Impact of Training Health Care Workers in Resuscitation on Asphyxia Related Deaths
Chandrakala BS1, Sudhindrashayana Fattepur2, Chaitali R Raghoji3, Kotturesha Rasthapurmath4 and Manisha Bhandankar5*
1Professor, Neonatology, St John’s Medical College, Bangalore - 560034 Karnataka
2Fellowship in Neonatology, Associate Professor of Pediatrics, KIMS, Hubli 580021 Karnataka
3Fellowship in Perinatal medicine, Senior resident, Department of Neonatology, Bapuji child health Institute, JJM Medical college, Davangere- 577004 Karnataka
4Consultant Neonatologist and Paediatrician, Kottureshwara Hospital, Shimoga, 577201, Karnataka
5Professor, JNMC, Belgaum, Karnataka
Submission: January 28, 2022; Published: May 11, 2022
*Corresponding author:Manisha Bhandankar, MD, PhD, MRCPCH, Professor, JNMC, Belgaum, Karnataka
How to cite this article:chandrakala BS, Sudhindrashayana F, Chaitali R R, Kotturesha R, Manisha B. Impact of Training Health Care Workers in Resuscitation on Asphyxia Related Deaths. Acad J Ped Neonatol 2022; 11(4): 555873. 10.19080/AJPN.2022.11.555873
Abstract
Introduction: Training and improvement in the quality of neonatal resuscitation (NR) programme is crucial to reduce early neonatal deaths secondary to birth asphyxia in the developing world.
Methodology: This was an interventional study, conducted in 8 high priority districts of Karnataka during the period 2018-2019. Primary Objective was to study the impact of training health care workers (HCW) in neonatal resuscitation, on the deaths related to asphyxia. Secondary objective was to compare the pretest knowledge and skills of the participants, with the post-test, after the training. A Total of 226 HCWs were trained by doctors certified as trainers. There were 88.9% female HCWS and 88% of them were nurses. The percentage of reduction of mortality in above mentioned districts after the training, was 27.4% from April 2017-Mar 2018 and 21% from April 2018 to March 2019 with P=<0.01. From April 2017 to Dec 2019 (2 year, 8 months). The total reduction was 57%, which was statistically significant over time (p<0.001). The score for Comparison of knowledge and skill scores before and after the training was 15.8 ± 3.26 Vs 18.4 ± 2.11(P value-<0.0001) out of 20 and 58.9 ± 28 Vs 188.8 ± 6.68 scores out of 100 (P value <0.0001) respectively.
Conclusion: Structured training of HCW in Neonatal Resuscitation reduces the birth asphyxia related mortality in high priority districts. Structured training also improves the knowledge and skills immediately after the training.
Keywords: Health care workers; training; resuscitation; knowledge and skills
Abbreviations: LMICs: Low and Middle-Income Countries, HPD: High Priority Districts, IAP: Indian Academy of Paediatrics, MOU: Memorandum of Understanding, IAP-NRP-FGM: Indian Academy of Pediatrics- Neonatal Resuscitation Programme- First Golden Minute Project, HMIS: Health Management Information System, NMR: Neonatal Mortality Rate, MDG-4: Millennium Development Goal-4, NR: Neonatal Resuscitation, SFNRT: Standardised Formal Neonatal Resuscitation Training, CHW: Community Health Workers
Introduction
Almost all deaths (97.8%) due to asphyxia occur in the first week of life, with 70% of them occurring within the first 24hours [1]. A systematic analysis of global, regional, and national causes of child mortality identified, preterm birth and its complications, infections are the two major causes of neonatal deaths in India, other cause being perinatal asphyxia and malformations [2]. Perinatal asphyxia is one of the major contributors of neonatal mortality in developing countries [3]. Problems at delivery can result in perinatal asphyxia if appropriate resuscitation help is not available [4]. Facilities where births occur should ensure that all birth attendants are trained and competent in Neonatal resuscitation. It is estimated that universal training on basic resuscitation may save hundreds of thousands of newborn lives currently lost each year, and hence contributes significantly to progress toward Millennium Development Goal 4 [5]. Inadequate skills in resuscitation among health-care providers, is a major challenge to the delivery of high-quality health care in low and middle-income countries (LMICs) [6].
