The Traveling Child Returns with A Fever: Rats! Pediatric Hemorrhagic Fever Renal Syndrome Due to Hantavirus
MD Sarah Schneider1,2*, MD Caitlin Carter1,2and MD Manaswitha Khare1,2
1University of California, USA
2Rady Children’s Hospital, USA
Submission: September 21, 2021; Published: December 09 2021
*Corresponding author:Sarah Schneider, University of California, USA
How to cite this article:MD Sarah S, MD Caitlin C, MD Manaswitha K. The Traveling Child Returns with A Fever: Rats! Pediatric Hemorrhagic Fever Renal Syndrome Due to Hantavirus. Acad J Ped Neonatol 2021; 11(2): 555861. 10.19080/AJPN.2021.11.555861
Abstract
A 6-year-old previously healthy female from the United States presented with 5 days of high fever to 103F, abdominal pain, and vomiting. Exposure history included recent travel to Russia, Turkey, Yosemite, and the San Diego Zoo, as well as multiple mosquito bites. On admission, she was found to have thrombocytopenia, hematuria, nephrotic range proteinuria and subsequently developed acute kidney injury. Her grandfather was hospitalized shortly after her family’s departure from Russia and diagnosed with hantavirus hemorrhagic fever renal syndrome (HFRS). While extremely rare in the United States, her clinical picture was concerning for HFRS. We also considered other infections with fever and thrombocytopenia such as rickettsia, leptospirosis, dengue, hemolytic uremic syndrome, and other causes of acute glomerulonephritis including lupus nephritis, post-streptococcus glomerulonephritis. After initial complications of acute kidney injury and thrombocytopenia requiring support with intravenous fluids, the patient made an uneventful recovery. Serology tests later resulted positive for Hantavirus. This case describes a rare diagnosis in the United States, and stresses importance of HFRS should be on differential of pediatric patient with fever, thrombocytopenia, and recent travel or exposure.
Keywords: Hantavirus; Hemorrhagic Fever Renal Syndrome; Acute Glomerulonephritis; Thrombocytopenia; Fever; Acute Kidney Injury.
Abbreviations: UTI: Urinary Tract Infection; HFRS: Hantavirus Fever Renal Syndrome; HPS: Hantavirus Pulmonary Syndrome.
Case Presentation
A 6-year-old previously healthy female presented with 5 days of fever to 103 F, abdominal pain, vomiting and intermittent headaches. No rashes, easy bruising, swelling, or sore throat were reported. Exposure history was extensive and included recent travel to Russia, Turkey, Yosemite, and the San Diego Zoo, as well as multiple mosquito bites in Russia and Yosemite. Travel to Russia occurred 3 weeks prior to admission, where she stayed at her grandfather’s farm. Rodent droppings were noted around the home. She then returned to the United States where she stayed at a rental home in Yosemite and played under a porch at that house and swam in fresh water. There were no known tick bites. She had a transient febrile illness in Russia that resolved, and no other recent illnesses. She visited her pediatrician and was taking Ibuprofen for fever and Cephalexin for possible urinary tract infection (hematuria on a urinalysis, culture ultimately negative). Due to persistent fever, she presented to the Emergency Department on day 5 of illness where she was found to have significant thrombocytopenia (Platelet 34 TH/uL) without leukopenia or anemia, and an unremarkable complete metabolic panel including near normal renal function (Creatinine 0.54 mg/dL eGFR 87 mL/min by bedside Schwartz equation) and normal liver function. Urinalysis with proteinuria (3+), hematuria (2+), and markedly elevated urine protein to creatinine ratio of 21.5 mg/mg. She was admitted to Pediatric Hospital Medicine service for further management.
Interestingly, her grandfather was hospitalized 2 weeks after her family’s departure from Russia and diagnosed with hantavirus hemorrhagic fever renal syndrome (HFRS). He has since made a full recovery.
