Hypocalcaemia in Asphyxiated Newborns: Prevalence and Relationship to Severity of Birth Asphyxia in Babies Admitted to A Tertiary Facility in South-Western Nigeria
Ugowe OJ1*, Adejuyigbe EA1,3 and Anyabolu CH2,3
1Neonatal Unit, Department of Paediatrics, Obafemi Awolowo University Teaching Hospitals Complex, Ile-Ife, Nigeria
2Paediatric Gastroenterology Unit, Department of Paediatrics, Obafemi Awolowo University Teaching Hospitals Complex, Ile-Ife, Nigeria
3Department of Paediatrics and Child Health, Obafemi Awolowo University, Ile-Ife, Nigeria
Submission: March 11, 2022; Published: June 01, 2022
*Corresponding author:Dr Ugowe Osagie, Neonatal Unit, Department of Paediatrics, Obafemi Awolowo University Teaching Hospitals Complex, Ile-Ife, Nigeria, Tel: +234 7066279676
How to cite this article:Ugowe O, Adejuyigbe E, Anyabolu C. Hypocalcaemia in Asphyxiated Newborns: Prevalence and Relationship to Severity of Birth Asphyxia in Babies Admitted to A Tertiary Facility in South-Western Nigeria. Acad J Ped Neonatol 2022; 11(4): 555875. 10.19080/AJPN.2022.11.555875
Abstract
Background: Birth asphyxia and hypocalcaemia can both cause significant morbidity and mortality. In spite of this, the prevalence of hypocalcaemia among newborns with birth asphyxia as well as its relationship to asphyxia severity has not been well researched in Nigeria. This study set out to determine the prevalence of hypocalcaemia in term neonates with birth asphyxia and the relationship between levels of calcium and the severity of birth asphyxia.
Methods: In this cross-sectional analytical study, the serum calcium levels of consecutive cases of birth asphyxia were compared with that of gestational age and sex-matched healthy babies seen at the Ife Hospital Unit of OAUTH. Babies with APGAR scores less than 7 in the fifth minute of life were recruited into the study. Blood samples were taken from each baby at birth. Serum total and ionised calcium were measured using an ion selective electrode method while serum albumin was measured using spectrophotometer.
Results: Of the 102 asphyxiated neonates, 44 (43.1%) compared with 16 (15.7%) of the control neonates had low serum total calcium (χ2=19.317, p=0.001) with an OR of 4.1 (95% CI 2.1,7.9). The proportion of babies with hypocalcaemia increased with severity of birth asphyxia (LR=10.341; p=0.035). The median (IQR) levels of serum total calcium were 2.2 (1.8-2.3) mmol/L, 1.9 (1.8-2.3) mmol/L and 1.9 (1.7-2.4) mmol/L in babies with mild, moderate and severe birth asphyxia respectively (H=.7.184; p =0.028).
Conclusion: This study has shown that hypocalcaemia is more common in babies with birth asphyxia and that hypocalcaemia worsened with increasing severity of asphyxia.
Keywords: Calcium levels, perinatal asphyxia, encephalopathy, severity of asphyxia
Abbreviations: OAUTHC: Obafemi Awolowo University Teaching Hospitals Complex, IHU: Ife Hospital Unit, APGAR: Appearance, Pulse, Grimace, Activity and Respiration
Introduction
The proportion of childhood deaths occurring in the neonatal period is increasing. Globally, an estimated four million babies die in the first four weeks of life annually and three-quarters of these deaths occur in the first week of life [1]. About 99% of neonatal deaths occur in low and middle-income countries including Nigeria. The gains made in reducing under-five mortality in Nigeria have not been matched by a significant reduction in deaths among neonates. According to the Nigeria Demographic and Health Survey reports of 2018, neonatal mortality rate was 39 per 1000 live births, constituting 58 percent of infant mortality [2]. This is slightly higher than a mortality rate of 37 per 1000 live births published in 2013. The main causes of neonatal death are birth asphyxia, preterm births and severe infections [1].