The high priority districts (HPD) are those in the bottom 25% of the districts in every state according to their ranking based on the composite health index. The high priority districts of Karnataka, which were selected for this project caters with nearly 15000 deliveries every year, thus adding to major burden of mortality and morbidity due to perinatal asphyxia. Current health infrastructure in Karnataka: Mothers with antenatal highrisk factors or intrapartum complications are being referred from the primary health centers or community health centers to the tertiary care hospital which may be either Medical Colleges or District/General Hospitals. Thus, the district hospitals have a high load of highrisk deliveries which leads to neonates requiring resuscitation at birth. The special newborn care unit of each of these district hospitals has a team of a Pediatrician, 3 Medical officers, and 12 staff nurses for every 12 bedded unit who are responsible for attending the delivery, caesarian section and provide newborn care including neonatal resuscitation when required. Although the HCWS (Medical Officers and staff nurses) are trained in basic neonatal care at the time of induction into the facility, the retention of skills and knowledge in resuscitation including the quality of care provided, does not get monitored, due to the high workload. 24/7 availability of a pediatrician is also restricted in these units. These are HCWS in SNCUs, who refer sick neonates to nearby tertiary hospitals. Hence, the nurses who attend delivery are not confident of resuscitation, which leads to inadequate and ineffective resuscitation leading to birth asphyxia. The nurses in SNCU did not have an official training certificate. Hence, this project was carried out to train the HCW, who attends delivery at SNCUs of the HPD in basic newborn resuscitation. If the training was found to be effective, in reducing the mortality, it was planned to extend this training project to other districts of Karnataka and to other states of the country.
Materials and Methods
The Primary Objective: To study the impact of training HCW in neonatal resuscitation on deaths related to birth asphyxia.
The Secondary objective: To compare the pre-test knowledge and skills of the participants with the post-test values immediately after the training.
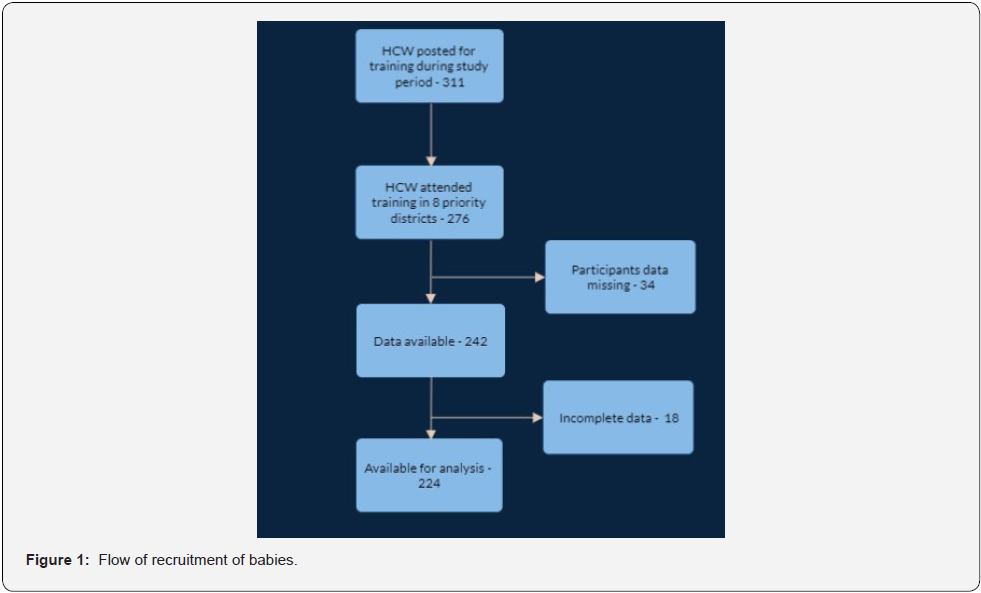
This interventional study was conducted in 8 HPD’s of Karnataka, which were Bidar, Chamarajanagar, Chitrdurga, Gadag, Haveri, Koppal, Yadgir and Tumkur. The Data was available for 226 participants and hence was analysed. The flow of the data analysis is shown in (Figure -1). The Academic coordinators for the state from Indian Academy of Paediatrics (IAP) had a Memorandum of understanding (MOU) with the Deputy director (DD), Health and family welfare department, government of Karnataka. The participants from each district were deputed by the Government. The training method of the participants across all districts was conducted as per the norms of IAP-NRP-FGM project (Indian Academy of Pediatrics- Neonatal Resuscitation programme- First Golden Minute project). The three state coordinators for basic NRP for Karnataka organised the overall logistics at each workshop.
