Babywearing Practices and Effects on Parental and Child Physical and Psychological Health
Henrik Norholt1*, Raylene Phillips2, Joanna McNeilly3 and Charles Price4
1The Somatosensory & Affective Neuroscience Group, Liverpool, United Kingdom,
2School of Medicine, Loma Linda University, Loma Linda, California, USA
3Center for Babywearing Studies, NYC, New York, USA
4College of Medicine, University of Central Florida, Orlando, Florida, USA
Submission: May 09, 2022; Published: June 06, 2022
*Corresponding author:Henrik Norholt, The Somatosensory & Affective Neuroscience Group, Liverpool, United Kingdom
How to cite this article:Norholt H, Phillips R, McNeilly J, Price C. Babywearing Practices and Effects on Parental and Child Physical and Psychological Health. Acad J Ped Neonatol 2022; 11(5): 555876. 10.19080/AJPN.2022.11.555876
Abstract
An increasing number of parents engage in extended daily chest-to-chest contact with their full-term healthy infants for several months after birth as an extension of skin-to-skin contact in the early postpartum period. This practice is commonly known as “babywearing” (BW) and employs various carrying devices. The purpose of this review is to acquaint pediatricians and primary care providers with the numerous studies of physical, behavioral and social effects of BW as well as the different types of infant carriers and safe practices. BW studies demonstrate improved attachment and breastfeeding outcomes and infant sleep organization, as well as reduced maternal postpartum depressive symptoms and infant crying. BW is likely to strengthen paternal caregiving engagement, associated with positive child outcomes. The spread squat position for the hips during BW offers an optimal position for hip development and may prevent some forms of developmental hip dysplasia. BW may reduce the risk of positional plagiocephaly, by decreasing the time infants spend in the supine position while also allowing for spontaneous head movements. BW enables some mothers with short maternity leave to bring their infants to the workplace with limited interference in their tasks. Numerous designs of infant carriers are described along with basic safety precautions. Pediatricians may be key influencers for parents in achieving the positive outcomes described in this review.
Abbreviations: BW: Babywearing; OT: Oxytocin; SCS: Skin-to-skin Contact; US: United States
Introduction
Parents expect pediatricians to provide evidence-based advice about parenting methods. This review provides the scientific background for the increasingly popular parental practice of “babywearing” (BW). The term ‘babywearing’ is used here in place of the medically recognized term “infant carrying” to reflect parents’ likely language usage in the clinic.
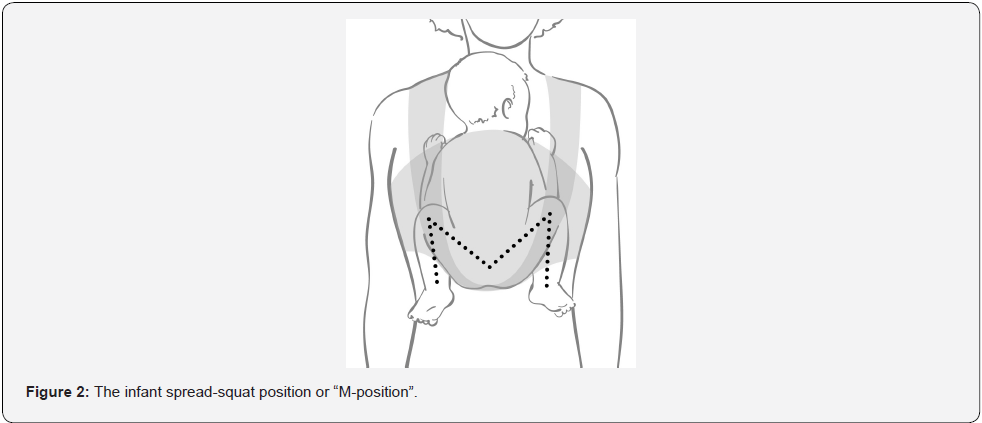
BW is characterized by the infant being carried for an extended period of time in an inward-facing spread-squat position on either the caregiver’s front, hip or back.
BW may improve child psychological resilience as well as ameliorate frequently encountered clinical challenges related to infant sleep, crying and breastfeeding. BW may also improve maternal mental health as well as fathers’ early childcare involvement and may allow mothers to return to work along with their infants. Physical benefits may include decreased risks of hip dysplasia and positional plagiocephaly.
Background
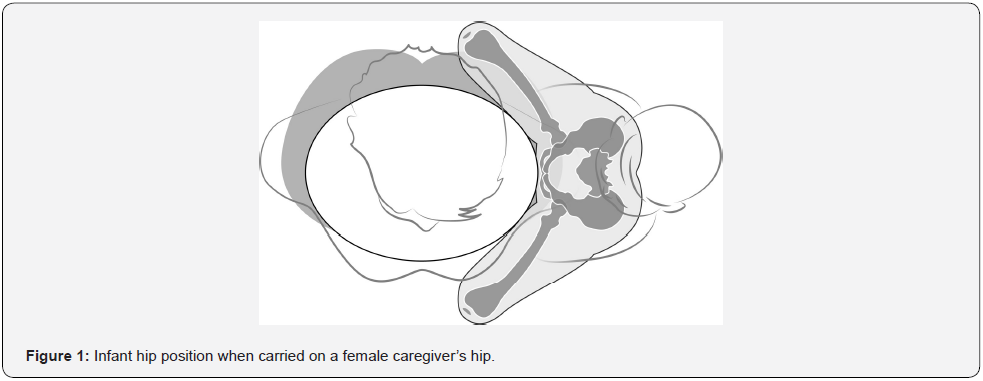
The infant as a parent-clinger
The newborn infant has palmar and plantar grasp reflexes that suggest clinging is a natural behavior. In addition, when lifted while supported underneath the arms, the newborn infant will instinctively flex the hips and knees and spread the thighs in preparation for being placed on the mother’s body [1]. The waist-to-hip ratio of females may also facilitate hip sitting position for BW [1,2]. These instinctive and anatomical characteristics suggest that humans are a parent-clinging species similar to other primates in that regard [2-4].
Pediatric support of child resilience
There is an increasing pediatric understanding of sub-optimal caregiving and environmental influences, resulting in child “toxic stress” that may impair development of physical and mental well-being [5]. At least one in five middle-class children will have experienced three or more adverse childhood experiences. The incidence for low-income groups is likely to be higher [6]. Approximately one in two adults will have an unresolved insecure relational history with caregivers, which is likely to be passed onto the next generation [7-9], evinced by estimates of up to 40% of infants categorized as insecurely attached [10]. Increased physical illness in adulthood has also been identified in individuals with insecure attachment as infants. In a longitudinal study, adults who exhibited insecure attachment patterns during infancy were four times more likely to report physical illness at age 32 years, compared to adults who were securely attached during infancy [11,12].
Pediatricians act as front-line guardians of healthy child development, as well as assume roles of leadership in devising new and effective interventions. Thus, knowledge of evidence to support BW is appropriate for pediatricians.
The sensitive period for contact goes beyond the first hour
A sensitive early postpartum period has been recognized during which iatrogenic mother-neonate separation is strongly contraindicated [13], influencing maternity ward practices worldwide [14]. Increasing the amount of parent-infant physical contact beyond the immediate postpartum period through BW offers a potential intervention pathway to secure attachment which can also involve other caregivers. This intervention mode is supported by the growing understanding of an “extended sensitive developmental period” [15-17]. During this period, both parents and infant require an array of mutual body-based kinesthetic [18-21], tactile [22-33], olfactory [34-36], audio [37-40] and visual [37,41-43] stimuli to develop optimum caregiving and utilize innate physiological co-regulatory systems. Oxytocin (OT) appears to be one of the central hormones involved in the early shaping of both the expression of parental caregiving behavior as well as infant development [23,44-47] and is released in response to tactile stimulation [48-54].
Behavioral Benefits of BW
Several trials have investigated the effects of extended mother-infant chest-to-chest contact beyond the first hour postpartum with regard to infant socio-emotional and other outcomes such as infant sleep, infant crying, breastfeeding, and postpartum depression, challenges frequently encountered in pediatric practice and sometimes difficult to manage. Handled unsuccessfully, these challenges may have long-term negative developmental effects [55-61].
In some trials, the mothers engaged in a high degree of skinto- skin contact (SSC) in order to maximize oxytocin release in mother and infant [62-65]. Other trials conformed to the current popular method of BW where mothers and infants are fully dressed [66,67]. Research in neonates suggests that the clothing barrier exerts only modest and non-significant effects on relevant outcomes, such as temperature regulation and longitudinal socioemotional development [24,68,69]. Hence, the clothed method of BW may suffice for mothers uncomfortable with the idea of extended SSC after the early neonatal period.