Birth asphyxia is a major cause of concern for health practitioners in Nigeria. It is defined as the failure to initiate and sustain spontaneous respiration within the first minute of life with consequent acidosis and hypoxic ischaemic injury to the tissues [3]. The prevalence of birth asphyxia in a study at the Wesley Guild Hospital, Ilesha, Osun State was 100.2 per 1000 neonatal admissions. This showed a significant contribution of birth asphyxia to neonatal morbidity in Ilesha, Osun State [4] Onyiriuka [5] found the incidence of birth asphyxia to be 83.8 per 1000 live births in a mission hospital in Benin City. The complications of birth asphyxia are pan-systemic and may result in permanent neurological damage and death [3]. Metabolic complications such as hypocalcaemia, hypomagnesaemia and hypoglycaemia may also be associated with birth asphyxia [6].
Calcium functions as support mineral in bones, act as second messengers in cellular signaling pathways and play vital roles in muscle contraction and relaxation. Calcium is very important in biochemical processes in the body and it is the most abundant mineral in the body; 99% is present in bone and less than one percent is found in the extracellular space [7]. Of the total serum calcium, 40% is protein bound, 10% exist in complexes with anions, such as citrate, phosphate, bicarbonate and lactate and 50% is the free or ionized physiologically active form. There are physiological reductions in the blood levels of calcium within the first few hours of life due to loss of placental supply after delivery. Calcium level is controlled by three major hormones; parathyroid hormone, calcitonin and 1,25 dihydroxycholecalciferol. A decrease in calcium levels in the blood after birth stimulates parathyroid hormone release. The levels of parathyroid hormone rise gradually to near adult values by 24-48 hours. Parathyroid hormone maintains normal calcium levels by stimulating bone resorption, increasing calcium reabsorption from renal tubules and promoting renal production of 1,25 dihydroxycholecalciferol which in turn increases intestinal absorption of calcium and phosphate [8].
Hypocalcaemia in term babies refers to serum calcium concentration below 2mmol/L [7,9]. Birth asphyxia is a common cause of neonatal hypocalcaemia [3,7]. Other causes include prematurity and intrauterine growth restriction, congenital defects like Di-George syndrome, vitamin D deficiency and consumption of formula feeds that are high in phosphate [7]. Poorly controlled maternal diabetes mellitus is also a risk factor for hypocalcaemia in the newborn [3,7]. Within 48 hours of delivery, their levels return to normal through homeostasis. This physiological reduction in serum levels of calcium after delivery is also worsened by birth asphyxia [10]. Lower levels of serum calcium in babies with asphyxia may be due to decreased calcium intake due to delayed feeding, [7]. renal insufficiency and increased serum calcitonin concentration [9,10]. Other factors include decreased parathyroid hormone and increased endogenous phosphate load [7,9,10]. A decreased phosphate excretion from low parathyroid hormone levels may lead to an increased endogenous phosphate load [7,10].
This study is relevant to the practice of Paediatrics especially in Nigeria where the burden of perinatal asphyxia is quite significant.[4,5]. Hypocalcaemia and birth asphyxia are both documented to be common in our environment but the relationship between hypocalcaemia, and severity of birth asphyxia has not been well researched in Nigeria. In a hospital-based study in Benin, Onyiriuka [11]. found the prevalence of hypocalcaemia among babies with severe birth asphyxia to be 22.6% while Kayode et al. [12]. reported a prevalence of 28.4% among all babies with birth asphyxia. Also, early onset hypocalcaemia among healthy and sick babies in Port Harcourt was 16.1% as reported by Anolue et al. [13]. More studies need to be carried out to provide information on the burden of hypocalcaemia in asphyxiated babies especially those with mild, moderate and severe asphyxia. This study was designed to determine the prevalence of hypocalcaemia in term neonates with birth asphyxia and the relationship between levels of calcium and the severity of asphyxia and encephalopath.