The workshop included the demonstration of skills playing videos and hands-on training of all participants. The ratio of participants to faculty was 8:1. The duration of training was 9 hours. The written test had 20 questions on knowledge assessment on resuscitation followed by structured performance evaluation of the skills by all the participants. There was uniformity of the assessment of their performance as per the checklist. Verbal and written feedback was taken from the participants on the workshop and logistics. A score of more han 85% in both knowledge and skills was required to receive the certificate from Indian Academy of Paediatrics (IAP). Ethical committee clearance from Health and Family welfare, Government of Karnataka, was taken before the manuscript was submitted for publication. The diagnosis of perinatal asphyxia was considered based on any one of the following - delayed cry, need of assisted ventilation at birth, OR APGAR score of <3 at 1 minute or < 5 at 5 min defined as per the FBNC guidelines from Government of India (GOI) (7). Moderate to severe perinatal asphyxia/HIE was identified in a baby with birth asphyxia who had encephalopathy if one or more of the following were present. Altered sensorium, inability to feed and convulsions (7). The data was uploaded regularly by the data coordinator of every SNCU to the health management information system (HMIS) of government of Karnataka and the deaths up to 4 weeks related to asphyxia was calculated.
Statistical analysis
Assumption of normality of the data was assessed using Q-Q plot. Descriptive statistics was reported as mean and standard deviation for the continuous variables. Categorical variables were reported as number and percentages. Knowledge and skill scores were compared before and after the training by the paired t -test. P value of less than 5% was considered as statistically significant. Analysis was carried out using SPSS version 25.0
Results
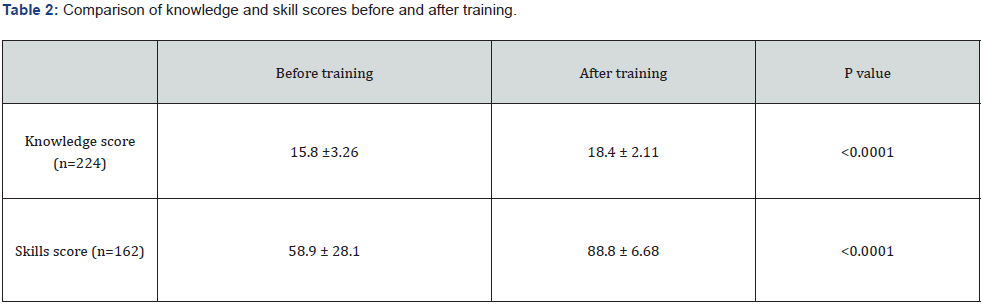
There were 276 HCWS from 8 high priority districts who attended that workshop. There were 33, 36, 34, 33, 34, 36, 32, 38 number of participants from Bidar, Chamarajanagar, Chitrdurga, Gadag, Haveri, koppal, Yadgir, Tumkur districts respectively. There were 197 (88%) staff nurses, 27(12%) medical officers and female HCW were 199 (88.9%). The nurses worked in labor rooms after completion of the training. The total number of deaths in the abovementioned districts was 346 (27.4%) in the year April 2017- Mar 2018 which was taken as a baseline and from April 2018-Mar 2019 was 248(21.4%) and from April 2019 to Dec 2019 (9 months) was 182 (17.3%). It was observed that the percent of reduction in mortality from 2017- 2018 to 2018 – Mar 2019 was 28%, p<0.01) and from April 2017- Dec 2019 (2 year, 9 months) was 57% (p<0.001). The reduction in mortality was statistically significant over time. (Table-1). Comparison of knowledge and skill scores before and after training is presented in (Table 2). Significant improvement in knowledge and skills was noted after resuscitation training (p=<0.0001).
