Physiological Effects of Music Therapy in Neonatal Intensive Care Setting Observational Study
Scott Brown1*, Katelyn Banks2, Hranush Danelyan3 and Raffi Tachdjian4
1Pacific Northwest University of Health Sciences, University of California, Children’s Music Fund Lead Research Coordinator, USA
2Pacific Northwest University of Health Sciences, Seattle Pacific University, USA
3Resident, Tucson Medical Center, USA
4Clinical Professor of Medicine and Pediatrics, UCLA School of Medicine, UCLA Health, USA
Submission: January 31, 2020; Published: April 20, 2022
*Corresponding author:Scott Brown, Pacific Northwest University of Health Sciences University of California, Los Angeles Children’s Music Fund, 3614 Englewood Avenue, Unit B Yakima, WA, 98902, USA7
How to cite this article:Scott B, Katelyn B, Hranush D, Raffi T. Physiological Effects of Music Therapy in Neonatal Intensive Care Setting Observational Study. Acad J Ped Neonatol 2022; 11(3): 555867. 10.19080/AJPN.2022.11.555867
Introduction
Neonatal Intensive Care Unit (NICU) infants are known to experience pain and anxiety during the multiple procedures they undergo in the first two weeks of life [1,2-5]. These stressors often result in a decline in oxygen saturation, increase in heart rate, increase in blood pressure, and elevation in pain scores. It is imperative to mitigate added stress in this population due to the long-term developmental ramifications of this physical stress. Previous literature demonstrates that music therapy-based interventions can return these physiologic parameters to baseline and even improve them. Studies on music therapy in the neonatal population are scarce, with two to four publications per year, and typically involve the high severity group that are intubated. Many of these studies have focused on the effects of music therapy on physiological vital signs such as heart rate, blood pressure, and oxygen saturation. While some studies examine the pain levels in NICU intubated patients, many base their measurements for stress on a patient’s vital signs [3,6,7]. However, few research teams have studied non-intubated NICU patients, and have rarely utilized standardized pain scales such as the Face Legs Activity Cry Consolability (FLACC) Scale or the Neonatal Infant Pain Scale (NIPS) to determine their results. Our study aims to address these gaps in knowledge by observing music therapy interventions based on time of the session, non-intubated neonates, and using perceived stress scales. According to the American Music Therapy Association (AMTA), music therapy is an evidence-based intervention offered as part of the multidisciplinary healthcare team [4]. For neonatal patients, interventions include parental songwriting with instruments, music-assisted relaxation, and womb sounds. Unlike many other studies in established literature,our study was exclusively facilitated by board-certified NICU trained Music Therapists.
Music therapy sessions were conducted from 2017-2020 in a level three NICU in Los Angeles, USA. These sessions ranged from fifteen minutes to one hour. Our team retrospectively analyzed data from de-identified, non-intubated patients ranging from zero to thirty-six weeks in age. A FLACC scale was used by music therapists working with the neonatal subject. Since all patients in the NICU are definitionally under three months of age, the FLACC pain scale was used to derive a better assessment for associated pain and distress levels. Overstimulation cues were used by music therapists to determine the FLACC score. The FLACC pain scale is a pain assessment for nonverbal patients based on facial expressions, legs, activity, crying, and consolability. If a patient exhibited a score higher than two from the initiation of a session, the music therapy session was terminated at that time. Pre- and post-session vitals were captured by monitors and transcribed by the Music Therapist. These included heart rate and blood oxygen saturation on room air. Measurements were separated into three sets which included males, females, and the aggregate group.