Study Methods
The study was carried out from 30th November 2018 to April 30th 2019 and it was cross-sectional analytical study that involved the comparison of asphyxiated babies (cases) with nonasphyxiated ones (controls). The location was at the neonatal and labour wards of the Ife Hospital Unit of the Obafemi Awolowo University Teaching Hospitals Complex (OAUTHC), Ile-Ife. The hospital serves as tertiary referral center for both urban and rural communities of Osun, Ondo and Ekiti States in the southwestern part of Nigeria. All the study subjects and controls were recruited from the Ife Hospital Unit (IHU) of Obafemi Awolowo University Teaching Hospital Complex (OAUTHC). Subjects were consecutive full-term neonates with birth asphyxia.
Birth asphyxia was defined by fifth minute APGAR scores below 7. Cases were term babies who were born in the hospital with APGAR scores less than 7 at the 5th minute of life while the controls selected were term neonates without birth asphyxia (APGAR scores 7 or more in the 5th minute. Mild asphyxia was defined as APGAR score of 6. Moderate and severe birth asphyxia were defined by APGAR scores 4-5 and APGAR scores 0-3 respectively [14]. Cases were classified into mild, moderate and severe encephalopathy using the Sarnat and Sarnat staging system [15]. for those that had features of hypoxic encephalopathy [15]. The neonates that met the inclusion criteria were recruited consecutively until the desired sample size in both arms of the study was attained. Babies born to mothers with diabetes mellitus, low birth weight (birth weight less than 2.5kg) and infants with congenital defects like Di-George syndrome were all excluded because LBW and infants of diabetic mothers are both predisposed to hypocalcaemia while hypocalcaemia is a feature of Di George syndrome [16,17]. Also, babies who received exchange blood transfusions were excluded because hypocalcaemia can result from chelation of ionised calcium by citrate in anticoagulated blood [16]. Ethical approval was obtained from the OAUTHC Research and Ethics Committee. Written consent was obtained from mothers or care givers after explaining to them that babies found to have low serum calcium will be given appropriate therapy after providing information about the study.
A research proforma was used to record the biodata of the study subjects (cases) and controls. The data included age and sex, gestational age at delivery (calculated from last menstrual period or early ultrasound scan done in the first or early second trimester for mothers unsure of date), birth weight, length and head circumference. Apgar scoring was done at birth by the researcher or his assistants. The researcher and assistants had undergone comprehensive neonatal resuscitation training and were also taking calls in the neonatal unit as part of routine call duty. Neonates who had low APGAR scores in the first minute of life were resuscitated according to standard unit protocol. Babies with APGAR scores less than 7 in the fifth minute of life were then recruited into the study and blood samples collected immediately.
Study Procedure
All babies were examined (both general and systemic examination) after resuscitation for the level of consciousness, muscle tone, reflexes, presence or absence of convulsion and the stage of encephalopathy using the Sarnat and Sarnat staging [15]. for all those who had clinical features of encephalopathy. EEG was not available for the study therefore no EEG findings were used to stage encephalopathy. Subsequently, patients with birth asphyxia were examined at least twice a day (at 12hours and at 24hours of life) for abnormal clinical signs or signs of encephalopathy which were documented. This examination was done till discharge or death. Maternal demographic characteristics like marital status, social class and educational level, parity, booking status, antenatal visits, place of delivery, duration of labour and mode of delivery.
Recruitment of the study subjects and controls was done by the researcher and two junior resident doctors who served as assistants. The research assistants were trained by the researcher and the procedure of assessing APGAR scores for newborns was standardized to minimize inter-observer variability. Standard setting was also done for other study protocols, such as obtaining consent, filling the proforma and obtaining blood samples correctly for the two arms of the study. The standardization exercises were reviewed and repeated at two-weekly intervals for quality assurance. All the babies recruited by the assistants were reassessed for confirmation by the researcher.