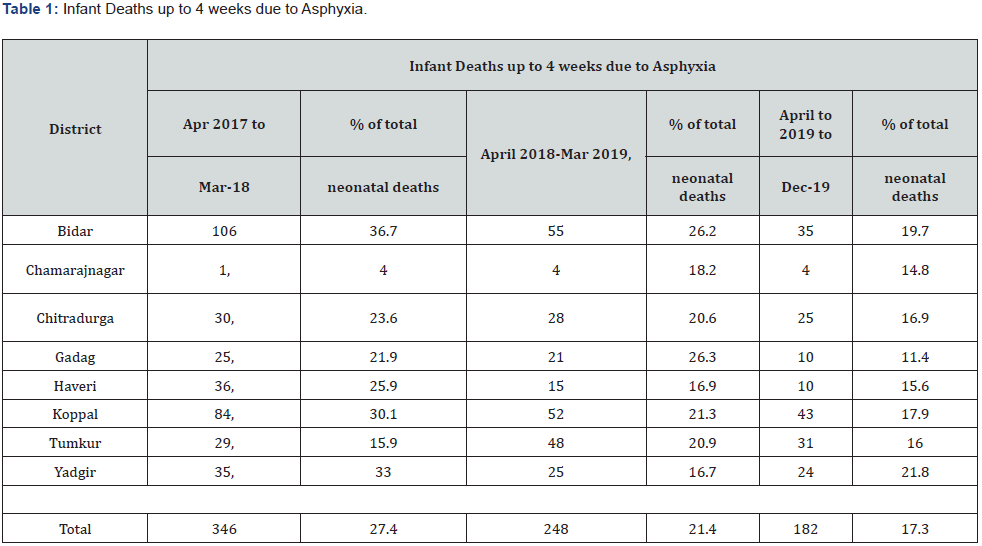
*Source: HMIS
(Table 2) shows the increase in knowledge and skill scores, which was significantly higher immediately post workshop. Hence, the workshops served the purpose of sharpening the already existing skills in resuscitation and create a sound knowledge base for the participants. Although the retention of skills was not done due to difficulty at the administrative level, the significant change noted in the drop in deaths due to perinatal asphyxia reflects the efficacy of these workshops in improving the skill of HCWS for significant duration.
Reported as mean ± SD
Discussion
The overall daily risk of mortality in the first 4 weeks of life is ~30 fold higher than the post-neonatal period, that is, from 1 month to 59 months of age. Low decline in neonatal mortality rate (NMR) in most countries including India, has hampered achieving the Millennium Development Goal-4 (MDG 4) by the year 2015 [8]. The studies have shown that the HCWS who attends delivery have substandard knowledge and skills in resuscitation [9-13,15] and NRP training will reduce mortality and improve the skills and knowledge of HCW across the world. In a study by Ogunlsi et al. only 14.0% had attended NR course within the last 5 years. The knowledge of appropriate decisions and actions during Neonatal Resuscitation (NR) was low. Koonwar et al and Gebreegziabher et al. have reported that the knowledge and skills were low at baseline [9-11]. Hence, training the HCW in neonatal resuscitation is needed to enhance their knowledge and skills necessary to manage emergency situations. Peacock et al has stressed upon the importance of confidence and skills in attending deliveries and initiating newborn resuscitation [12]. Narayan S has opined that to know the impact of training the same test has to be given after the training [13]. It has been a major challenge to impart the concept of new-born resuscitation extensively. Health workers attending birth are either not confident in resuscitation techniques or the equipment may not be available, or it may be non-functional. Moreover, there is a tendency to overuse of resuscitation procedures. Therefore, in addition to the training of health workers, regular assessments of the quality-of-care new-born receive around birth, including appropriate use of resuscitation, are required [14]. A study by Koonwar S et al. on fifty nursing personnel, has shown that the overall mean scores of knowledge and skill pre -and post training were (11.12 ±4.18, 5.98±1.68) Vs (27.28±1.45, 16.28±0.99) respectively (P<0.0001).
Effectiveness of the training programme as demonstrated as a t value of 37.27 and p value <0.0001 was highly significant (10). The correlation between the pre-test knowledge and skill was r=0.97 i.e., positive correlation between knowledge and skill of the nursing personnel regarding neonatal resuscitation protocol. In our study, Comparison of knowledge and skills scores before and after the training was 15.8 ± 3.26 Vs 18.4±2.11 (P value-<0.0001) and 58.9 ± 28 Vs 188.8 ± 6.68 (P value <0.0001) respectively. The nurses were not officially trained before though they were allowed to attend deliveries. This could be the reason for low scores on knowledge and skills. The nurses who got trained in NRP were deputed to other areas to work, where there was no exposure to delivery, which allowed them to forget the skills learnt.
