Rare Case of Optic Nerve Glioma Revealed by Russell Syndrome
Chaimae Khairoun1,2*, Mouna Sabib1, Toufik Meskini1, Naima Erreimi1 and Nezha Mouane1
1 Department of Pediatric Hepatology Gastroenterology and Nutrition, Rabat Children’s Hospital, Morocco
2 Faculty of Medicine and Pharmacy, Morocco
Submission:February 26, 2020; Published:March 12, 2020
*Corresponding author: Chaimae Khairoun, Department of Pediatric Hepatology Gastroenterology and Nutrition, Rabat Children’s Hospital, Rabat, Morocco
How to cite this article: Chaimae Khairoun, Mouna Sabib, Toufik Meskini, Naima and Nezha Mouane. Rare Case of Optic Nerve Glioma Revealed by Russell Syndrome. Acad J Ped Neonatol. 2020; 9(3): 555820. DOI: 10.19080/AJPN.2020.09.555820
Abstract
Optic nerve glioma (or optic glioma), is a rare form of glioma which affects the optic nerve. There is very little data available in the literature that describes this pathology. It represents 5% of brain tumors in children. The diagnosis is always made on the occasion of ophthalmological clinical signs (nystagmus, loss of visual acuity). In some cases, its mode of revelation is uncommon, delaying the diagnosis and the treatment. Through our work, we have reported the case of a 17-month-old infant with optic chiasm glioma, revealed by diencephalic cachexia evolving since the age of 5 months. The child was put on enteral nutrition at constant flow rate and polychemotherapy with an improvement in the clinical state and radiological stabilization after a 3-month follow-up.
Introduction
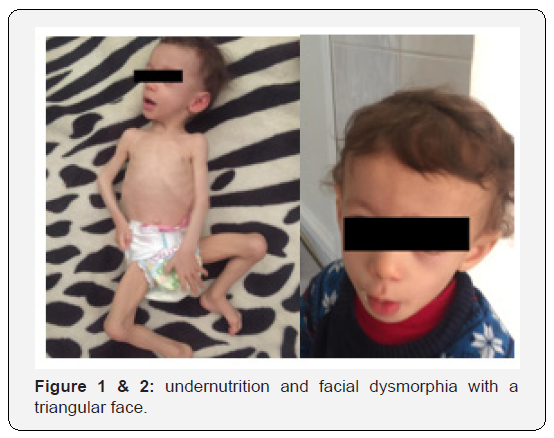
Diencephalic cachexia (Russell syndrome) was first described in 1951 by Russel [1]. It affects young children under the age of one with an average age of 6 months. It includes all of the clinical signs (severe weight loss despite an adequate caloric intake and absence of neurological abnormalities) linked to hypothalamic dysfunction, related to lesions occupying the space of the optic chiasm region (low grade gliomas) or tumors near the fourth ventricle [2] and whose mechanism remains unexplained. We report a case of optic chiasm glioma, diagnosed at 17 months of age with severe undernutrition and a facial dysmorphia explained by Russell syndrome.
Observation
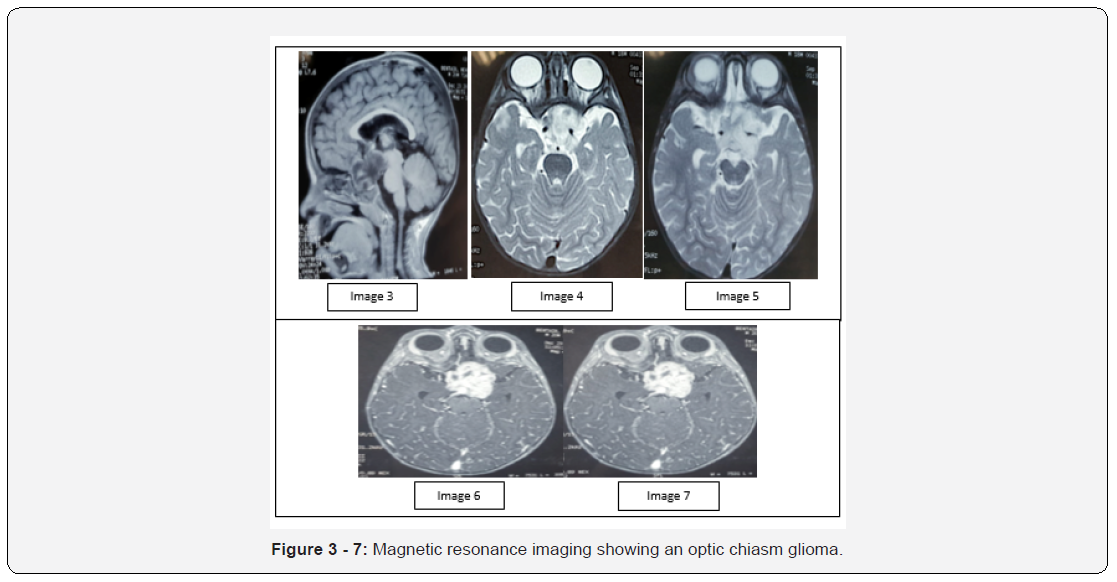
It’s about a 17-month-old infant of non-consanguineous parents. He was the second of two siblings (a healthy 4-year-old sister). He was admitted to the pediatric gastroenterology department for moderate undernutrition. He was on exclusive breastfeeding from birth until the age of 2 months before turning to artificial milk. It was diversified at the age of 6 months with an adequate caloric intake. Its symptomatology goes back at the age of 5 months with severe anorexia, weight-loss stagnation and