About 3mls of venous blood was collected from each of the study participants using a 23G needle into plain bottles for determining serum concentrations of total and ionized calcium, total albumin. To avoid venous stasis, blood samples were collected from peripheral veins without applying a tourniquet. The skin over the peripheral vein area was swabbed with methylated spirit before collection of blood samples. The blood samples were allowed to clot. Thereafter they were centrifuged at 3000 revolutions per minute for 10 minutes. The supernatant serum was pipetted into another plain bottle and sent for analysis. Serum total and ionized calcium concentrations were determined immediately when the samples got to the laboratory. After analysis of serum calcium, remnant serum samples were stored at -20 °C for analysis of serum albumin concentrations which were done in batches.
Serum total and ionised calcium were analysed using ion selective electrode technique [18]. with results available immediately while serum albumin was analysed in batches using spectrophotometry [19]. Serum samples were analysed at the Chemical Pathology Research Laboratory of the OAUTHC, Ile-Ife. Other investigations like packed cell volume (PCV) and random blood sugar (RBS) were carried out as part of the neonatal unit protocol. The normal range of total calcium and ionized calcium used for this study was 2.0-2.65mmol/L and 1.1-1.5mmol/L respectively. The reference range for albumin was 35.0-54.0g/L. Babies with low levels of calcium (less than 2mmol/L or ionised calcium less than 1.1mmol/L) were treated with bolus doses of intravenous calcium gluconate at a dose of 1ml/kg over 15 minutes [7]. The cost of analysing the samples and of treatment for babies with hypocalcaemia was borne by the researcher.
Median and interquartile range were determined for continuous variables such as weight, serum total and ionized calcium levels of study participants and median values of continuous variables were compared using non-parametric tests such as Mann-Whitney U and Kruskal-Wallis tests. Total serum calcium concentrations were grouped into normal (2.0-2.65mmol/L), hypocalcaemia (< 2mmol/L) and hypercalcaemia (>2.65mmol/L). while ionised calcium was grouped into normal (1.1-1.5mmol/L), hypocalcaemia (<1.1mmol/L) and hypercalcaemia (>1.5mmol/L) [7]. for subjects and for controls. The total serum calcium levels were corrected for albumin before entering the data as total calcium. Serum albumin was grouped into normal albumin (35- 54g/L) and hypoalbuminaemia (<35g/L). Birth asphyxia was grouped according to severity as mild (APGAR score 6), moderate (APGAR score 4-5) and severe (APGAR score 0-3) [14].
Results
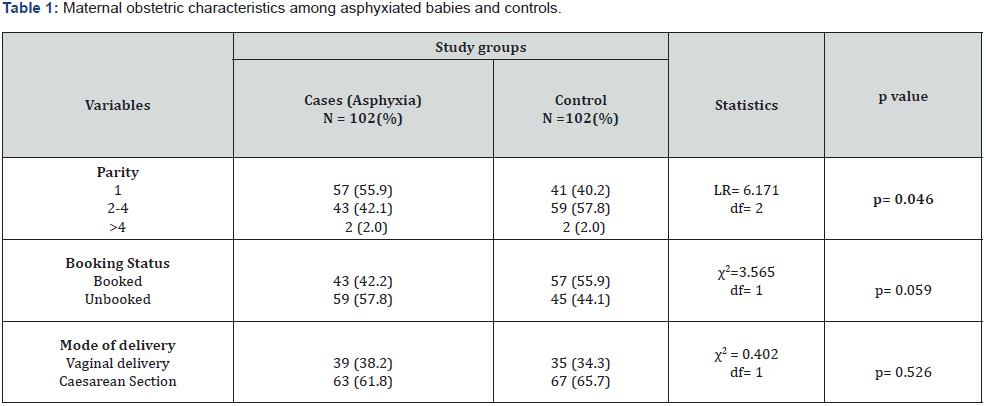
Among the 204 neonates recruited, 102 neonates were in the case group while 102 neonates were in the control group. There were 56 (54.9%) males and 46 (45.1%) females in the case group. Similarly, there were 52 (51.0%) males and 50 (49.0%) females in the control group (χ2 = 0.131, df =1, p = 0.717). The M:F ratio for this study was 1.1:1. Out of the 102 subjects with birth asphyxia, 39 (38.2%) were in the mild asphyxia group while the number of babies in the moderate and severe group were 49 (48.0%) and 14 (13.7%) respectively. Maternal characteristics are shown in Table 1.