The finding in our study favours the study by Enweronu et al. who reported the median pre-training and post training scores to be 38% and 71% for midwives, 43% and 81% for nurses, 52% and 90% for nurse anaesthesiologists, and 62% and 98% for physicians (p < 0.001). This again stresses upon the low baseline scores before training. Among the 271 professionals with their experience (18 nurse anaesthetists, 55 nurses, 68 physicians, and 130 midwives), it has been shown that midwives at primary health care facilities were less likely to achieve passing post-test scores than midwives at secondary and tertiary facilities [35/53 vs. 24/26 vs. 45/51 (p = 0.004)] respectively [15]. Gebreegziabher et al. (11) have shown in his study that the baseline score in knowledge and skill was substandard in 150 participants. Overall mean scores of knowledges and skills of midwives, nurses, and residents were 19.9 (SD=3.1) and 6.8 (SD=3.9), respectively [10]. A study by Taksande et al. also favour our finding [16]. Our finding was similar to that in a study conducted by Ogunlsi TA et al. The mean in pre-test was 5.98±1.68 compared to the post- test skill test mean 16.28±0.99 [9].
Another study similar to ours Xiang Ding et al, in 23 HCW (nurses, midwives, physicians and administrators’ neonatal resuscitation) assessed knowledge and skills after 2 days training and 2 days of refresher course after 9 months). The knowledge mean scores before and after the training increased from 9.60 to 13.60 (95% CI: −5.900; −2.099, p < 0.001). After 9 months, the scores increased from 10.80 to 15.44 (95% CI: −6.062; −3.217, p < 0.001). The mean knowledge scores post-training over time were 13.60 after 1st training and 15.44 after refresher course 2018 (95% CI: −3.489; 0.190, p = 0.030). The resuscitation skills performance between the two time periods increased from a mean of 32.26 (SD = 2.35) to a mean of 42.43 (SD = 1.73) (95% CI: −11.402; −8.945, p < 0.001). They concluded that continuous neonatal resuscitation training is essential to provide confidence in healthcare professionals and to improve neonatal outcomes [17]. Retention of knowledge and skills has always been a challenge and studies have shown that there is a decline of the same over time. Hence, training needs to be repeated at regular intervals to reinforce the learning and to increase confidence [12]. In Zambia, Carlo WA et al. has shown the importance of refresher training and it should be provided on a regular basis, as frequently as every 6 months, to prevent loss of skills. In his study the resuscitation knowledge and skills of midwives declined significantly 6 months after a neonatal resuscitation program training [18]. Indira et al. have reported 88% of providers remained competent to perform neonatal resuscitation at 6 months following regular supervisory and retraining visits conducted in group sessions every 3 months [19]. Many have recommended that a Monthly, quarterly and biannual resuscitation refresher courses have been demonstrated to be more effective than longer intervals [20].
A systematic review of neonatal resuscitation training in lowresource settings showed that significant declines in knowledge and skills were mitigated by refresher trainings [21]. However, skills may decline at different rates, depending on various provider characteristics, such as the type of facility where the provider works, prior resuscitation training, and type of training (initial vs. refresher) [22]. Reduction in mortality by training. A study by Zhu X et al. in rural China has shown that a training program in modern resuscitation at primary maternal health centres was associated with a reduction in intrapartum-related case fatality rate from 7.1% to 0.45% [23]. A study by A study by Zhu XY et al. in Zhuhai has shown that training all delivery room staff in the American Academy of Pediatrics, resulted in a 63% reduction in early neonatal mortality from 9.9 per 1000 before training to 3.4 per 1000 after training [24]. A study by Vakrilova L et al. in Bulgaria, a training program of all delivery room staff resulted in a 13% reduction in neonatal mortality [25]. there are studies estimating an additional 20–40% neonatal lives saved with adequate coverage of basic neonatal resuscitation at all sites where a baby may be born [26,27].