Final Diagnosis
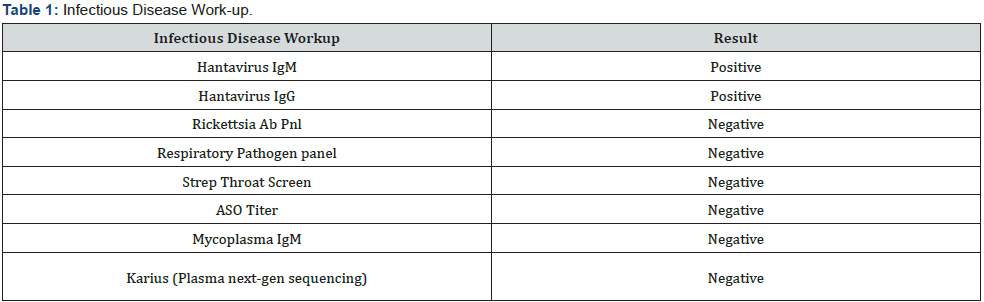
In cases of prolonged fever with significant travel history, there is a wide differential diagnosis including bacterial infections,viral infections, and autoimmune processes. Her presentation of significant proteinuria, hematuria, thrombocytopenia, and acute kidney injury (developed shortly after admission) with travel to Eastern Russia with known hantavirus exposure was concerning for HFRS. She underwent broad infectious work-up (Table 1) including Karius testing [Karius is a plasma next-generation sequencing that can detect 1000 bacterial pathogens, fungi, parasites, DNA viruses (Complete list of pathogens available at: https://kariusdx.com/ pathogenlist/3.6)] [1]. and testing for etiologies of acute kidney injury or acute glomerulonephritis (Table 2). As shown in Table 2, she tested positive for microalbumin and B2 microglobulin which are consistent with acute kidney injury. Her urine cytology did not show evidence of eosinophilia that would have been suggestive of acute kidney injury due to NSAIDs.

Hantavirus testing eventually resulted positive and diagnosis of Hantavirus Hemorrhagic Renal Syndrome was confirmed.
Hospital Course
Her admission vitals including blood pressure for age and physical examination including abdominal, neurological, and skin examination were unremarkable. Within 24-48 hours she developed acute kidney injury with elevated serum creatinine.
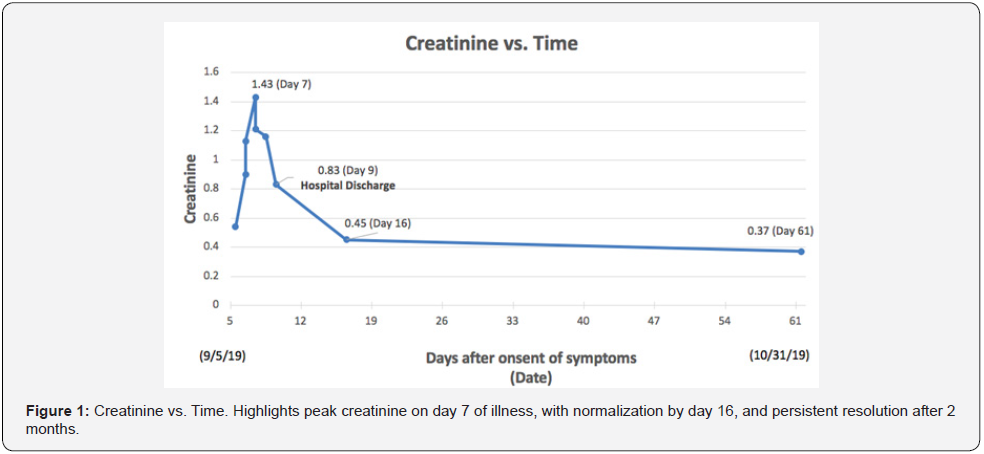
Her peak serum creatinine was 1.43 mg/dL on day 7 of illness, as demonstrated in Figure 1. She also developed mild hypoalbuminemia (albumin 2.9 mg/dL) and hyperphosphatemia (Phos 7.4 mg/dL). She remained non-oliguric throughout her 4-day hospital stay. Her thrombocytopenia improved after day 5 of illness, as shown in Figure 2. Renal ultrasound was unremarkable.