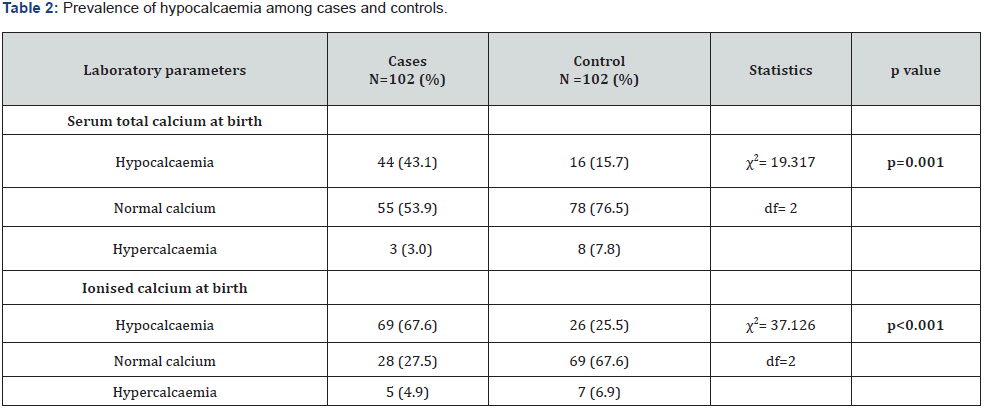
The range of total serum calcium at birth for the cases was 1.1-2.7mmol/L with a median (IQR) of 2.0 (1.7-2.2) mmol/L while in the control the range was 1.7-3.0mmol/L with a median (IQR) of 2.3 (2.1-2.5) mmol/L. The difference in the median of the total serum calcium in the subjects and controls was statistically significant (U=2858.0; p=0.001). Serum ionised calcium for cases ranged from 0.5-2.4mmol/L with a median (IQR) of 1.0 (0.8-1.1) mmol/L while the range and median levels were 0.8-2.0mmol/L and 1.2 (1.1-1.4) mmol/L respectively in the control group. The difference was statistically significant (U=2724.0; p value=0.001). Table 2 shows the prevalence of hypocalcaemia among babies with birth asphyxia was more than twice that of healthy babies.
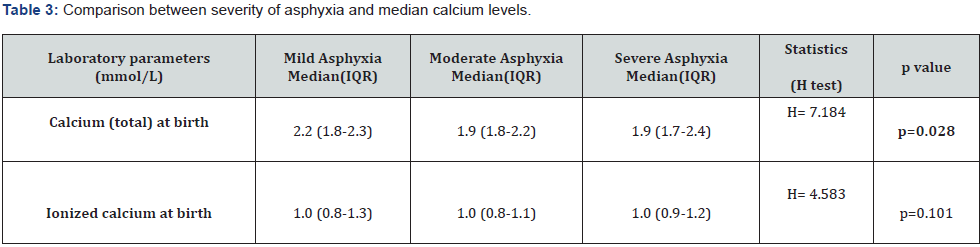
The comparison between the severity of birth asphyxia and median calcium level is shown in Table 3. The median total calcium levels of babies with mild, moderate and severe birth asphyxia were 2.2 (1.8-2.3) mmol/L, 1.9 (1.8-2.2) mmol/L and 1.9 (1.7-2.4) mmol/L respectively. This difference in serum calcium levels was found to be statistically significant (H= 7.184; p value =0.028). Also, the results showed that 10 (25.6%) of the babies with mild birth asphyxia had low total calcium, while hypocalcaemia was found in 25 (51.0%) and 9 (64.3%) of the babies with moderate and severe asphyxia respectively. The proportion of babies with hypocalcaemia increased with severity of birth asphyxia. This relationship was statistically significant (LR = 10.341; p = 0.035).
