Behavior Problems and Attention Deficit Hyperactivity Disorder in Children and Adolescents with Neurofibromatosis Type 1
Ornella Piscitelli1, Alice Monda1, Maria C Digilio2, Rossella Capolino2 and Vincenzo Di Ciommo2*
1Child Psychiatry Unit, Department of Neuroscience, Bambino Gesù Children’s Hospita, Italy
2Clinical Genetics, Department of Pediatrics, Bambino Gesù Children’s Hospital, Italy
Submission: June 16, 2017; Published: August 03, 2017
*Corresponding author: Vincenzo Di Ciommo, Bambino Gesù Children’s Hospital, Professiona Developmental, Piazza S. Onofrio 4, Roma 00165, Roma, Italy.
How to cite this article: Ornella P, Alice M, Maria C D, Rossella C, Vincenzo D C. Behavior Problems and Attention Deficit Hyperactivity Disorder in Children and Adolescents with Neurofibromatosis Type 1. Acad J Ped Neonatol. 2017; 5(2): 555716. DOI:10.19080/AJPN.2017.05.555716
Abstract
Aim:To estimate the prevalence of Attention Deficit Hyperactivity Disorder (ADHD) and of behavioral disorders in children and adolescents with Neurofibromatosis Type 1 (NF1), evaluating possible associations between them
Methods: Patients with NF1 were consecutively enrolled from the outpatient clinic of a pediatric hospital, with their parents as informants. To assess behavior disorders Child Behavior Check List (CBCL) was administered, and parents inattention disease scale (SDAG) with teachers inattention disease scale (SDAI) were used to identify ADHD according to the criteria of the DSM-IV.
Results: Sixty-eight patients with NFI were investigated (mean age 9 years 6 months). Twenty-nine of them fulfilled the criteria of ADHD, with a prevalence of 42.6%. Thirty-one of the patients disclosed problems of behavior (45.6%), with an higher prevalence of internalizing problems in comparisons of externalizing behaviors. Scores of behavior problems were significantly higher in patients with inattentive or combined ADHD than in patients without. Combined ADHD was associated to externalized behavioral problems while the inattentive type was associated to internalized problems.
Interpretation: Behavioral problems and ADHD are common in children and adolescents with NF1 and a link between ADHD and psychological problems can be suggested, but the origins of this relationship remain to be elucidated.
Keywords: Neurofibromatosis; Attention deficit; Behavior; Children; Adolescents
Abbrevations: CBCL: Child Behavior Checklist; SDAG: Parents inattention disease scale; SDAI: Teachers inattention disease scale; SD: Standard Deviations; ADHD: Attention Deficit Hyperactivity Disorder
Introduction
Neurofibromatosis, type 1 (NF1) is a rare, autosomal dominant genetic disorder. It is associated with a mutation on the long arm of chromosome 17, and has highly variable phenotypic expression. Children and adolescents with NF1 have a high incidence of neuropsychological and learning impairments [1]. In 1988 the Conference of the National Institutes of Health established the diagnostic criteria of Neurofibromatosis 1 that were subsequently reconfirmed in 1997 [2].
In addition to the somatic manifestations, the features of the syndrome have been recognized as including neuropsychological and cognitive problems. The psychological aspects have only recently become of interest of clinicians and other professional figures [3]. In spite of the self-concept of children and adolescents appears to be normal, children with NF1 may disclose behavioral and social problems [4]. A study conducted with the Children Behavior Checklist (CBCL) [5] showed that children and adolescents with NF1 reported high scores on scales of anxiety / depression and social problems in comparison of their healthy siblings [6]. Other studies show the presence of internalizing problems in 39% of children with NF1 and externalizing in 24%. Children with NF1 have greater difficulty interacting with peers. Parents describe them as being loners, shy or awkward with peers [7].
Compared with their unaffected siblings, children with NF1 showed higher scores on the total problems, internalization and other domains (social problems, thought problems, and somatic complaints) [8]. It has been hypothesized that the presence of high scores in the scale of externalizing is related to attention problems [9]. The personality profile of children and adolescents with NF1 differs markedly from the control group. Compared to the latter, youngsters with NF1 are perceived by their parents as equally agreeable, but less conscientious in task situations, less emotionally stable, less open to new ideas, less physically active, and more extravert, more irritable, and over-reacting to frustrations, and more dependent on others [10].