Parent-Infant Contact for Secure Attachment and Resilience
A landmark study of the effects of BW included mothers with social risk factors known to affect maternal-infant attachment [66]. The mothers were randomly assigned to receive either a soft carrier for BW or a plastic seat-type carrier with a handle for carrying and placing near the mother as needed. Evaluation at age 3,5 and 13 months respectively demonstrated that the mothers with the soft carrier had significantly greater maternal responsivity scores and 83% of their infants demonstrated secure parent-infant relations, compared to the group of infants in the seat-carrier group (38%). Amongst the subgroup of mothers who used the soft carriers on a daily basis, 93% of the infants demonstrated a secure attachment pattern, demonstrating a doseresponse relationship.
Another study similarly provided high-risk teenage mothers in the U.S. a soft structured carrier and encouraged BW for one hour daily for three months. A control group was given baby picture books to be read to their babies. Relative to the control group, the BW mothers and infants displayed significant more positive interactions during the Still Face test, indicating increased maternal sensitivity, supporting infant social and emotional development [67]. Employing an algorithm derived from the Global Rating scales of Mother-Infant Interaction [70], BW infants were found to be more likely to have a secure attachment and less likely to have disorganized attachment. A dose-response relationship between duration of BW and secure attachment was furthermore established [67].
A group of Canadian low-risk mothers of full-term infantsmaintained SSC daily during the first month postpartum [62]. In comparison to the control group with negligible SSC-exposure, at three months the SSC infants showed greatly accelerated socioemotional development during the Still Face test [71], responding with behaviors normally expected at 6-7 months of age [72]. Such early-age Still Face test behavior predicts later healthy parent-child relations [73-75]. A 9-year follow-up confirmed this prediction, with SSC children displaying greater mother-child reciprocity, which is linked to improved stress regulation [76].
Breastfeeding
The links between physical contact and oxytocin [50] as well as between oxytocin and breastfeeding [77] suggest that BW may support optimum breastfeeding outcomes. An Italian study randomized 200 middle-class mothers to receive either a commercial BW device or a pamphlet with information about breastfeeding at discharge from the maternity ward. The BW mothers were found to be significantly more likely to breastfeed at two (72% vs. 51%) and five months (48% vs. 24%) and were breastfeeding significantly more frequently [78]. A US study randomized 100 low-income mothers to receive either a baby carrier or be assigned to a wait control group. Parents in the intervention group were significantly more likely to be breastfeeding or feeding expressed human milk at 6 months than control group parents (68% vs. 40%.) Exclusive human milk feeding did not differ significantly between groups at 6 months (intervention versus control 49% vs 26%, P=,06) [79].
Recognizing a newborn’s subtle early hunger cues is an important skill mothers learn with each new baby. Mother–infant physical contact has been shown to predict feeding in response to early hunger cues when mother–infant proximity (without physical contact) did not [80]. Increased physical contact (which BW provides) promotes more frequent breastfeeding, which helps to establish and maintain mother’s milk supply and to ensure optimal nutrition for baby.
Canadian low-risk mothers who implemented daily SSC in the first postpartum month were more likely to maintain breastfeeding at three months, compared to mothers in the control group with limited SSC [63]. Amongst low-risk London- and Copenhagenbased mothers, the duration of daily mother-infant physical contact was found to correlate positively with breastfeeding outcomes at 12 weeks [81]. In Swedish breastfeeding dyads with severe latch-on problems, SSC during breastfeeding enhanced maternal positive feelings and shortened the time it took to resolve severe latch-on problems [82]. By supporting increased duration of breastfeeding, BW contributes to decreased risks for a range of physical illness for both mother and child [63,80-82].
Crying & Colic
Most mothers will respond intuitively to a crying infant by picking it up and placing it chest-to-chest, while engaging in rhythmical rocking movements. Such stimuli resemble those an infant will experience during BW, lending credence to a potential BW impact to decrease infant crying.
In a randomized study of the effects of BW on infant crying, mothers in the intervention group were encouraged to engage in extended BW when their babies were 4 weeks of age, while mothers in the control group were not given information about BW. In this study, extended BW resulted in a reduction of daily infant crying by 43% (1.23 vs. 2.16 h/d) at 6 weeks of age, when infant crying normally peaks [83]. In a high-risk sample, at two months postpartum, only 21% of carried infants had a regular daily period of crying, compared to 52% in the control group, whose mothers were issued a plastic infant seat at birth [66]. This finding, however, could not be replicated in a similar study [84]. In a longitudinal observational study of London and Copenhagen parents, the daily duration of parent-infant contact correlated with decreased duration of daily infant crying. London parents engaged in significantly less contact than Copenhagen parents, and their infants were found to cry 50% more than Copenhagen infants [81].
Compared to being held by a sedentary mother, infants whose mothers engaged in brisk walking immediately ceased crying and excessive movements and furthermore demonstrated reduced heart rate and increased heart rate variability, indicative of physiological calming [85,86].
Approximately 15-20% of infants may suffer from unsoothable crying/colic [87,88]. BW by itself has not been shown to be effective as a preventive [81,84] or therapeutic [89] approach to colic. At present, there are no generally effective therapies, and the etiology remains elusive [57,90-92]. Infant frequent feeders (>11 feeds/24 hours) are less likely to have daytime sleep or cry problems at 4 months [93]. BW has been showed to facilitate frequent and time-efficient breastfeeding [78,94] and may therefore modify colic. The therapeutic effects of BW-related vestibular stimulation merits further exploration [85].
Infant Sleep
Neonatal sleep regulation appears to underpin social and cognitive development. Improved socio-emotional and cognitive outcomes at five-year follow-up have been identified for neonates whose sleep/wake patterns are predominantly characterized by alternating between quiet sleep (as opposed to active sleep) and quiet wakefulness (unlike crying) [59]. The wide range of sensory stimulation inherent in parent-infant contact [95-97] and infant hormonal adaptation (notably oxytocin) [50] may influence infants’ state organization during sleep [98].
A study of the effects of parent-infant contact on sleep in full-term infants using a within-subjects design, demonstrated a significant, seven times increase in quiet sleep when 2-day-old infants were held in skin-to-skin contact compared to being placed separately in a cot [65]. Such early, more optimum sleep pattern configuration may have long-term consequences since high levels of quiet sleep at birth is a significant predictor for self-soothing at 12 months [99]. A study of parent-infant contact for pre-term infants demonstrated that early SSC predicted significantly improved sleep patterns and sleep efficiency at age 10 years [17].
Neonatal tactile stimulation in full-term infants has been shown to enhance circadian rhythms, and promote adjustment of restactivity and melatonin secretion rhythms in the nocturnal period [100]. Furthermore, providing rhythmical movement to both pre- and full-term infants has been shown to positively influence infant sleep-wake state organization (greater proportions of quiet sleep and quiet alert states) [86,101-103] as well as behavioral and physiological calming [85]. The natural movement of an active caregiver can supply such rhythmical stimuli to a carried baby.
Maternal Mental Health
Postpartum depression and anxiety affect up to 12-24% of women in industrialized countries, with the highest prevalence in low-income mothers [104,105]. The negative long-term effects on child development include deficits in cognitive and socioemotional development as well as behavioral challenges [106]. The American Academy of Pediatrics recommends that pediatric practices incorporate recognition and management of perinatal depression [106].
Consistent with the anxiolytic, stress-reducing and pro-social parenting properties of oxytocin [23,44,107], SSC may alleviate maternal depressive [64] and anxiety symptoms and improve parenting behaviors [17]. Physiological markers of stress, such as respiratory rate, blood pressure [108] and salivary cortisol [64], are positively influenced in mothers providing SSC. In an online survey, repetitive negative thinking (a risk factor for the development and maintenance of various mental disorders) was found to be significantly lower, and positive mental health was significantly higher while BW compared to overall levels in non- BW conditions [109]. Associations between early postpartum depressive symptoms and breastfeeding outcomes have been demonstrated [110,111]. The directionality of the association is far from clear [112,114], but the hormonal effect of SSC is known to improve breastfeeding outcomes, which then again may improve depressive symptoms [23,114-116].
BW combined with daytime walks and participation in mothers’ support groups may constitute a low-cost intervention against mild depression, given the documented effects of bright light [117-119], exercise [120] and social support on depression [121,122].