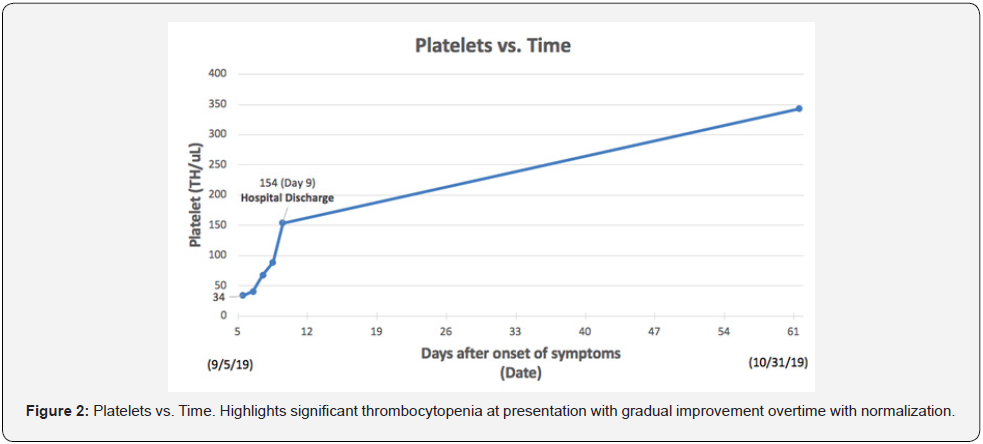
Treatment focused on supportive care and careful fluid management. She was started on intravenous fluids, a low potassium low phosphorus diet, and phosphorus binders with meals. She was discharged home after hospitalization for 4 days total. Her renal function and thrombocytopenia gradually improved and normalized over the next 2 weeks and proteinuria resolved. She did not require hemodialysis. She was seen in Nephrology Clinic 2 months after admission and was doing well with normal renal function, no proteinuria, and normal blood pressure.
Hantavirus testing resulted positive the day after discharge, confirming the diagnosis of Hantavirus hemorrhagic renal syndrome.
Discussion
Hantavirus infections can lead to life-threatening pulmonary and renal disease [2]. Hantaviruses are a genus of enveloped RNA viruses within the family Bunyaviridae [3]. Pathogenic viruses in humans are carried by rodents and transmitted through inhalation of aerosolized rodent urine, saliva, and feces [4]. Humans are generally considered dead-end hosts. The virus causes changes in blood coagulation, vasodilatation, and disturbances in the barrier function of capillaries, leading to severe capillary leak syndrome. Hantaviruses of the Old World (Europe and Asia) are known to cause HFRS, while hantaviruses of the New World (Americas) are known to cause Hantavirus Pulmonary Syndrome (HPS). Puumala virus is the most common disease causing HFRS in Western and Northern Europe, particularly in Russia, and has been known to be the cause of epidemic breakouts. In Russia, 131,590 cases of HFRS were reported during 2000-2017 from 6 different strains with a 0.4% case fatality [5]. Interestingly, most patients were age 20-50 years of age and 80% of cases were in men. Only 2.4% of cases (3,157) during this timeframe were reported in children less than 14 years old. In St. Petersburg Russia in 2019, only 2 out of 73 cases of HFRS were in children [6].
In North America, Sin Nombre virus (SNV) is the most predominant hantavirus, known to cause HPS [7]. Deer mice (Peromyscus maniculatus) found throughout North America are the reservoir for SNV [8]. The mouse prefers woodlands but also appears in desert areas. In 2012, there was an outbreak of HPS from Sin Nombre virus to visitors in Yosemite National Park due to suspected deer mouse reservoir [9]. Interestingly, our patient did have recent travel to Yosemite. However, given her clinical picture fit HFRS and her grandfather also tested positive, we suspect she most likely contracted Hantavirus during her travel in Russia. Children are thought to be less affected by hantavirus when compared to adults, but more recently have been found in highly pathogenic endemic regions were shown to be comparable [10].
According to the Centers for Disease Control and Prevention, in 2017 there was an outbreak in the United States of the Seoul virus, a hantavirus strain causing HFRS, affecting 17 people 8 including an 18-year-old female owner of infected pet rats, who was determined to be the index case [11]. In 2014, a case report was published in BMJ of a 59-year-old man in the United Kingdom who developed hantavirus HFRS from infected rats on his property [12]. He made an uneventful recovery after management with supportive care and careful fluid balance.