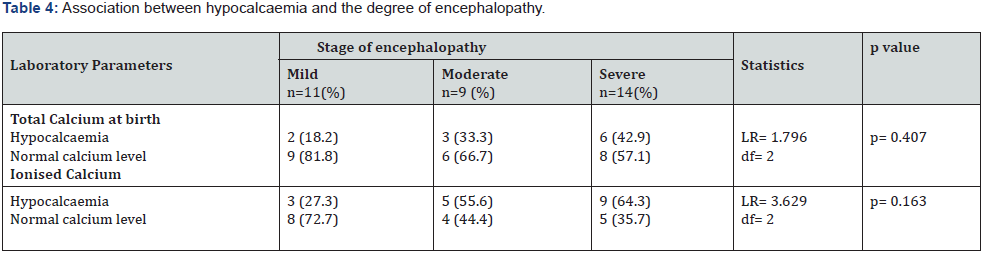
A total of 34 out of the 102 cases of birth asphyxia had features of encephalopathy. Eleven (32.4%) of the 34 cases with encephalopathy compared to 33(48.5%) of the 68 cases without encephalopathy had hypocalcaemia. The difference was not statistically significant (χ2= 2.418; p=0.06). Table 4 below shows that the proportion of babies with hypocalcaemia increased with increasing severity of encephalopathy although this was not statistically significant.
Discussion
This study confirms that hypocalcaemia was more common among neonates with birth asphyxia compared to healthy babies. The proportion of babies with hypocalcaemia also increased with the severity of birth asphyxia. The prevalence of hypocalcaemia among subjects with birth asphyxia was 43.1%, which is higher than the prevalence of 22.6% and 28.4% found by Onyiriuka [11] and Kayode et al. [12] in Benin and Osogbo (both in Nigeria) respectively. This study also showed a higher prevalence of hypocalcaemia among controls (15.7%) compared to 7.9%, 4.9% and 1.4% found by Onyiriuka [11] Kayode et al. [12] and Nayirat [20] respectively. The higher cut-off value for hypocalcaemia (total calcium <2mmol/L) used in the present study could explain the higher prevalence than what was found by Onyiriuka [11] where cut-off for hypocalcaemia was <1.75mmol/L which was also lower than other reported studies [20-22].
Furthermore, differences in laboratory methods may account for the higher prevalence of hypocalcaemia found in the present study. Total and ionised calcium were measured using electrode analyser in this study compared to the Onyiriuka [11] and Kayode et al. [12] study where spectrophotometry was used to determine calcium levels. The use of spectrophotometry to measure total calcium (and the subsequent correction for albumin) has been found to underestimate hypocalcaemia especially with albumin levels lower than 30g/L [18]. The timing of blood sample collection in the current study may also account for the higher prevalence of hypocalcaemia. In the present study, the first batch of samples was taken at birth compared to the Nayirat [20]. study where samples were taken at any time within the first 48 hours. Blood samples taken at birth, a time when calcium levels are expectedly lower due to separation of the foetus from the placenta [7,16]. may explain the higher prevalence of hypocalcaemia compared to the Nayirat study [20]
This study interestingly showed that hypercalcaemia can exist among babies with birth asphyxia even though the prevalence was very low (3.0%). This was not iatrogenic as no subject had calcium infusion before samples were taken. Neonatal hypercalcaemia is a rare condition with an unclear pathogenesis. It may be asymptomatic or associated with anorexia, poor feeding and hypotonia. Hypercalcaemia may lead to nephrocalcinosis, hypercalciuria and central nervous system damage [23-25]. Causes of neonatal hypercalcaemia include William syndrome, hyperparathyroidism, familial hypercalcaemia and subcutaneous fat necrosis [23-25]. Subcutaneous fat necrosis can occur among birth asphyxiated babies and it is commonly associated with hypercalcaemia although hypocalcaemia can occur as well [26]. There was no case of subcutaneous fat necrosis among the cases of birth asphyxia in the present study. Monitoring of calcium levels is therefore important while correcting hypocalcaemia so as not to tilt babies into hypercalcaemia.