Paternal Involvement
Fathers’ caregiving patterns towards infants tend to differ from mothers’ with a greater emphasis on extrovert activities, animating infant exploration of the outer world and providing proprioceptive (rough and tumble) stimulation [123,125]. Fathers may contribute to security of exploration, defined as “confident, attentive, eager and resourceful exploration of materials and tasks, especially when a child faces disappointment [126].” Fathers contribute uniquely to children’s cognitive, language and social development [127-129]. Fathers’ brains appear sensitive to caregiving experiences, with increased involvement correlating with activation of care-related brain centers and oxytocin systems [130]. Father-infant SSC improves paternal role attainment, increases paternal interactive behavior, and reduces paternal stress and anxiety [131]. Father BW enhances amygdala response to infant crying, thereby promoting attention to and accurate perception of infant signals. Interestingly and relevant to intervention programs, the effects of BW were even more pronounced amongst fathers with more adverse childhood experiences [132].
Physical Benefits of BW
Hip Development and Hip Dysplasia
Postnatal practices may influence the risk of late hip dysplasia. The spread squat position for the infant’s hips when BW is an optimal position for hip development, while swaddling in the opposite position with the hips and knees extended increases the risk of hip dislocation [133-136].
Physical examination alone is an unreliable method for detecting infantile hip dislocations, and dislocations without risk factors are more likely to be detected after the age of three months [137,138]. A large majority of hip dysplasia cases go undetected during childhood and are initially diagnosed during adolescence or early adulthood as acetabular dysplasia [139].
It remains unknown whether these cases of acetabular dysplasia are the result of inadequate hip development during early infancy, or deficient growth during later in childhood. Nonetheless, the only opportunity to influence this process is during early infancy when the hip is pliable and developing rapidly. Hip ultrasound studies have shown that a deeper acetabulum in early infancy correlates with improved hip development during growth [140].
The optimum position for acetabular development is achieved with the hips flexed 100° to 110° and each hip abducted approximately 40° [135,136]. This is approximately the position achieved by the Pavlik harness and by BW when infant’s buttocks are below the knees and the thighs are spread around the mother’s torso (Figure 1).
This optimum position for hip development may explain why cultures that carry their babies in the spread squat position during early childhood (BW) have very low prevalence of hip dysplasia and low risk of adult hip arthritis [141].
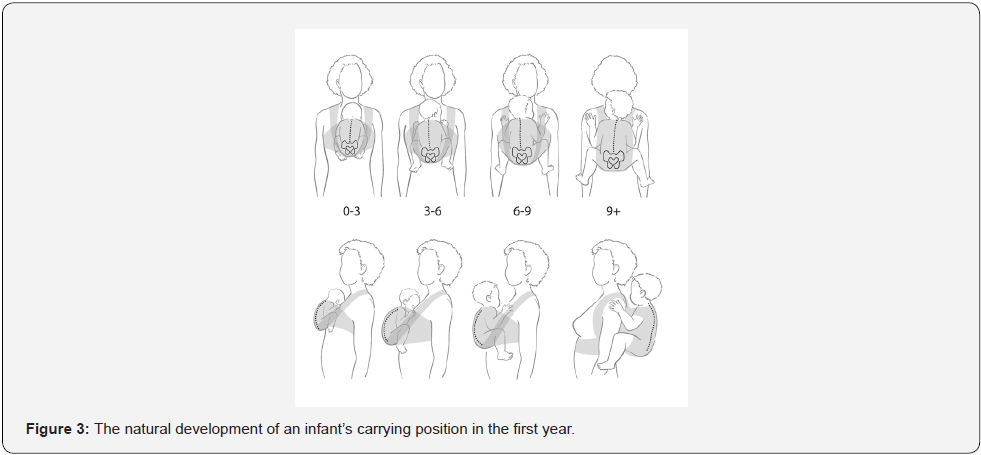
Anatomical and biomechanical studies have verified that the spread squat position is optimal for hip development [142]. This is often referred to as the “M-position” with the knees higher than the buttocks (Figure 2). However, the effects of intermediate positions are still unknown. Anatomical studies of infants have demonstrated that increased hip flexion requires less abduction for the hips to be centered in the acetabulum. As the child grows, more abduction is accompanied by decreased hip flexion to maintain the femoral head in the center of the acetabulum (Figure 3).
Cranial Shape and Plagiocephaly
There has been a significant increase in positional plagiocephaly in children throughout the world since the early 1990’s [143]. The benefits of the “Back-to-Sleep” campaign for prevention of Sudden Infant Death Syndrome are well known. However, this campaign was a likely contributor to the rise in prevalence of positional plagiocephaly, which has gone from 0.3% in 1974 to up to 47% [144,145].
In general, repositioning is recommended as first line therapy for infants younger than four months or for infants with mild to moderate asymmetry. Infants who are given activities that promote spontaneous physical movement have decreased risk for incidence and severity of plagiocephaly compared to infants who spend more time in the supine position [146]. There is a limited time window for repositioning treatment, as about 80% of cranial growth occurs before the first 12 months of age [147]. Helmet therapy is recommended for infants with severe deformational plagiocephaly or if moderate plagiocephaly persists after 4-6 months of age [143,148,149]. A major limitation to helmet therapy is related to cost of the cranial orthoses and need to wear the helmet 23 hours a day for a minimum of 3-4 months duration [148]. There are other limitations of repositioning treatment, including the need for frequent repositioning and increased prone positioning during periods of wakefulness. Non-compliance may be one reason why approximately 30% of infants who receive positional therapy continue to have some level of skull deformation at six months of age [150].
BW may be a useful practice to reduce the risk of positional plagiocephaly because upright BW decreases the amount of time that babies spend lying on their back or being in a position where their head is resting on a flat surface [151]. After development of head control, carried infants may spontaneously change head position during the natural movements of the mother. This potential for improved psychomotor development may also benefit children with psychomotor delays associated with excessive duration of supine positioning [152].
Potential Benefits
Parenting in the workplace
Only about half of the 185 surveyed countries live up to the recommendation of the International Labour Organization of minimum 14 weeks of statutory maternity leave [153]. The United States (US) currently provides 12 weeks of unpaid maternity leave, whichis the lowest level of support amongst countries belonging to the Organization for Economic Co-operation and Development [154]. In the US, the length of maternity leave has been found to negatively influence breastfeeding outcomes [155,156], the quality of mother-infant interactions, and infant attachment outcomes [157], as well as maternal mental health [158].
Bringing a pre-crawling baby (< age 7 months) to the workplace in an infant carrier is one potential interim solution to short statutory maternity leave. To date, 2,100 US infants in 200 companies, spanning 30 industries have been brought to work through formalized parenting-in-the-workplace programs. Outcomes include higher staff retention rates, earlier return to the workplace (mitigating temporary workers costs), increased morale and teamwork, higher dedication to employer (impacting long-term productivity), and increased breastfeeding rates [159].
Products, Practice and Safety
Types of Carriers
The styles of carriers fall into several groups that may be characterized as wraps, slings, structured soft carriers, and others (Figure 4).
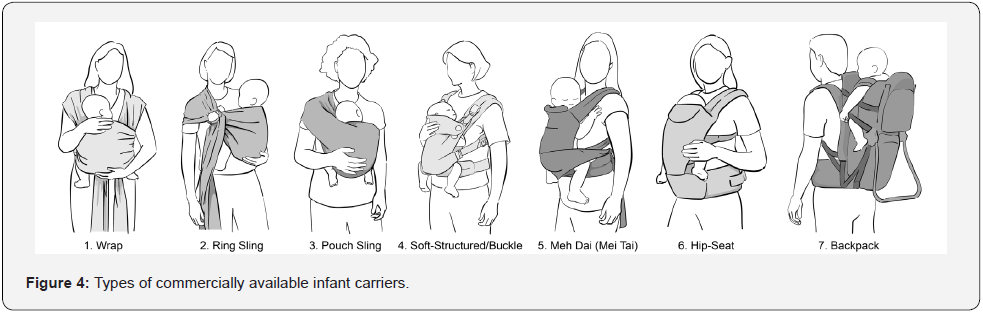
1. Wraps: A traditional type of carrier that consists of a broad swath of fabric that is wrapped around the mother and infant in various configurations. Using a wrap requires some learning but constitutes a relatively inexpensive and adjustable method for BW.
2. Slings: Fabric carriers that are easily stored, quick to use and easily adjusted. This type of carrier can be useful for infants and toddlers who may be up and down frequently. However, the risk of suffocation may be increased if an infant is in a side-lying position or if the head becomes covered.
3. Structured soft carriers are the most widely used commercial products. These are also called buckle carriers and come in a wide variety of sizes, materials and prices.
4. Other types of carriers include varieties and mixtures of wraps, slings and soft-structured carriers. Some provide a wide band of support or a seat underneath the infant’s buttocks. Frame pack carriers are specifically designed for hiking.