It is observed from our study that the percent of reduction in mortality from 2017-18 to 2018-2019 financial year was 28%,p<0.001) and April 2017 - Dec 2019 (2 years, 8 months) was 57% p<0.001). The reduction in mortality was statistically significant over time. A meta-analysis, which included three large communitybased trials by Pammi et al. where they implemented standardised formal neonatal resuscitation training (SFNRT) programme and showed a reduction in neonatal mortality and morbidity, improve acquisition, retention of knowledge and skills. The birth attenders were trained in neonatal resuscitation in addition to basic new born care showed decreased early neonatal mortality [risk ratio (RR) 0.85 (95% CI 0.75– 0.96)], 28-day mortality [RR 0.55 (95% CI 0.33–0.91), decreasing trends were noted for late neonatal mortality [RR 0.47 (95% CI 0.20–1.11)] and perinatal mortality [RR 0.94 (95% CI 0.87–1.00)], but there were no differences in fresh stillbirths [RR 1.05 (95% CI 0.93–1.20)] [28]. Another systematic review and meta- analysis by Patel A et al. included 20 trials, to assess the impact of neonatal resuscitation training (NRT) programme and showed that post-NRT, decreased the risk of all stillbirths by 12% (RR 0.88, 95% CI 0.83 to 0.94), fresh stillbirths by 26% (RR 0.74, 95% CI 0.61 to 0.90), 1-day neonatal mortality by 42% (RR 0.58, 95% CI 0.42 to 0.82), 7-day neonatal mortality by 18% (RR 0.82, 95% CI 0.73 to 0.93), 28-day neonatal mortality by 14% (RR 0.86, 95% CI 0.65 to 1.13) and perinatal mortality by 18% (RR 0.82, 95% CI 0.74 to 0.91), compared to Pre NRT [29]. A study in India has demonstrated that even if the resuscitation is attended by Trained Birth Attendants, the significant reduction by 60% (14.2 to 5.7 for mild asphyxia). Asphyxia specific mortality rate was reduced by 65% compared to the times when CHW (community health workers) were trained, and case fatality of severe asphyxia was reduced by 48% [30].
Limitations
Even though the HMIS data was generated by the Government of Karnataka (GOK), mortality rates were under reported. The exact data on mild, moderate, and severe asphyxia, true perinatal mortality (PMR), early neonatal mortality (ENMR), and Neonatal mortality rate (NMR) were not available.
Future directives
Universal training of all HCWs, who attend delivery must be made compulsory. The finding of this study should be confirmed on a large sample size and needs to be implemented in other states. High frequency low dose training, to reinforce the learning and increase confidence and sustainability of knowledge and skill. The train-the-trainer (TOT) model and mentoring programme will contribute towards sustainability of knowledge and skills.
Acknowledgement
We acknowledge the IAP-NRP FGM team Dr SS Kamath, Dr CP Bansal, Dr Somashekhar, Dr Vikas Goyal for constant encouragement and support. We thank The Deputy directors, Health, and family welfare for deputing the HCW from the government SNCUs. (Dr Ramachandra Bairy, Dr Prabhu, Dr Chandrakala) All the faculties who were a part of the training. Dr Yamuna, SNCU coordinator who helped us coordinate the programme. The statistician Ms Sumitra Selvam for assisting us in the statistical part of the study.
References
- Baqui AH, Darmstadt GL, Williams EK, Kumar V, Kiran TU, et al. (2006) Rates, timing and causes of neonatal deaths in rural India: implications for neonatal health programmes. Bull World Health Organ 84(9): 706-713.
- Liu L, Johnson HL, Cousens S, Perin J, Scott S, et al. (2012) Global, regional and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000 Lancet 379: 2151-2161.
- Dawodu A (1998) Neonatology in developing countries: Problems, practices and prospects. Ann Trop Paediatr 18: S73-S79.
- Saugstad OD (1998) Practical aspects of resuscitating asphyxiated newborn infants. Eur J Pediatr 157(S1): S11-S15.
- Wall SN, Lee AC, Niermeyer S, English M, Keenan WJ, et al. (2009) Neonatal resuscitation in low-resource settings: what, who, and how to overcome challenges to scale up. Int J Gynaecol Obstet 107(Suppl 1): S47-S64.
- Rowe AK, Rowe SY, Peters DH, Halloway KA, Chalker J et al. (2018) Effectiveness of strategies to improve health-care provider practices in low-income and middle-income countries: a systematic review. Lancet Glob Health 6(11): e1163-1175.
- (2011) Facility Based Newborn care operational guidelines Guidelines for planning and implementation Ministry of Health and family welfare. Governament of India.
- Sankar MJ, Neogi SB, Sharma J, Chauhan M, Srivastava R et al. (2016) State of newborn health in India. Journal of Perinatology 36(s3): S3-S8.
- Ogunlsi TA, Dadeke O, Adekanmbi FA, Fetuga BM, Okeniyi AJ (2008) Neonatal resuscitation: knowledge and practice of nurses in western Nigeria. South African Journal of Child health 2: 1.
- Koonwar S, Kumari R, Kumar S, Verma S (2016) The effectiveness of teaching on standardized neonatal resuscitation protocol in relation to knowledge and skills of nursing personnel in tertiary care hospital. Int J Contemp Pediatr 3: 1239-1243.