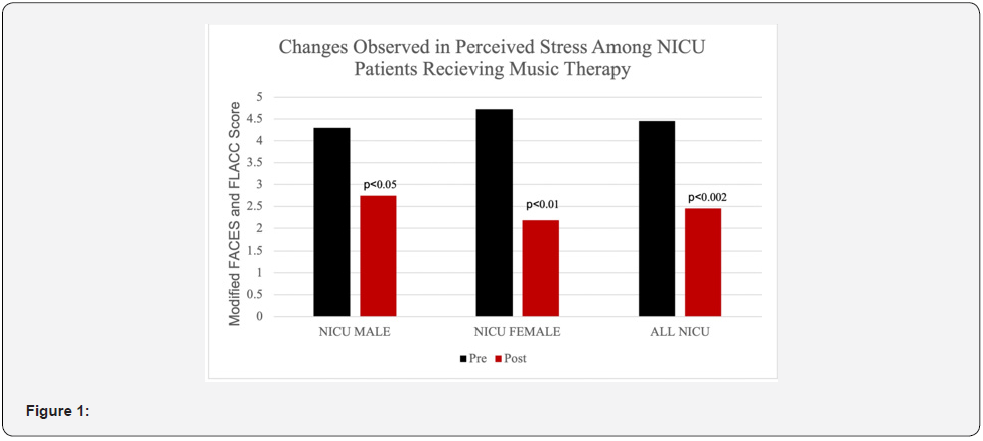
Ninety-four subjects and their music therapy sessions were analyzed for our study. Anova and Tukey tests with a P-Value < 0.05 were used to produce a ninety-five percent confidence level to determine statistical significance between groups. Our analysis indicates that music therapy can improve physiological parameters in as little as a fifteen-minute session. Figure 1 (listed below) depicts the associated decrease in pain found in the NICU data sets. Based on a FLACC scale assessment, subjects experienced an average of forty-eight percent decrease in pain going from moderate-to-severe to mild. We also observed a significant reduction in heart rate (by thirteen percent) which supports existing literature on the effects of music-assisted relaxation. A salient finding from this analysis was blood oxygen saturation improvement that was greater in females (six percent) than males—a result only previously seen in intubated patients.
During the initial five days of a hospitalization, music therapy sessions positively impacted perceived pain levels. This finding was not statistically significant most likely due to a diminishing number of patients with a length of stay greater than five days. After the initial five days, the remaining patients experienced a plateau in pain levels as measured by the modified FLACC scale. Consistent with the existing literature, we found that multiple music therapy sessions during hospitalization had a greater impact than just a single session. Finally, our data supports existing literature in regard to the appropriate length of a music therapy session for pediatric patients [1]. Given the results of our study— confirming existing literature regarding the optimal length of a music therapy session— it would be helpful to determine the optimal time to intervene with music therapy during a hospitalization and to follow the longitudinal effects of inpatient music therapy.
References
- Amini E, Rafiei P, Zarei K, Gohari M, Hamidi M (2013) Effect of lullaby sand classical music on physiologic stability of hospitalized preterm infants: A randomized trial. J Neonatal Perinatal Med 6(4): 295–301.
- Anderson DE, Patel AD (2018) Infants born preterm, stress, and neurodevelopment in the neonatal intensive care unit: Might music have an impact? Dev Med Child Neurol 60(3): 256–266.
- Caparros-Gonzalez RA, de la Torre-Luque A, Diaz-Piedra C, Vico FJ, Buela-Casal G (2018) Listening to Relaxing Music Improves Physiological Responses in Premature Infants: A Randomized Controlled Trial. Adv Neonatal Care 18(1): 58–69.
- Hohmann L, Bradt J, Stegemann T, Koelsch S (2017) Effects of music therapy and music-based interventions in the treatment of substance use disorders: A systematic review. PLOS ONE 12(11) e0187363.
- Maitre NL, Arnon S (2020) Music therapy for neonatal stress and pain—Music to our ears. J Perinatol 40(12): 1734–1735.
- Yakobson D, Gold C, Beck BD, Elefant C, Bauer-Rusek S, Anon S (2021) Effects of Live Music Therapy on Autonomic Stability in Preterm Infants: A Cluster-Randomized Controlled Trial. Children 8(11): 1077.
- Yue W, Han X, Luo J, Zeng Z, Yang M (2021) Effect of music therapy on preterm infants in neonatal intensive care unit: Systematic review and meta-analysis of randomized controlled trials. J Adv Nurs 77(2): 635–652.






