Positioning and Safety
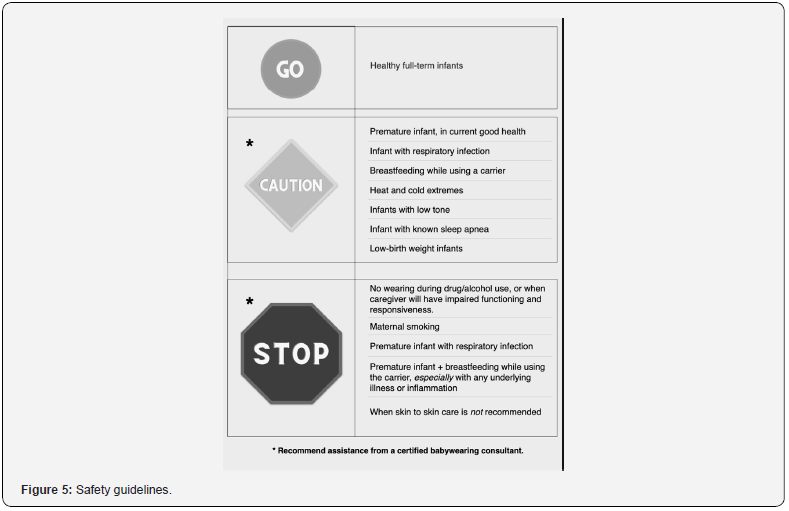
Caution should be advised, or BW should be discouraged, when infants have a respiratory infection, during breastfeeding,in extreme weather conditions, for infants with sleep apnea or low motor tone, or when the caregiver is impaired, or uses drugs, alcohol, or cigarettes on a regular basis (Figure 5).
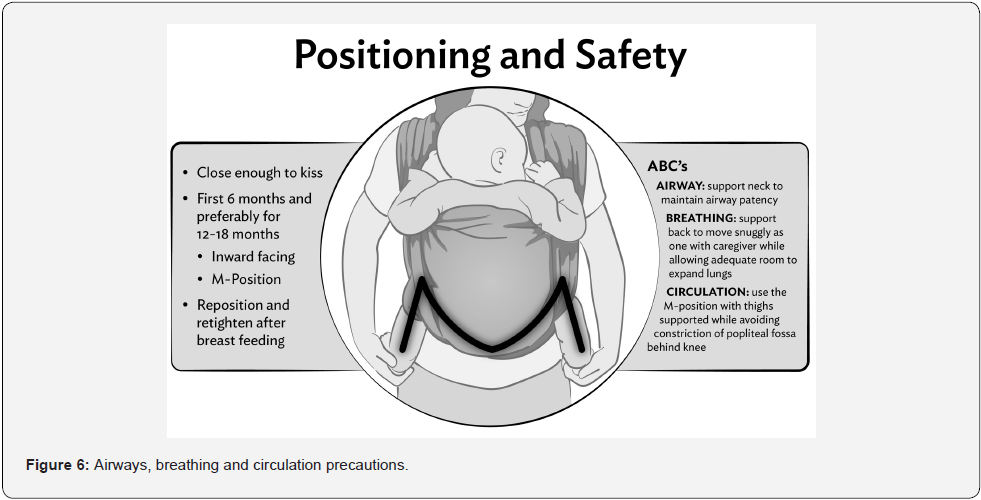
The carrier should support the infant from knee to neck until the infant achieves sufficient head and trunk control. The infant’s legs should be supported from the knee and held in an M-position where the knees are higher than the baby’s buttocks.
Side-lying position of the infant in a sling is associated with the greatest risk of suffocation. In addition, this position holds the thighs together similar to tight swaddling; therefore, this position should be avoided. When using any baby carrier, the standard ABC’s of Airway, Breathing, and Circulation can be used to mitigate potential risks for the infant and the wearer (Figure 6).
Some BW devices enable front facing forward of the infant. This position is controversial, as it tends to place the infant hips extended and with limited abduction in a suboptimal position for healthy hip development during early infancy [160]. The infant’s social referencing to caregiver’s face (regulating infant stress to novel stimuli) is also prevented, possibly leading to overstimulation and elevated stress levels for young or sensitive young infants [161]. For parents desiring to face their baby forward, several carrier designs now exist that support a marginally ergonomic position in the front facing forward mode. Current manufacturer recommendations are to place infants in the front facing forward position no earlier than at 5-6 months of age. However, the forward-facing position is advised primarily for short low-stimulus sessions.
Risks of BW
The injury-related risks associated with BW are generally from misuse of the product or from old or faulty carriers. However, trips and falls of the wearer may occur due to the added weight of the infant or because of improper distribution of the infant’s weight on the wearer. Drops and falls of the infant are most common during placement in or removal from the carrier. When the infant is larger, reported injuries are more likely to be related to cooking, and bumps from furniture and corners [162].
Head injuries and striking of objects may result from a fall, drop, or lack of attention to furniture and doorways. Additionally, wear and tear of carriers or buckle failure can add to the risk of sudden unexpected falls. Older, second hand, and poorly designed carriers may contribute to the risk of injury [163]. Improperly tightened carriers can cause the carrier to be loose, allowing the baby to slip out when the caregiver bends over. The risk of suffocation and positional asphyxia are greater for infants younger than four months, especially in the presence of underlying conditions, head covering, maternal smoking, and while breastfeeding (see Figure 5) [164,165]. These and other reports emphasize the need to encourage parents to avoid holding the infant too low, breastfeeding in the carrier, covering the head, or positioning so that the head cannot be seen easily. Parents should also be encouraged to read instructions carefully, and to be vigilant when placing the infant in the carrier or removing the infant from the carrier.
Duration
The duration of daily SSC/BW depends on parental and infant preferences. Positive outcomes for breastfeeding and infant socioemotional development have been found with approximately one hour of daily BW [67,78]. However, a dose-response effect has been shown for socio-emotional and resilience outcomes,so parents should be encouraged to carry as much as possible and not merely limit carrying to transport situations [66]. Infant interest and desire for BW may decrease as the infant engages in developmentally appropriate locomotion and environmental exploration at around 7-9 months [161].
Additional guidance has been designed by the trade organization Baby Carrier Industry Alliance for safe Infant Carrying [166]. In the US, The Center for Babywearing Studies provides education and support for interested parents and providers [167]. Certified BW consultants are available for parents who need additional support.
Conclusion
Pediatricians can influence long-term health and well-being by recommending simple interventions during early childhood to improve parenting and infant outcomes. BW during the first months of life is a simple, low-cost preventive intervention, which may help pediatricians resolve several frequently encountered, intractable clinical challenges, including poor parental bonding, non-optimum parenting behaviors, early discontinuation of breastfeeding, parental postpartum depression, infant poor sleep and crying, developmental dysplasia of the hip, positional plagiocephaly as well as early-return-to-work-induced separation issues for both parent and infant. For safety and comfort reasons, parents should be advised to employ ergonomically suitable BW devices, which support both the caregiver’s and the infant’s healthy posture, while protecting infant airways. BW promotes the development of emotional connections between parents and their infants, thus supporting secure attachments and forming the foundation for healthy relationships, which are known contribute to physical and emotional health and wellbeing throughout the lifespan. This simple, low-cost intervention at the beginning of life has well-documented short- and long-term benefits for babies and families and, thus, has the potential to benefit society as a whole.
Article Summary
abywearing effects on child physical and psychological health and describes types of carriers and safe practices
Conflict of Interest Disclosures (includes financial disclosures): HN received consultancy fees from the baby carrier manufacturer Ergobaby Inc. during the initial conception and drafting of the article. HN had no conflict of interest during the completion of the drafting and critical revision of the article. At the time of submission, HN owns a company engaged in consultancy, design and brand development of baby carriers. Joanna McNeilly receives income from educating babywearing consultants. The other authors have no conflicts of interest to disclose.
Contributors’ Statement
Dr. H Norholt, PhD and Prof C Price, MD conceptualized and designed the article, drafted the initial manuscript, and reviewed and revised the manuscript.
Prof R Phillips, MD drafted the initial manuscript and critically reviewed the manuscript for important intellectual content.
Ms J McNeilly, BFA drafted the initial manuscript and reviewed and revised the manuscript.
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
References
- Kirkilionis E (1997) Die Grundbedürfnisse des Säuglings und deren medizinische Aspekte - dargestellt und charakterisiert am Jungentypus Tragling. Notabene Medici 27(2): 61-66.
- Kirkilionis E (2014) A Baby Wants to Be Carried: Everything You Need to Know about Baby Carriers and the Benefits of Babywearing. (1st Edn), Pinter & Martin Ltd, UK.