Furthermore, there was a relationship between the degree of birth asphyxia and levels of total calcium. The median total calcium level was lower in babies with severe birth asphyxia compared to those with mild birth asphyxia. This pattern was reported by Rai et al. [27] as mean serum calcium for babies with mild, moderate and severe asphyxia were 2.12mmol/L, 2.05mmol/L and 1.99mmol/L respectively, showing a negative correlation of mean calcium levels to severity of asphyxia [27]. However, there were limitations in comparing the findings of this work to other studies to highlight how the degree of birth asphyxia affects calcium levels because most studies only compared calcium levels of babies with birth asphyxia to healthy babies and did not examine the relationship between the degree of birth asphyxia and serum calcium levels.
The findings from this study also did not demonstrate a significant relationship between calcium levels and encephalopathy as was reported by Thakur et al. [28] and Zaman et al. [29]. Though there is no reported direct relationship between hypocalcaemia and development of hypoxic encephalopathy, hypocalcaemia is a known aetiology of neonatal convulsions and seizures are a key feature of encephalopathy [15].
Conclusion
This study has shown that hypocalcaemia is common in asphyxiated babies born in OAUTHC Ile-Ife. More importantly, low levels of calcium can be found in all degrees of asphyxia and encephalopathy. The proportion of babies with hypocalcaemia increased with worsening asphyxia but there was no clear relationship between calcium levels and encephalopathy. The fact that hypercalcaemia was recorded is instructive because while managing other complications of birth asphyxia, monitoring of calcium levels is valuable as it helps in detecting both reduced and possibly elevated values.
References
- Lawn JE, Blencowe H, Oza S, You D, Lee AC, et al (2014) Every Newborn: progress, priorities and potential beyond survival. Lancet 384 (9938): 189-205.
- National Population Commission (NPC) (Nigeria) and ICF (2019) Nigeria Demographic and Health Survey 2018. Abuja, Nigeria and Rockville, Maryland, USA, NPC and ICF.
- Lisa M, Lu-Ann P (2008) Perinatal Asphyxia In: Cloherty, John P, Eichenwald EC, Stark AR (eds) Manual of Neonatal Care. (6th Edn) Lippincott Williams & Wilkins, USA, 27C: 519-28.
- Ogunlesi T, Oseni SB (2008) Severe Birth Asphyxia in Wesley Guild Hospital, Ilesa: A persistent plague! Niger Med Pract 53: 40-43.
- Onyiriuka A (2009) Birth asphyxia in a Nigerian mission hospital in Benin city. Trop J Obstet Gynaecol 26: 80-88.
- Ira A, Barbara J (2007) Hypoxia- Ischaemia In: Robert M, Richard E, Hal B(eds) Nelson Textbook of Pediatrics (18th Edn) WB Saunders, Philadelphia, USA 99.5: 718.
- Michael R, Robert M (2013) Glucose, Calcium and Magnesium In: Avroy A, Jonathan M(Eds) Klaus & Fanaroff's Care of the High-Risk Neonate. (6th Edn) Elsevier Saunders 12: 299-305.
- Mundy GR, Guise TA (1999) Hormonal Control of Calcium homeostasis. Clin Chem 45(8): 1347-1352.
- Jain A, Agarwal R, Sankar MJ, Deorari A, Paul VK (2010) Hypocalcemia in the newborn. Indian J Pediatr 77(10): 1123-1128.
- Welime KJ (2011) A study of the prevalence and correlates of early onset neonatal hypocalcaemia in term neonates at Kenyatta national hospital (Unpublished): University of Nairobi.
- Onyiriuka AN (2011) Early-Onset Neonatal Hypocalcaemia Among Full-Term Infants with Severe Birth Asphyxia. Pac J Med Sci 8(1): 4-11.
