findings in this study are comparable with those reported in previous studies [11,12]. For example, Ashish et al. [12] and Mullany et al. [13] reported mean foot length of 7.72cm and 7.92cm, respectively. The similarities in the values of foot length found in the index study with those of previous studies may be explained by some methodological factors. The methodological similarities in these studies include the use of transparent plastic tapes, common landmarks for measurement and the inclusion of preponderance of term neonates. However, despite the robust evidence in the literature suggesting similar values of foot length across studies in various continents [12,13], Wyk et al. [14] found a much lower value (4.83±3.05 cm) in a South African study. It is noteworthy that that study with contrary finding has several methodological differences with the present study. Firstly, whereas the present study used a transparent plastic measuring tape, a caliper was used in the South African study. Secondly, the landmark for the measurement of foot length varied in both studies. While the index study used as landmark, the heel to the tip of the big toes, Wyk et al. [14] used the heel to the longest toe which may not necessarily be the big toe. Thirdly, the least gestational age in the present study was 26 weeks, but the South African study included lower gestational age of 24 weeks. Furthermore, the variations in the values of foot length across studies in various continents may be due to genetic and epigenetic factors [11,13].,
This present study demonstrated a significant strong positive correlation between foot length and the other anthropometric indices. This study further demonstrated a linear positive relationship between foot length and BW, CC and OFC with high coefficients of determination for all the indices.
Occipito-frontal circumference showed the least correlation with foot length. This finding is similar to that found in Bengaluru, India by Anshuman et al. [15] which showed a significant correlation between FL and other anthropometric variables namely BW, OFC and CC with r value of 0.9, 0.86 and 0.81 respectively and a significant P value of <0.0001.This finding is also in agreement to a study in India by Gowri and Kumar [16] who found a very high correlation between foot length and birth weight(r=0.94). Hadush et al [17] also found a strong positive correlation between foot length and birth weight(r=0.71), although the observed value is much lower than that found by this present study (r=0.826). Similar findings were obtained in a study by Guha et al [18] in which foot length was significantly correlated with birth weight, length, head circumference, chest circumference and gestational age. All the parameters showed strong and positive correlation coefficients. The maximum correlation was observed with birth weight and the least correlation with chest circumference, just like in the present study. A study by Gavhane et al [19] in Aurangabad also found similar positive and significant correlation between foot length and other anthropometric variables in both term and preterm infants.
Conclusion
In the setting of the present study, there was a strong positive correlation between foot-length and BW, CC and OFC with OFC having the least correlation. Correlation coefficients were 0.826, 0.783 and 0.801 for BW, CC and OFC respectively [20,21].
Recommendations
The recommendations, based on the findings of this study are as follows:
1. Foot length measurements may be adopted to be part of routine examination of newborn babies.
2. The use of foot length measurements may be promoted for use as a surrogate for BW in the assessment of newborn babies especially in the rural settings when weighing scale and the expertise required for measurement of other anthropometric indices are not available.
Competing Interests
The authors have declared that no competing interests exist.
Author’s Contributions
Principal researcher, Dr Nzeduba designed the work, collected the data and wrote up the article. Dr. Asinobi I.N supervised the work, Dr Eneh C.I reviewed the work and did the correspondence.
References
- Levels and Trends in child mortality: Report 2017 (from world bank, WHO, UN department of Economic and Social affairs, UN children’s fund).
- WHO (2007) National and perinatal mortality. In: Safer MP (Ed) Country, regional and global estimates 2004. Geneva, Switzerland.
- Monitoring the situation of children and women.
- Chimbira THK (1989) Uncertain gestation and pregnancy outcome. Cent Afr J Med 35: 333-342.
- Lucas A (1993) Enteral nutrition. In: Tsang R, Lucas A, Uaay R, Zlotkin S (Eds) Nutritional Needs of the Preterm Infant: Scientific Basis and Practical Guidelines. Williams and Wilkins, Baltimore, Pp. 209-224.
- Cooke RW, Lucas A, Yudkin PL, Pryse DJ (1977) Head circumference as an index of brain weight in the fetus and newborn. Early Hum Dev 1(2): 145-149.
- Sparks JW, Ross JC, Cetin I (1992) Intrauterine growth and nutrition. In: Polin RA and Fox WW (Eds) Fetal and Neonatal Physiology. WB Saunders, Philadelphia, Pp. 267-290.
- Bahl R, Martines J, Bhandari N, Biloglav Z, Edmond K, et al. (2012) Setting research priorities to reduce global mortality from preterm birth and low birth weight by 2015. J Glob Health 2(1): 10403.
- Kliegman RM (1996) The high risk infant. In: Nelson WE, Behrman RE, Kliegman RM, et al. (Eds) Nelson Textbook of Pediatrics. (15th edn), W.B. Saunders Company, Philadelphia, Pp. 451-463.
- Lawn JE, Kinney MV, Belizan JM, Mason EM, McDougall L, et al. (2013) Born too soon: accelerating actions for prevention and care of 15 million newborns born too soon. Reprod Health 10(Suppl 1): S6.
- Mullany LC, Darmstadt GL, Khatry SK, Leclerq SC, Tielsch JM (2007) Relationship between the surrogate anthropometric measures, foot length and chest circumference and birth weight among newborns of Sarlahi, Nepal. Eur J Clin Nutr 61(1): 40-46.
- Lewis TL and Chamberlain GV (1990) Obstetrics by Ten teachers. (15th edn), Edward Arnold, Pp. 33–62.
- Sasidharan K, Dutta S, Narang A (2009) Validity of New Ballard Score until 7th day of postnatal life in moderately preterm neonates. Arch Dis Child Fetal Neonatal Ed 94(1): F39–F44.
- Wyk LV, Smith J (2016) Postnatal Foot Length to Determine Gestational Age: A Pilot Study. J Trop Pediatr 62(2): 144-151.
- Anshuman S, Sharma U, Kumar S (2015) To study correlation of foot length and gestational age of new born by new Ballard score. Int J Res Med Sci 3(11): 3119-3122.
- Gowri S, Kumar V (2017) Clinical study of the correlation of foot length and birth weight among newborns in a tertiary care hospital. Int J Contemp Pediatr 4(3): 979.
- Hadush MY, Berhe AH, Medhanyie AA (2017) Foot length, chest and head circumference measurements in detection of Low birth weight neonates in Mekelle, Ethiopia: a hospital based cross sectional study. BMC Pediatr 17(1): 111.
- Natwar LG, Prachi SA, Dipti D, Shavi G, Shilpi G (2021) The Correlation between Foot Length and Birth Weight among Newborns. DOI: 10.7860/JCDR/2021/51867.15588.
- Gavhane S, Kale A, Golawankar A, Sangle A (2016) Correlation of foot length and gestational maturity in neonates. Int J Contemp Pediatr 3(3): 705-708.
- Raj AA (2020) Maheswari K. A cross-sectional study on the correlation between postnatal foot length and various other anthropometric parameters along with the gestational age. Pediatric Rev Int J Pediatr Res 7(8): 414-419.
- Mukherjee S, Roy P, Mitra S, Samanta M, Chatterjee S (2013) Measuring new born foot length to identify small babies in need of extra care: a cross-sectional hospital based study. Iran J Pediatr 23(5): 508-512.






