- Büschelberger J (1931) Studies on the Peculiarities of the Hip Joint in Infancy and Their Role in Pathogenesis, Prophylaxis and the Treatment of Hip Luxation. Medical Academy “Carl Gustav Carus” in Dresden; 1961.
- Hassenstein B (1970) Tierjunges und Menschenkind im Blick der vergleichenden Verhaltensforschung. Berichte Naturwissenschaftlich-Med Ver Innsbr 58: 35-50.
- Shonkoff JP, Garner AS, Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care, et al. (2012) The Lifelong Effects of Early Childhood Adversity and Toxic Stress. Pediatrics 129(1): e232-e246.
- About the CDC-Kaiser ACE Study (2016) Child Maltreatment|Violence Prevention|Injury Center|CDC.
- Van IJzendoorn MH, Bakermans-Kranenburg MJ (1996) Attachment representations in mothers, fathers, adolescents, and clinical groups: a meta-analytic search for normative data. J Consult Clin Psychol 64(1): 8-21.
- Fonagy P, Steele H, Steele M (1991) Maternal representations of attachment during pregnancy predict the organization of infant-mother attachment at one year of age. Child Dev 62(5): 891-905.
- Van IJzendoorn MH (1995) Adult attachment representations, parental responsiveness, and infant attachment: a meta-analysis on the predictive validity of the Adult Attachment Interview. Psychol Bull 117(3): 387-403.
- Moullin S, Waldfogel J, Washbrook E (2014) Baby Bonds: Parenting, Attachment and a Secure Base for Children. The Sutton Trust.
- Puig J, Englund MM, Simpson JA, Collins WA (2013) Predicting adult physical illness from infant attachment: a prospective longitudinal study. Health Psychol Off J Div Health Psychol Am Psychol Assoc 32(4): 409-417.
- Farrell AK, Waters TEA, Young ES, Englund MM, Carlson EE, et al. (2019) Early maternal sensitivity, attachment security in young adulthood, and cardiometabolic risk at midlife. Attach Hum Dev 21(1): 70-86.
- Klaus MH, Kennell JH (1976) Maternal-Infant Bonding. C.V. Mosby Company.
- World Health Organization (2009) Baby-Friendly Hospital Initiative Revised, Updated and Expanded for Integrated Care.
- Feldman R (2015) Sensitive periods in human social development: New insights from research on oxytocin, synchrony, and high-risk parenting. Dev Psychopathol 27(2): 369-395.
- Polaan H, Hofer MA (2008) Psychobiological Origins of Infant Attachment and Its Role in Development. In: Cassidy J, Shaver PR, eds. Handbook of Attachment Second Edition Theory, Research, and Clinical Applications. Guilford Press.
- Feldman R, Rosenthal Z, Eidelman AI (2014) Maternal-preterm skin-to-skin contact enhances child physiologic organization and cognitive control across the first 10 years of life. Biol Psychiatry 75(1): 56-64.
- Mason WA, Berkson G (1975) Effects of maternal mobility on the development of rocking and other behaviors in rhesus monkeys: A study with artificial mothers. Dev Psychobiol 8(3): 197-211.
- Dettmer AM, Ruggiero AM, Novak MA, Meyer JS, Suomi SJ (2008) Surrogate mobility and orientation affect the early neurobehavioral development of infant rhesus macaques (Macaca mulatta). Dev Psychobiol 50(4): 418-422.
- Esposito G, Setoh P, Yoshida S, Kuroda KO (2015) The calming effect of maternal carrying in different mammalian species. Front Psychol 6: 445.
- Anderson CO, Mc Kenney AM, Mason WA (1977) Effects of maternal mobility, partner, and endocrine state on social responsiveness of adolescent rhesus monkeys. Dev Psychobiol 10(5): 421-434.
- Harlow HF, Harlow MK (1966) Learning to love. Am Sci 54(3): 244-272.
- Uvnäs-Moberg K (2015) Oxytocin: The Biological Guide to Motherhood. Hale Publishing.
- Bystrova K, Ivanova V, Edhborg M, Matthiesen A-S, Ransjö-Arvidson A-B, et al. (2009) Early contact versus separation: effects on mother-infant interaction one year later. Birth Berkeley Calif 36(2): 97-109.
- Feldman R, Weller A, Leckman JF, Kuint J, Eidelman AI (1999) The nature of the mother’s tie to her infant: maternal bonding under conditions of proximity, separation, and potential loss. J Child Psychol Psychiatry 40(6): 929-939.
- Feldman R (2015) The adaptive human parental brain: implications for children’s social development. Trends Neurosci 38(6): 387-399.
- Feldman R, Weller A, Sirota L, Eidelman AI (2003) Testing a family intervention hypothesis: the contribution of mother-infant skin-to-skin contact (kangaroo care) to family interaction, proximity, and touch. J Fam Psychol JFP J Div Fam Psychol 17(1): 94-107.
- Bergman NJ (2014) The neuroscience of birth--and the case for Zero Separation. Curationis 37(2): 1-4.
- Welch MG, Myers MM, Grieve PG, Isler JR, Fifer WP, et al. (2014) Electroencephalographic activity of preterm infants is increased by Family Nurture Intervention: a randomized controlled trial in the NICU. Clin Neurophysiol 125(4): 675-684.
- Welch MG, Halperin MS, Austin J, Stark RI, Hofer MA, et al. (2016) Depression and anxiety symptoms of mothers of preterm infants are decreased at 4 months corrected age with Family Nurture Intervention in the NICU. Arch Womens Ment Health 19(1): 51-61.
- Welch MG, Firestein MR, Austin J, Hane AA, Stark RI, et al. (2015) Family Nurture Intervention in the Neonatal Intensive Care Unit improves social-relatedness, attention, and neurodevelopment of preterm infants at 18 months in a randomized controlled trial. J Child Psychol Psychiatry 56(11): 1202-1211.
- Mariani Wigley ILC, Mascheroni E, Bonichini S, Montirosso R (2022) Epigenetic protection: maternal touch and DNA-methylation in early life. Curr Opin Behav Sci 43: 111-117.
- Montirosso R, McGlone F (2020) The body comes first. Embodied reparation and the co-creation of infant bodily-self. Neurosci Biobehav Rev 113: 77-87.
- Kaitz M, Good A, Rokem AM, Eidelman AI (1987) Mothers’ recognition of their newborns by olfactory cues. Dev Psychobiol 20(6): 587-591.
- Porter RH, Makin JW, Davis LB, Christensen KM (1992) Breast-fed infants respond to olfactory cues from their own mother and unfamiliar lactating females. Infant Behav Dev 15(1): 85-93.
- Porter RH, Cernoch JM, McLaughlin FJ 1983() Maternal recognition of neonates through olfactory cues. Physiol Behav 30(1):151-154.
- Brazelton TB, Nugent JK (1995) Neonatal Behavioral Assessment Scale. Cambridge University Press.
- Kim P, Feldman R, Mayes LC, Eicher V, Thompson N, et al. (2011) Breastfeeding, brain activation to own infant cry, and maternal sensitivity. J Child Psychol Psychiatry 52(8): 907-915.
- Rand K, Lahav A (2014) Maternal sounds elicit lower heart rate in preterm newborns in the first month of life. Early Hum Dev 90(10): 679-683.
- Imafuku M, Hakuno Y, Uchida-Ota M, Yamamoto J ichi, Minagawa Y (2014) “Mom called me!” Behavioral and prefrontal responses of infants to self-names spoken by their mothers. NeuroImage 103: 476-484.
- Farroni T, Johnson MH, Menon E, Zulian L, Faraguna D, et al. (2005) Newborns’ preference for face-relevant stimuli: Effects of contrast polarity. Proc Natl Acad Sci U S A 102(47): 17245-17250.
- Simion F, Giorgio ED (2015) Face perception and processing in early infancy: inborn predispositions and developmental changes. Front Psychol 6: 969.
- Stern DN (2004) The First Relationship: Infant and Mother, With a New Introduction. Harvard University Press.
- Feldman R (2016) The neurobiology of mammalian parenting and the biosocial context of human caregiving. Horm Behav 77: 3-17.
- Insel TR, Young LJ (2001) The neurobiology of attachment. Nat Rev Neurosci 2(2): 129-136.
- Kim S, Strathearn L (2016) Oxytocin and Maternal Brain Plasticity. New Dir Child Adolesc Dev 2016(153): 59-72.
- Strathearn L, Fonagy P, Amico J, Montague PR (2009) Adult attachment predicts maternal brain and oxytocin response to infant cues. Neuropsychopharmacol Off Publ Am Coll Neuropsychopharmacol 34(13): 2655-2666.