The acute clinical course of HFRS classically includes five phases of illness: febrile, hypotensive, oliguric, polyuric, covalescent. The febrile phase occurs day 1-7 and includes symptoms of fever, headache, vomiting, abdominal pain, back pain, visual disturbances [13] The hypotensive phase, occurring between days 1-3 of illness, is characterized by, features of capillary leak and manifests predominantly pulmonary symptoms. The oliguric phase occurs days 2-6 and features decreased urine output, fluid retention, anuria. The severity of acute kidney injury peaks in the second week of illness and is mediated by both cellular and innate immune systems, to endothelial cell infection viral infection [14]. The oliguric phase followed by the polyuric phase occurs after 2 weeks with increased urine output. Finally, the convalescent phase occurs over the next 3 to 6 months and can include symptoms of fatigue and weakness. This clinical timeframe fit our patient’s presentation; however, to our knowledge she has not shown any long-term effects of fatigue and weakness thus far. The literature on the expected course in children is sparse; a recent report from Germany compared clinical features of hantavirus infection between 295 adults and 22 children and showed no significant differences in regard to incidence or severity of AKI or thrombocytopenia, with full recovery of all patients [15]. Children were more likely to present with abdominal pain and nausea/ vomiting, which was consistent with our patient’s course. While the acute phase typically resolved, there may be an association between hantavirus exposure and future chronic kidney disease in endemic populations [16]. Because our patient’s renal disease improved with supportive care, kidney biopsy was not pursed, and it is possible that she had renal impairment and proteinuria related to NSAID exposure, however her clinical course was most consistent with hantavirus infection.
Treatment is focused generally on supportive care, as there is no current anti-viral treatment [4,17]. Ribavirin has been shown in some in vitro and in vivo studies to have some clinical effect; however, it is non-specific and is not the standard of care [18]. One prospective study of 242 patients showed intravenous ribavirin reduced mortality, but other studies have not been able to replicate this finding [19]. Our patient improved clinically without ribavirin. There is no vaccine available due to lack of adequate animal models of hantavirus-associated disease [4,17]. Currently, efforts are focused on prevention of contacts between humans and infections mammals to help prevent the spread of the virus.
To our knowledge there have been no pediatric case reports of hantavirus HFRS of a patient receiving treatment in the United States, while it is a prevalent cause of acute kidney injury throughout Europe and the western world [7]. Hantavirus infection contracted in the United States has typically been related to virus strains causing Hantavirus Pulmonary Syndrome (HPS), but not strains causing hantavirus HFRS [20]. We suspect our patient contracted the virus in Russia. Early diagnosis of HFRS has been shown to decrease medical costs and hospitalizations, as early diagnosis can prevent unnecessary testing and encourage supportive care [21]. Through this case report we hope to increase the awareness of hantavirus infection as a potential cause of hemorrhagic fever with renal syndrome in pediatric patients. This case stresses the importance of obtaining detailed travel history to determine uncommon etiologies of undifferentiated fever.
Conclusion
Hantaviruses of Old World are known to cause a clinical picture of hemorrhagic fever with renal syndrome. HFRS should be on differential of pediatric patient with fever, thrombocytopenia, and recent travel or exposure. Development of Acute Kidney Injury can be delayed from initial presentation. Management of HFRS is supportive with fluid rehydration and close monitoring of renal function and fluid status. Prevention efforts focus on eradicating infectious mammals to prevent spread of the virus.
References
- Karius (2020) Inc. Accessed.
- Tkachenko EA, Lee HW (1991) Etiology and epidemiology of hemorrhagic fever with renal syndrome. Kidney Int Suppl 35: 54-61.
- Martin Zeier, Michaela Handermann, Udo Bahr, Baldur Rensch, Sandra Müller, et al. (2005) New ecological aspects of hantavirus infection: a change of a paradigm and a challenge of prevention--a review. Virus Genes 30(2): 157-180.