involuntary movements of the two eyeballs. The clinical admission examination showed a conscious, overactive child, a delay in weight with an estimated weight of 6.8 kg (-3DS) and an estimated size of 75 cm (-2DS), while the cranial perimeter was normal at 48cm. Mild to moderate undernutrition with a pasty fold of undernutrition and sign of slump were observed. We observed also a facial dysmorphia with a triangular face, a pointed chin and a bulging forehead evoking the Russell syndrome (Figure 1 & 2). The rest of the somatic examination did not find any signs in favour of neurofibromatosis. Ophthalmologic examination showed an accentuated bilateral rotary nystagmus in the left eye and a unilateral oedema of the left eye in stage I. The malabsorption and hormonal balance were normal. The eso-gastro-duodenal fibroscopy was normal and the jejunal biopsy objectified the absence of villous atrophy, the absence of metaplasia or dysplasia and pathogenic microorganism. Brain magnetic resonance imaging showed the presence of an optic chiasma glioma. In fact, the MRI has shown the presence of a medial suprasellar lesion process lateralized to the left, poorly limited, in T1 hypo signal (Figure 3), T2 hypersignal (Figure 4 & 5) and flair, without translation on the diffusion sequences, enhanced heterogeneously after injection of gadolinium (Figure 6 & 7), measuring 35X37, 5X26cm (TX AP XH).
On the topographic plan:
a) From behind, it fills the inter-peduncle cistern, with discreet mass effect on the left mesencephalic peduncle.
b) Forward, it encompasses the optic chiasm and extends along the path of the left optic nerve without endo-orbital extension.
c) At the top, comes into contact with the 3rd ventricle.
d) At the bottom, she widens the sella turcica with respect for the physiological T1 hypersignal of the post-pituitary gland.
e) Laterally, it includes the middle and anterior cerebral arteries which remain permeable. (Figure 3-7)
The biopsy was not performed on our patient due to the risk of blindness. Regarding the therapeutic issue, the child was “retyped” nutritionally where he was put on enteral nutrition at constant flow for one month. Due to the achievement of optic chiasm, a chemotherapy combining Carboplatin and Vincristine was established following the LGG protocol. This recommended treatment was accompanied by regular quarterly pediatric, ophthalmological and radiological monitoring in order to look for signs of progression of this pathology. After a 3-month followup, the patient presented an improvement in the clinical state marked by an increase in weight estimated at 4 kg and radiological stabilization (image 8) as the cerebral control MRI was in favor of a chiasma glioma optical appearance stable compared to the MRI of 9/30/2019.