- Matthiesen AS, Ransjö-Arvidson AB, Nissen E, Uvnäs-Moberg K (2001) Postpartum maternal oxytocin release by newborns: effects of infant hand massage and sucking. Birth Berkeley Calif 28(1): 13-19.
- Stock S, Uvnäs-Moberg K (1988) Increased plasma levels of oxytocin in response to afferent electrical stimulation of the sciatic and vagal nerves and in response to touch and pinch in anaesthetized rats. Acta Physiol Scand 132(1): 29-34.
- Moberg KU, Handlin L, Petersson M (2020) Neuroendocrine mechanisms involved in the physiological effects caused by skin-to-skin contact - With a particular focus on the oxytocinergic system. Infant Behav Dev 61: 101482.
- Hardin JS, Jones NA, Mize KD, Platt M (2020) Parent-Training with Kangaroo Care Impacts Infant Neurophysiological Development & Mother-Infant Neuroendocrine Activity. Infant Behav Dev 58: 101416.
- Norholt H (2020) Delivering Clinically on our Knowledge of Oxytocin and Sensory Stimulation: The Potential of Infant Carrying in Primary Prevention. Front Psychol 11: 590051.
- Vittner D, McGrath J, Robinson J, Lawhon G, Cusson R, et al. (2018) Increase in Oxytocin from Skin-to-Skin Contact Enhances Development of Parent-Infant Relationship. Biol Res Nurs 20(1): 54-62.
- Cong X, Ludington-Hoe SM, Hussain N, Cusson RM, Walsh S, et al. (2015) Parental oxytocin responses during skin-to-skin contact in pre-term infants. Early Hum Dev 91(7): 401-406.
- Douglas PS, Hiscock H (2010) The unsettled baby: crying out for an integrated, multidisciplinary primary care approach. Med J Aust 193(9): 533-536.
- Häggkvist AP, Brantsæter AL, Grjibovski AM, Helsing E, Meltzer HM, et al. (2010) Prevalence of breast-feeding in the Norwegian Mother and Child Cohort Study and health service-related correlates of cessation of full breast-feeding. Public Health Nutr 13(12): 2076-2086.
- St James-Roberts I (2008) Infant crying and sleeping: helping parents to prevent and manage problems. Prim Care 35(3): 547-567.
- Gartner LM, Morton J, Lawrence RA, Naylor AJ, O'Hare D, et al. (2005) Breastfeeding and the use of human milk. Pediatrics 115(2): 496-506.
- Weisman O, Magori-Cohen R, Louzoun Y, Eidelman AI, Feldman R (2011) Sleep-wake transitions in premature neonates predict early development. Pediatrics 128(4): 706-714.
- Stuebe A (2009) The risks of not breastfeeding for mothers and infants. Rev Obstet Gynecol 2(4): 222-231.
- Hemmi MH, Wolke D, Schneider S (2011) Associations between problems with crying, sleeping and/or feeding in infancy and long-term behavioural outcomes in childhood: a meta-analysis. Arch Dis Child 96(7): 622-629.
- Bigelow AE, Power M (2012) The effect of mother-infant skin-to-skin contact on infants’ response to the Still Face Task from newborn to three months of age. Infant Behav Dev 35(2): 240-251.
- Bigelow AE, Power M, Gillis DE, Maclellan-Peters J, Alex M, et al. (2014) Breastfeeding, skin-to-skin contact, and mother-infant interactions over infants’ first three months. Infant Ment Health J 35(1): 51-62.
- Bigelow AE, Power M, MacLellan-Peters J, Alex M, McDonald C (2012) Effect of mother/infant skin-to-skin contact on postpartum depressive symptoms and maternal physiological stress. J Obstet Gynecol Neonatal Nurs 41(3): 369-382.
- Morgan BE, Horn AR, Bergman NJ (2011) Should neonates sleep alone? Biol Psychiatry. 70(9): 817-825.
- Anisfeld E, Casper V, Nozyce M, Cunningham N (1990) Does infant carrying promote attachment? An experimental study of the effects of increased physical contact on the development of attachment. Child Dev 61(5): 1617-1627.
- Williams LR, Turner PR (2020) Infant carrying as a tool to promote secure attachments in young mothers: Comparing intervention and control infants during the still-face paradigm. Infant Behav Dev 58: 101413.
- Bystrova K, Widström AM, Matthiesen AS, A B Ransjö-Arvidson, B Welles-Nyström, et al. (2003) Skin-to-skin contact may reduce negative consequences of “the stress of being born”: a study on temperature in newborn infants, subjected to different ward routines in St. Petersburg. Acta Paediatr 92(3): 320-326.
- Filingeri D, Cowley H, Merrick C, Gang PS, Filingeri VL (2020) The effects of clothing layers on the thermoregulatory responses to short duration babywearing in babies under 12 months old. Physiol Rep 8(9): e14425.
- Abbott K (2016) Attachment during the First Year of Life: Validity and Longitudinal Associations to 14 Months, of Attachment Classification at 7 Months. Doctoral dissertation. University of Liverpool, Accessed January 4, 2020.
- Tronick E, Als H, Adamson L, Wise S, Brazelton TB (1978) The infant’s response to entrapment between contradictory messages in face-to-face interaction. J Am Acad Child Psychiatry 17(1): 1-13.
- Bigelow AE (2006) Infants held skin to skin six hours a day the first week and two hours a day the second through fourth week appear to be socially bidding to Mom at the age of three months in contrast to the age of seven months when social bidding has been recorded in previous studies. In: Sixth Biennial International Workshop of the International Network of Kangaroo Mother Care.
- Ainsworth MDS, Blehar MC, Waters E, Wall SN (2015) Patterns of Attachment: A Psychological Study of the Strange Situation. Psychology Press.
- Mesman J, van IJzendoorn MH, Bakermans-Kranenburg MJ (2009) The many faces of the Still-Face Paradigm: A review and meta-analysis. Dev Rev 29(2): 120-162.
- Barbosa M, Beeghly M, Moreira J, Tronick E, Fuertes M (2020) Emerging patterns of infant regulatory behavior in the Still-Face paradigm at 3 and 9 months predict mother-infant attachment at 12 months. Attach Hum Dev 23(6):814-830.
- Bigelow AE, Power M, MacLean K, Gillis D, Ward M, et al. (2018) Mother-Infant Skin-to-Skin Contact and Mother-Child Interaction Nine Years Later. Soc Dev 27(4): 937-951.
- Uvnäs Moberg K, Ekström-Bergström A, Buckley S, Massarotti C, Pajalic Z, et al. (2020) Maternal plasma levels of oxytocin during breastfeeding-A systematic review. PloS One 15(8): e0235806.
- Pisacane A, Continisio P, Filosa C, Tagliamonte V, Continisio GI (2012) Use of baby carriers to increase breastfeeding duration among term infants: the effects of an educational intervention in Italy. Acta Paediatr 101(10): e434-e438.
- Little EE, Cioffi CC, Bain L, Legare CH, Hahn-Holbrook J (2021) An Infant Carrier Intervention and Breastfeeding Duration: A Randomized Controlled Trial. Pediatrics 148(1): e2020049717.
- Little EE, Legare CH, Carver LJ (2018) Mother–Infant Physical Contact Predicts Responsive Feeding among U.S. Breastfeeding Mothers. Nutrients 10(9): 1251.
- St James-Roberts I, Alvarez M, Csipke E, Abramsky T, Goodwin J, et al. (2006) Infant crying and sleeping in London, Copenhagen and when parents adopt a “proximal” form of care. Pediatrics 117(6): e1146-e1155.
- Svensson KE, Velandia MI, Matthiesen AST, Welles-Nyström BL, Widström AME () Effects of mother-infant skin-to-skin contact on severe latch-on problems in older infants: a randomized trial. Int Breastfeed J 8(1): 1.
- Hunziker UA, Barr RG (1986) Increased carrying reduces infant crying: a randomized controlled trial. Pediatrics 77(5): 641-648.
- St James-Roberts I, Hurry J, Bowyer J, Barr RG (1995) Supplementary carrying compared with advice to increase responsive parenting as interventions to prevent persistent infant crying. Pediatrics 95(3): 381-388.
- Esposito G, Yoshida S, Ohnishi R, Tsuneoka Y, Rostagno MDC, et al. (2013) Infant calming responses during maternal carrying in humans and mice. Curr Biol CB 23(9): 739-745.
- Vrugt DT, Pederson DR (1973) The Effects of Vertical Rocking Frequencies on the Arousal Level in Two-Month-Old Infants. Child Dev 44(1): 205-209.
- Lucassen P, Assendelft W, van Eijk JTM, Gubbels J, Douwes A, et al. (2001) Systematic review of the occurrence of infantile colic in the community. Arch Dis Child 84(5): 398-403.