- Detlev H Kruger, Luiz Tadeu Moraes Figueiredo, Jin Won Song, Boris Klempa (2015) Hantaviruses--globally emerging pathogens. J Clin Virol 64:128-136.
- Evgeniy A Tkachenko, Aydar A Ishmukhametov, Tamara K D zagurova, Alla D Bernshtein, Viacheslav G Morozov, et al. (2019) Hemorrhagic Fever with Renal Syndrome, Russia. Emerg Infect Dis. 25(12): 2325-2328.
- Ivanov D O TVN, Pavlova EB, Pavlova NV, Nazarova AN, Chernova TM, et al. (2020) Hemorrhagic fever with renal syndrome in a child early age. Journal Infectology 12(5).
- Hjelle B (2019) Epidemiology and diagnosis of hantavirus infections. In: Hirsch M, ed.
- (2020) Prevention CfDCa. Hemorrhagic Fever with Renal Syndrome.
- Jonathan J Núñez, Curtis L Fritz, Barbara Knust, Danielle Buttke, Barryett Enge, et al. (2014) Hantavirus infections among overnight visitors to Yosemite National Park, California, USA, 2012. Emerg Infect Dis20(3): 386-393.
- Tamara K Dzagurova , Evgeniy A Tkachenko, Aydar A Ishmukhametov, Mariya V Balovneva, Boris Klempa, et al (2018) Severe hantavirus disease in children. J Clin Virol 101: 66-68.
- et, al. (2017) F. MMWR Morb Mortal Weekly Report. CDC.gov.
- Kate Adams, Lisa Jameson, Rolf Meigh, Tim Brooks (2014) Hantavirus: an infectious cause of acute kidney injury in the UK. BMJ Case Rep.
- Hong Jiang, Hong Du, Li M Wang, Ping Z Wang, Xue F Bai (2016) Hemorrhagic Fever with Renal Syndrome: Pathogenesis and Clinical Picture. Front Cell Infect Microbiol 6:1.
- Eva Mittler, Maria Eugenia Dieterle, Lara M Kleinfelter, Megan M Slough, Kartik Chandran, et al. (2019) Hantavirus entry: Perspectives and recent advances. Adv Virus Res 104: 185-224.
- Fabian Echterdiek, Daniel Kitterer, M Dominik Alscher, Vedat Schwenger, Bettina Ruckenbrod, et al. (2019) Clinical course of hantavirus-induced nephropathia epidemica in children compared to adults in Germany-analysis of 317 patients. Pediatr Nephrol 34(7): 1247-1252.
- Yomani D Sarathkumara, Chandika D Gamage, Sithumini Lokupathirage, Devinda S Muthusinghe, Nishantha Nanayakkara, et al. (2019) Exposure to Hantavirus is a Risk Factor Associated with Kidney Diseases in Sri Lanka: A Cross Sectional Study. Viruses 11(8): 700.
- Rebecca L Brocato, Jay W Hooper (2019) Progress on the Prevention and Treatment of Hantavirus Disease. Viruses. 11(7): 610.
- Marcos L Moreli, Ariany C Marques-Silva, Vagner A Pimentel, Vivaldo G da Costa (2014) Effectiveness of the ribavirin in treatment of hantavirus infections in the Americas and Eurasia: a meta-analysis. Virusdisease 25(3): 385-389.
- J W Huggins, C M Hsiang, T M Cosgriff, M Y Guang, J I Smith, et al. (1991) Prospective, double-blind, concurrent, placebo-controlled clinical trial of intravenous ribavirin therapy of hemorrhagic fever with renal syndrome. J Infect Dis 164(6): 1119-1127.
- Centers for Disease Control and Prevention (CDC) (2012) Hantavirus pulmonary syndrome in visitors to a national park--Yosemite Valley, California, 2012. MMWR Morb Mortal Wkly Rep 61(46): 952.
- Alette Brorstad, Kristina Bergstedt Oscarsson, Clas Ahlm (2010) Early diagnosis of hantavirus infection by family doctors can reduce inappropriate antibiotic use and hospitalization. Scand J Prim Health Care 28(3): 179-184.






