- Gebreegziabher E, Aregawi A, Getinet H (2014) Knowledge and skills of neonatal resuscitation of health professionals at a university teaching hospital of Northwest Ethiopia. World J Emerg Med 5(3): 196-202.
- Peacock P J, Woodman A, Mccay W, Sarah E Bates (2016) Resuscitation of the Newborn: Simulating for Confidence. Cureus 8(9): e790.
- S Narayan, SS Mathai, K Adhikari, A Bhandari, KS Bawa (2004) Effectiveness of Teaching of Neonatal Resuscitation Programme at a Workshop for a Mixed Population of Medical Personnel. Med J Armed Forces India 60(3): 244-246.
- (2012) WHO guideline Guideline on basic neonatal resuscitation. 61 pages.
- Enweronu LC, Engmann C, Osafo A, Bose C (2009) Evaluating the effectiveness of a strategy for teaching neonatal resuscitation in West Africa. Resuscitation 80(11): 1308-1311.
- Taksande MA, Vilhekar KY (2012) Neonatal resuscitation training programme, its efficiency at rural hospital. Medical J Islamic World Academy of Sci 20(1): 6-9.
- Ding X, Wang L, Msellem MI, Hu Y, Qiu J, et al. (2021) Evaluation of a Neonatal Resuscitation Training Programme for Healthcare Professionals in Zanzibar, Tanzania: A Pre-post Intervention Study. Front Pediatr 9: 693583.
- Carlo WA, Wright LL, Chomba E, McClure EM, Carlo ME et al. (2009) Educational impact of the neonatal resuscitation program in low-risk delivery centres in a developing country. J Pediatr 154(4): 504-508.
- Indira N (2009) Personal Communication.
- Anderson R, Sebaldt A, Lin Y, Cheng A (2019) Optimal training frequency for acquisition and retention of high-quality CPR skills: A randomized trial. Resuscitation 135: 153-161.
- Reisman J, Arlington L, Jensen L, Louis H, Suarez-Rebling D (2016) Newborn resuscitation training in resource-limited settings: a systematic literature review. Pediatrics 138(2): e20154490.
- Bang A, Bellad R, Gisore P, Patricia Hibberd, Archana Patel, et al (2014) Implementation and evaluation of the Helping Babies Breathe curriculum in three resource limited settings: does Helping Babies Breathe save lives? A study protocol. BMC Pregnancy Childbirth 14: 116.
- Zhu X (1993) Neonatal resuscitation. World Health Forum 14(3): 289-290.
- Zhu XY, Fang HQ, Zeng SP, Li YM, Lin HL, et al. (1997) The impact of the neonatal resuscitation program guidelines (NRPG) on the neonatal mortality in a hospital in Zhuhai, China. Singapore Med J 38(11): 485-487.
- Vakrilova L, Elleau C, Sluncheva B French-Bulgarian program “Resuscitation of the newborn in a delivery room”-results and perspectives.
- Musafili A, Essen B, Baribwira C, Rukundo A, Persson LA (2013) Evaluating Helping Babies Breathe: training for healthcare workers at hospitals in Rwanda. Acta Paediatr 102(1): e34-38.
- Seto TL, Tabangin ME, Josyula S, Taylor KK, Vasquez JC (2015) Educational outcomes of Helping Babies Breathe training at a community hospital in Honduras. Perspect Med Educ 4(5): 225-232.
- Pammi M, Dempsey EM, Ryan CA, Barrington KJ (2016) Newborn Resuscitation Training Programmes Reduce Early Neonatal Mortality. Neonatology 110(3): 210-224.
- Patel A, Khatib MN, Kurhe K, Savita Bhargava, Akash Bang (2017) Impact of neonatal resuscitation trainings on neonatal and perinatal mortality: a systematic review and meta-analysis. BMJ Paediatrics Open 1(1): e000183.
- Bang AT, Bang RA, Baitule SB, Reddy HM, Deshmukh MD (2005) Management of birth asphyxia in home deliveries in rural Gadchiroli: the effect of two types of birth attendants and of resuscitating with mouth-to-mouth, tube-mask or bag-mask. J Perinatol 25(Suppl 1): S82-91.
- Van Heerden C, Maree C, Janse Van Rensburg ES (2016) Strategies to sustain a quality improvement initiative in neonatal resuscitation. Afr J Health Care Fam Med 8(2): a958.






