- St James-Roberts I, Halil T (1991) Infant crying patterns in the first year: normal community and clinical findings. J Child Psychol Psychiatry 32(6): 951-968.
- Barr RG, McMullan SJ, Spiess H, D G Leduc, J Yaremko, et al. (1991) Carrying as colic “therapy”: a randomized controlled trial. Pediatrics 87(5): 623-630.
- Lucassen P (2015) Colic in infants. BMJ Clin Evid 2015: 0309.
- Shamir R, St James-Roberts I, Di Lorenzo C, Burns AJ, Thapar N, et al. (2013) Infant crying, colic, and gastrointestinal discomfort in early childhood: a review of the evidence and most plausible mechanisms. J Pediatr Gastroenterol Nutr 57(Suppl 1): S1-S45.
- Daelemans S, Peeters L, Hauser B, Vandenplas Y (2018) Recent advances in understanding and managing infantile colic. F1000Res 7: F1000 Faculty Rev-1426.
- Hiscock H, Cook F, Bayer J, Ha N D Le, Mensah F, et al. (2014) Preventing early infant sleep and crying problems and postnatal depression: a randomized trial. Pediatrics 133(2): e346-e354.
- Winberg J (2005) Mother and newborn baby: mutual regulation of physiology and behavior--a selective review. Dev Psychobiol 47(3): 217-229.
- Tuulari JJ, Scheinin NM, Lehtola S, Merisaari H, Saunavaara J, et al. (2019) Neural correlates of gentle skin stroking in early infancy. Dev Cogn Neurosci 35: 36-41.
- Williams G, Fabrizi L, Meek J, Jackson D, Tracey I, et al. (1992) Functional magnetic resonance imaging can be used to explore tactile and nociceptive processing in the infant brain. Acta Paediatr 104(2): 158-166.
- Graham AM, Pfeifer JH, Fisher PA, Lin W, Gao W, et al. (2014) The potential of infant fMRI research and the study of early life stress as a promising exemplar. Dev Cogn Neurosci 12: 12-39.
- Van Puyvelde M, Mairesse O (2022) Do C-tactile afferents go to sleep? A potential role for somatosensory stimulation in sleep regulation. Curr Opin Behav Sci 43: 62-68.
- Burnham MM, Goodlin-Jones BL, Gaylor EE, Anders TF (2002) Nighttime sleep-wake patterns and self-soothing from birth to one year of age: a longitudinal intervention study. J Child Psychol Psychiatry 43(6): 713-725.
- Feldman R, Rosenthal Z, Eidelman AI () Maternal-preterm skin-to-skin contact enhances child physiologic organization and cognitive control across the first 10 years of life. Biol Psychiatry. 2014;75(1):56-64. doi:10.1016/j.biopsych.2013.08.012 [17]
- Ferber SG, Laudon M, Kuint J, Weller A, Zisapel N (2002) Massage therapy by mothers enhances the adjustment of circadian rhythms to the nocturnal period in full-term infants. J Dev Behav Pediatr 23(6): 410-415.
- Edelman AH, Kraemer HC, Korner AF (1982) Effects of Compensatory Movement Stimulation on the Sleep-Wake Behaviors of Preterm Infants. J Am Acad Child Psychiatry 21(6): 555-559.
- Korner AF, Grobstein R (1966) Visual Alertness as Related to Soothing in Neonates: Implications for Maternal Stimulation and Early Deprivation. Child Dev 37(4): 867-876.
- Korner AF, Schneider P, Forrest T (1983) Effects of vestibular-proprioceptive stimulation on the neurobehavioral development of preterm infants: a pilot study. Neuropediatrics 14(3): 170-175.
- Isaacs M (2004) Community Care Networks for Depression in Low-Income Communities and Communities of Color: A Review of the Literature. Howard University School of Social Work and the National Alliance of Multiethnic Behavioral Health Associations.
- Dunkel Schetter C, Tanner L (2012) Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice. Curr Opin Psychiatry 25(2): 141-148.
- Earls MF, Yogman WY, Mattson G, Rafferty J, COMMITTEE ON PSYCHOSOCIAL ASPECTS OF CHILD AND FAMILY HEALTH (2010) Incorporating Recognition and Management of Perinatal and Postpartum Depression into Pediatric Practice. Pediatrics 126(5): 1032-1039.
- Thul TA, Corwin EJ, Carlson NS, Brennan PA, Young LJ (2020) Oxytocin and postpartum depression: A systematic review. Psychoneuroendocrinology 120: 104793.
- Nimbalkar A, Patel D, Sethi A, Nimbalkar S (2014) Effect of skin to skin care to neonates on pulse rate, respiratory rate SPO2 and blood pressure in mothers. Indian J Physiol Pharmacol 58(2): 174-177.
- Schoppmann J, Teismann T, Holleck-Weithmann VA, Hundertmark E, Jandewerth K, et al. (2021) Infant carrying is associated with reduced maternal repetitive negative thinking and increased maternal mental health. J Reprod Infant Psychol 1-14.
- Hannah P, Adams D, Lee A, Glover V, Sandler M (1992) Links between early post-partum mood and post-natal depression. Br J Psychiatry J Ment Sci 160: 777-780.
- Hatton DC, Harrison-Hohner J, Coste S, Dorato V, Curet LB, et al. (2005) Symptoms of postpartum depression and breastfeeding. J Hum Lact 21(4): 444-449.
- Dias CC, Figueiredo B (2015) Breastfeeding and depression: a systematic review of the literature. J Affect Disord 171: 142-154.
- Figueiredo B, Dias CC, Brandão S, Canário C, Nunes-Costa R (2013) Breastfeeding and postpartum depression: state of the art review. J Pediatr (Rio J) 89(4): 332-338.
- Ip S, Chung M, Raman G, Chew P, Magula N, et al. (2007) Breastfeeding and maternal and infant health outcomes in developed countries. Evid ReportTechnology Assess (153): 1-186.
- Abou-Saleh MT, Ghubash R, Karim L, Krymski M, Bhai I (1998) Hormonal aspects of postpartum depression. Psychoneuroendocrinology 23(5): 465-475.
- Warner R, Appleby L, Whitton A, Faragher B (1996) Demographic and obstetric risk factors for postnatal psychiatric morbidity. Br J Psychiatry J Ment Sci 168(5): 607-611.
- Lambert GW, Reid C, Kaye DM, Jennings GL, Esler MD (2002) Effect of sunlight and season on serotonin turnover in the brain. Lancet Lond Engl 360(9348): 1840-1842.
- Lam RW, Levitt AJ, Levitan RD, Michalak EE, Cheung AH, et al. () Efficacy of Bright Light Treatment, Fluoxetine, and the Combination in Patients With Nonseasonal Major Depressive Disorder: A Randomized Clinical Trial. JAMA Psychiatry 73(1): 56-63.
- Perera S, Eisen R, Bhatt M, Bhatnagar N, de Souza R, et al. (2016) Light therapy for non-seasonal depression: systematic review and meta-analysis. BJPsych Open 2(2): 116-126.
- Kvam S, Kleppe CL, Nordhus IH, Hovland A (2016) Exercise as a treatment for depression: A meta-analysis. J Affect Disord 202: 67-86.
- Kim THM, Connolly JA, Tamim H (2014) The effect of social support around pregnancy on postpartum depression among Canadian teen mothers and adult mothers in the maternity experiences survey. BMC Pregnancy Childbirth 14: 162.
- Leahy-Warren P, McCarthy G, Corcoran P (2011) Postnatal depression in first-time mothers: prevalence and relationships between functional and structural social support at 6 and 12 weeks postpartum. Arch Psychiatr Nurs 25(3): 174-184.
- Lamb ME (2004) The Role of the Father in Child Development. John Wiley & Sons.
- Parke RD, Sawin DB (1976) The Father’s Role in Infancy: A Re-Evaluation. Fam Coord 25(4): 365-371.
- Feldman R (2003) Infant–mother and infant–father synchrony: The coregulation of positive arousal. Infant Ment Health J 24(1): 1-23.
- Grossmann K, Grossmann KE, Kindler H, Zimmermann P (2008) A wider view of attachment and exploration: The influence of mothers and fathers on the development of psychological security from infancy to young adulthood. In: Cassidy J, Shaver PR, eds. Handbook of Attachment: Theory, Research, and Clinical Applications. (2nd Edn), Guilford Press, Pp. 857-879.
- Cabrera N, Shannon J, C TL (2007) Fathers’ Influence on Their Children’s Cognitive and Emotional Development: From Toddlers to Pre-K. Applied Developmental Science 11(4): 208-213.