Discussion
Glioma of the optic nerve is rare and poorly described in the literature. Tt represents 5% of childhood brain tumors. Its frequency is less than 5% [3] and its prevalence in the general population is 1 per 100,000 [4]. Most childhood gliomas are sporadic, but in 30 to 58% of cases, they are associated with neurofibromatosis type 1 [5]. These sporadic cases are more aggressive with rapid chiasmatic and retro-chiasmatic expansion whereas cases linked to neurofibromatosis remain confined to the optic nerve and have a slower progression [4,6]. Gliomas of the optic nerve are usually revealed around the age of 2 to 7 years [7], by a decrease in visual acuity, an abnormality in the fundus, strabismus, exophthalmia, nystagmus [4,8] and signs of retinal ischemia [9] or gonadal disorders [10]. Our patient presented as signs a bilateral rotational nystagmus more marked on the left and moderate undernutrition for the 5th month of life in connection and a facial dysmorphia with diencephalic cachexia or Russell syndrome, which constitutes a rare mode of revelation of this pathology. This atypical clinical presentation delayed the diagnosis, which can affect the visual functional prognosis [4]. Cerebral MRI with Gadolinium injection is essential in order to assess the intra-orbital or even intracerebral extension by visualizing the optic chiasm [11]. In case of our patient, imaging revealed pathognomonic signs, showing a poorly limited medial suprasellar lesion process lateralized to the left, in T1 hypointense, T2 hypersignal and flair, without translation on the diffusion sequences, enhanced heterogeneously after injection of gadolinium. Biopsy is not always necessary for histological confirmation [6]. In the case of our patient, the biopsy was not done given the location of the tumor and the risk of blindness. The aim of the treatment is to preserve visual acuity and to avoid the bilateralization of the tumour. Polychemotherapy remains the first-line treatment, combining vincristine and carboplatin [6,12,13], especially in the event of an active tumor and in children aged less than 7 years [14]. Surgical treatment is indicated as firstline treatment, in the event of a tumor limited to the optic nerve without chiasmatic involvement, with severe impairment of visual acuity and lack of possibility of recovery, severe exophthalmos and threat of chiasmatic injury [6,12,15]. Radiation therapy is indicated in the event of tumor progression despite chemotherapy or in case of a life-threatening threat due to intracranial hypertension by tumour compression [6,12]. The child presented an optic chiasm with a risk of bilateral blindness in the event of surgical treatment, hence the implementation of LGG chemotherapy with stabilization of the clinical, nutritional and radiological state after a 3-month follow-up.
Conclusion
The diagnosis of optic chiasm glioma in a young infant is rare, especially in case of atypical clinical picture such as diencephalic cachexia, which constitutes a rare mode of revelation that can delay the diagnosis and management until the blindness stage. Chemotherapy is the first-line treatment given the risk of blindness.
References
- Russel A (1950) A diencephalic syndrome of emaciation in infancy and childhood. Arch Dis Child26:274-2
- Poussaint TY, Barnes PD, Nichols K, Anthony DC, Cohen L, et al. (1997) Diencephalic syndrome: clinical features and imaging findings. American journal of neuroradiology18(8):1499-1
- Levecq L, De Potter P, Guagnini A-P (2005) Epidemiology of ocular and orbital lesions addressed to an ocular oncology center. French Journal of Ophthalmology 28(8): 840-844.
- Singhal S, Birch JM, Kerr B, Lashford L, Evans DGR (2002) Neurofibromatosis type 1 and sporadic optic gliomas. Acute paediatrics87(1):65-70.
- Lena G, Pech-Gourg G, Scavarda D, Klein O, Paz-Paredes A (2010) Glioma of the optic nerve in children. Neurosurgery 56(2-3): 249-2
- Shapey J, Danesh-Meyer H, Kaye A (2011) Diagnosis and management of optic nerve glioma. J Clin Neurosci18(12):1585-15
- Viennet A, Nezzar H, Bonnin N, Sinardet D, Campagne D, et al. (2008) An optic nerve glioma in a 4-month-old childJ Fr Ophtalmol31(6 Pt 1):618-6
- Mikaeloff Y, Chaix Y, Grill J, Adamsbaum C, Bursztyn J, Rubie H, et al. (2002) Optic pathway gliomas in neurofibromatosis type I. Longitudinal study of 30 cases in two multidisciplinary practices. Arch Pediatr9(8):797-804.
- Rebika S, Bonnin N, Kémény J, Chiambaretta F, Bacin F (2015)Apropos of 5 cases of optic nerve tumors diagnosed during a 6-year-period. J Fr Ophtalmol38(1):13-21.
- Elguecier A, Rahel A, Meskine D (2016) Chiasma glioma revealed by gonadal disorders in 2 cases. Annals of Endocrinology.
- Balcer LJ, Liu GT, Heller G, Bilaniuk L, Volpe NJ, et al. (2001) Visual loss in children with neurofibromatosis type 1 and optic pathway gliomas: relation to tumor location by magnetic resonance imaging. Am J Ophthalmol131(4):442-44
- Genol I, Troyano J, Ariño M, Iglesias I, Arriola P, García-Sánchez J (2009) Meningocele, glioma and optic nerve meningioma: differential diagnosis and treatment. Arch Soc Esp Oftalmol84:563-56
- Demaerel P, De Ruyter N, Casteels I, Renard M, Uyttebroeck A, et al. (2002) Visual pathway glioma in children treated with chemotherapy. Eur J Paediatr Neurol6(4):207-2
- Wilhelm H (2009) Primary optic nerve tumours. Curr Opin Neurol22(1):11-1
- Lena G, Pech-Gourg G, Scavarda D, Klein O, Paz-Paredes A (2010) Optic nerve glioma in children. Neuro-Chirurgie56(2-3):249-2






