- Kayode OV, Adebami OJ, Oyedeji OA, Oninla SO, Oseni SBA, et al. (2021) Abnormal biochemical parameters among term neonates with perinatal asphyxia and their non-asphyxiated controls in Osogbo. Res J of Health Sci 9(3): 308-319.
- Anolue MA, Tamunopriye J, Opara PI (2019) Early Onset Hypocalcaemiain Babies Delivered at the University of Port-Harcourt Teaching Hospital, Port-Harcourt, Nigeria. J Pediatr Noenatal Biol (1): 101.
- Olowu JA, Azubuike JC (1999) Assessment and Care of the Newborn Infant In: Azubuike, Nkangineme (Editors) Paediatrics and Child Health in a Tropical Region. African Educational Series 38-43.
- Sarnat HB, Sarnat MS (1976) Neonatal encephalopathy following fetal distress: a clinical and electroencephalographic study. Arch Neurol 33(10): 696-705.
- Rennie J, Kendall G (2002) Metabolic Disorders In: Rennie J(Ed). A Manual of Neonatal Intensive Care (5th Edn) Hodder Arnold 689-694.
- Thilo E, Rosenberg A (2011) The newborn infant In: Hay WW Jnr, Levin MH, Deterding RR (eds). Current Diagnosis and Treatment in Pediatrics (20th Edn) McGraw Hill, New York, USA, Pp. 1-63.
- Robertson WG, Marshall RW (1979) Calcium measurements in serum and plasma- Total and Ionized. CRC Crit Rev Clin Lab Sci 11(3): 271-304.
- Robertson WS (1981). Optimizing determination of plasma albumin by the bromocresol green dye-binding method. Clin Chem 27(1): 144-146.
- Nayirat M (2016) Prevalence of Hypocalcemia in Term Neonates with Moderate and Severe Perinatal Asphyxia in Kenyatta National Hospital. University of Nairobi Research Archive Pp.15-19.
- IIves P, Kiisk M, Soopold T, Talvik T (2000) Serum total magnesium and ionized calcium concentrations in asphyxiated term newborn infants with hypoxic-ischaemic encephalopathy. Acta Paediatrica 89(6): 680-685.
- Saha D, Ali M, Haque M, Ahmed M (2015) Association of hypoglycemia, hypocalcemia and hypomagnesemia in neonates with perinatal asphyxia. Mymensigh Med J 24(2): 244-250.
- Ghirri P, Bottone U, Coccoli L, Bernadini M, Vuerich M, et al. (1999) Symptomatic hypercalcemia in the first months of life: calcium-regulating hormones and treatment. J Endocrinol Invest 22(5): 345-353.
- Chrysaidou K, Sargiotis G, Karava V, Liasis D, Gourvas V, et al. (2021) Subcutaneous Fat Necrosis and Hypercalcemia with Nephrocalcinosis in Infancy: Case Report and Review of the Literature. Children 8(5): 374.
- Gorvin CM (2021) Genetic causes of neonatal and infantile hypercalcaemia. Pediatr Nephrol 37(2): 289-301.
- Onyiriuka AN, Utomi TE (2017) Hypocalcemia Associated with Subcutaneous Fat Necrosis of the Newborn: Case Report and Literature Review. Oman Med J 32(6): 518-521.
- Rai S, Bhatiyani KK, Kaur S (2015) Effect of Birth Asphyxia on Serum Calcium and Glucose level: A Prospective Study Int J Sci Stud 3(7): 3-6.
- Thakur J, Bhatta NK, Singh RR, Poudel P, Lamsal M, et al. (2018) A Prevalence of electrolyte disturbances in birth asphyxia: A prospective study. Ital J Pediatr 44(1): 56.
- Zaman R, Mollah AH, Chowdhury MMR, Yeasmin S, Chowdhury AS, et al. (2017) Serum Magnesium and Calcium Status among Term Asphyxiated Newborns with Moderate to Severe Hypoxic-Ischemic Encephalopathy (HIE). J Dhaka Med Coll 26(2): 148-152.






