- Ruppenthal GC, Harlow MK, Eisele CD, Harlow HF, Suomi SJ (1974) Development of peer interactions of monkeys reared in a nuclear-family environment. Child Dev 45(3): 670-682.
- Sethna V, Perry E, Domoney J, Iles J, Psychogiou L, et al. (2017) FATHER-CHILD INTERACTIONS AT 3 MONTHS AND 24 MONTHS: CONTRIBUTIONS TO CHILDREN’S COGNITIVE DEVELOPMENT AT 24 MONTHS. Infant Ment Health J 38(3): 378-390.
- Abraham E, Hendler T, Shapira-Lichter I, Kanat-Maymon Y, Zagoory-Sharon O, et al. (2014) Father’s brain is sensitive to childcare experiences. Proc Natl Acad Sci U S A 111(27): 9792-9797.
- Shorey S, He HG, Morelius E (2016) Skin-to-skin contact by fathers and the impact on infant and paternal outcomes: an integrative review. Midwifery 40: 207-217.
- Riem MME, Lotz AM, Horstman LI, Cima M, Verhees MWFT, et al. (2021) A soft baby carrier intervention enhances amygdala responses to infant crying in fathers: A randomized controlled trial. Psychoneuroendocrinology 132: 105380.
- Kutlu A, Memik R, Mutlu M, Kutlu R, Arslan A (1992) Congenital dislocation of the hip and its relation to swaddling used in Turkey. J Pediatr Orthop 12(5): 598-602.
- Yamamuro T, Ishida K (1984) Recent advances in the prevention, early diagnosis, and treatment of congenital dislocation of the hip in Japan. Clin Orthop (184): 34-40.
- Büschelberger H (1976) Untersuchungen zur findung einer weitgehend physiologischen therapiemöglichkeit bei luxationshϋfte. In: Tagungsband Der 24 Tagung Der Gesellschaft Fϋr Klinische Medizin Der DDR Und Gesellschaft Fϋr Orthopädie Der DDR. VEB Kongreß- und Werbedruck Oberlungwitz, Magdeburg.
- Fettweis E (1991) Muscle-mechanical and biomechanical conditions of the squat-seat position in the treatment of infantile dislocation of the hip. Ortop Prax 8: 474-481.
- Harper P, Joseph BM, Clarke NMP, Herrera-Soto J, Sankar WN, et al. (2020) Even Experts Can Be Fooled: Reliability of Clinical Examination for Diagnosing Hip Dislocations in Newborns. J Pediatr Orthop 40(8): 408-412.
- Mulpuri K, Schaeffer EK, Andrade J, Sankar WN, Williams N, et al. (2016) What Risk Factors and Characteristics Are Associated with Late-presenting Dislocations of the Hip in Infants? Clin Orthop 474(5): 1131-1137.
- Engesaeter IØ, Lie SA, Lehmann TG, Furnes O, Vollset SE, et al. (2008) Neonatal hip instability and risk of total hip replacement in young adulthood: follow-up of 2,218,596 newborns from the Medical Birth Registry of Norway in the Norwegian Arthroplasty Register. Acta Orthop 79(3): 321-326.
- Castelein RM, Sauter AJM, de Vlieger M, van Linge B (1992) Natural History of Ultrasound Hip Abnormalities in Clinically Normal Newborns: J Pediatr Orthop 12(4): 423-427.
- Graham SM, Manara J, Chokotho L, Harrison WJ (2015) Back-carrying infants to prevent developmental hip dysplasia and its sequelae: is a new public health initiative needed? J Pediatr Orthop 35(1): 57-61.
- Sidharthan S, Kehoe C, Dodwell E (2020) Post-Natal Positioning through Babywearing: What the Orthopaedic Surgeon Needs to Know: J Pediatr Orthop Soc N Am 2(3). Accessed May 11, 2021.
- Couture DE, Crantford JC, Somasundaram A, Sanger C, Argenta AE, et al. (2013) Efficacy of passive helmet therapy for deformational plagiocephaly: report of 1050 cases. Neurosurg Focus 35(4): E4.
- Mawji A, Vollman AR, Hatfield J, McNeil DA, Sauvé R (2013) The Incidence of Positional Plagiocephaly: A Cohort Study. Pediatrics 132(2): 298-304.
- Ballardini E, Sisti M, Basaglia N, Benedetto M, Baldan A, et al. (2018) Prevalence and characteristics of positional plagiocephaly in healthy full-term infants at 8-12 weeks of life. Eur J Pediatr 177(10): 1547-1554.
- Aarnivala H, Vuollo V, Harila V, Heikkinen T, Pirttiniemi P, et al. (2015) Preventing deformational plagiocephaly through parent guidance: a randomized, controlled trial. Eur J Pediatr 174(9): 1197-1208.
- Kelly KM, Littlefield TR, Pomatto JK, Ripley CE, Beals SP, et al. (1999) Importance of early recognition and treatment of deformational plagiocephaly with orthotic cranioplasty. Cleft Palate-Craniofacial J Off Publ Am Cleft Palate-Craniofacial Assoc 36(2): 127-130.
- Robinson S, Proctor M (2009) Diagnosis and management of deformational plagiocephaly. J Neurosurg Pediatr 3(4):284-295.
- Flannery ABK, Looman WS, Kemper K (2012) Evidence-based care of the child with deformational plagiocephaly, part II: management. J Pediatr Health Care Off Publ Natl Assoc Pediatr Nurse Assoc Pract 26(5): 320-331.
- van Wijk RM, Pelsma M, Groothuis-Oudshoorn CGM, IJzerman MJ, van Vlimmeren LA, et al. (2014) Response to pediatric physical therapy in infants with positional preference and skull deformation. Phys Ther 94(9): 1262-1271.
- Siddicky SF, Bumpass DB, Krishnan A, Tackett SA, McCarthy RE, et al. (2020) Positioning and baby devices impact infant spinal muscle activity. J Biomech 104: 109741.
- Kennedy E, Majnemer A, Farmer JP, Barr RG, Platt RW (2009) Motor development of infants with positional plagiocephaly. Phys Occup Ther Pediatr 29(3): 222-235.
- International Labour Organization (2014) Maternity and Paternity at Work: Law and Practice across the World. International Labour Organization. Accessed August 4, 2020.
- Chzhen Y, Gromada A, Rees G (2019) Are the World’s Richest Countries Family Friendly? UNICEF Office of Research, Florence, Pp. 0-22.
- Guendelman S, Kosa JL, Pearl M, Graham S, Goodman J, et al. (2009) Juggling Work and Breastfeeding: Effects of Maternity Leave and Occupational Characteristics. Pediatrics 123(1): e38-e46.
- Ogbuanu C, Glover S, Probst J, Liu J, Hussey J (2011) The Effect of Maternity Leave Length and Time of Return to Work on Breastfeeding. Pediatrics 127(6): e1414-e1427.
- Plotka R, Busch-Rossnagel NA (2018) The role of length of maternity leave in supporting mother–child interactions and attachment security among American mothers and their infants. Int J Child Care Educ Policy 12(1): 2.
- Kornfeind KR, Sipsma HL (2018) Exploring the Link between Maternity Leave and Postpartum Depression. Womens Health Issues 28(4): 321-326.
- Parenting in the Workplace Institute (2020) Parenting in the Workplace Institute. piwi. Published 2020. Accessed August 4, 2020.
- Baby Carriers, Seats, & Other Equipment (2016) International Hip Dysplasia Institute. Accessed December 19, 2016.
- Murray L (2014) The Psychology of Babies: How Relationships Support Development from Birth to Two. Robinson.
- Pollitzer P, Little B (2014) Proposed Rule: Safety Standard for Sling Carriers. Published online 2014. Accessed November 17, 2020.
- Frisbee S, Hennes H (2000) Adult-worn child carriers: a potential risk for injury. Inj Prev 6(1): 56-58.
- Ferres JML, Anderson TM, Johnston R, Ramirez JM, Mitchell EA (2020) Distinct Populations of Sudden Unexpected Infant Death Based on Age. Pediatrics 145(1): e20191637.
- Bergounioux J, Madre C, Crucis-Armengaud A, E Briand-Huchet, A P Michard-Lenoir, et al. (2015) Sudden deaths in adult-worn baby carriers: 19 cases. Eur J Pediatr 174(12): 1665-1670.
- Baby Carrier Industry Alliance (2021) Resources & References. Baby Carrier Industry Alliance. Published 2021. Accessed March 9, 2021.
- Center for Babywearing Studies (2019) Center for Babywearing Studies. Center for Babywearing Studies. Published 2021. Accessed December 16, 2019.






