No relation was detected between individual differences in the personality profiles of patients with NF1 and the severity of medical problems, the presence versus absence of cosmetic disfigurement, the mode of inheritance of the syndrome (familiar versus new mutation) and the Intelligence Quotient [10]. The somatic manifestations and aesthetic disfigurement commonly associated with this syndrome may contribute to psychological and behavioral problems of children and adolescents with NF1, and may negatively affect their quality of life [7].
Moreover, children and adolescents with NF1 show higher prevalence of Deficit Attention / Hyperactivity Disorder (ADHD) than in the general population [1,11,12]. Using a questionnaire completed by the parents some authors were able to identify ADHD in 33% of patients with NF1 in children [3]. An even higher percentage of this disorder has been documented by a study in which about 23 children with NF1, almost 50% had been diagnosed as “hyperactive” or ADHD, but these subjects were selected from patients a clinic for learning difficulties [12]. One third of NF1 population of 36 children qualified for a diagnosis of ADHD by DSM IV criteria [13]. Similarly, studies reported that 49.5% of their 93 child and adolescent patients had ADHD, as did 36% of their adult patients [9]. With regard to the behavioral aspects related to ADHD data obtained from questionnaires given to parents and teachers suggest that problems with concentration [14], attention, hyperactivity [15] and impulsivity [6] are more common in children with NF1 than in comparison subjects.
We hypothesized that children with NF1 could have ADHD associated with emotional disorders, so the aim of the study was to estimate the prevalence of both disorders in children and adolescents with NF1, in order to evaluate the associations between internalizing and externalizing behavior disorders and types of ADHD.
Methods
A cross-sectional design was adopted. Sixty-eight patients were recruited consecutively from the outpatient Genetics Clinic of the Bambino Gesù Children’s Hospital in Rome, Italy. All were diagnosed with NF1 according to the criteria of the National Institute of Heaslth [2]. Exclusion criteria included central nervous system lesion or other medical conditions affecting test performance (e.g. epilepsy/seizures, brain tumors, hydrocephalus). Social class was classified in five categories from the highest (professionals and entrepreneurs) to the lowest (handworkers – housewives).
Instruments
Child Behavior Checklist (CBCL) – Achenbach [5] is a questionnaire developed to measure, in a standardized format, emotional and behavioral problems in children until 18 years was used for children and adolescents. It is completed from a parent and it includes 113 items describing a wide range of emotional and behavioral problems, to be answered on a three point scale from 0 (“not true”) to 2 (“very true” or “very often true”) over the last six months. Eight sub-scales are scored: anxious/depressed, depressed, somatic complaints, social problems, thought problems, attention problems, rule-breaking behavior, aggressive behavior, other problems Summary scores are obtained for Internalizing behaviors (sum of scores of first three subscales) and for Externalizing (sum of scores of the subscales: social problems, thought problems, attention problems, other problems).
Measures consistent with the diagnostic categories of the American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders (Affective, Anxiety, Somatic, Attention/Hyperactivity, Oppositional and Conduct problems) are derived from the scores.
Parents inattention disease scale (SDAG) and Teachers inattention disease scale (SDAI) [16] are Italian scales for teachers and parents, to detect children inattention and hyperactivity behaviors, based on DSM IV diagnostic criteria. Each scale is composed by 18 items, and their scores are summed and transformed in scores on a scale of 0 (no problem) to 3 (worst condition). The odd items amount is related to in attention, instead impulsiveness and hyperactivity are related to all squared items amount.
The patients and their parents were consecutively enrolled; they completed the questionnaires through three sessions lasting one hour each, comprising a clinical history, cognitive, neuropsychological and emotional-behavioral evaluation, ending with a final report including diagnosis and therapy.
Statistical analysis
A sample size of 60 total patients was calculated as necessary to show a significant difference (p < 0.05) of at least 10 points on a psychometric scale between two groups of patients (e.g. affected versus not affected) with a power of 0.9. Continuous data were firstly checked with Kolmogorov-Smirnov test to assess the normal distribution; they were summarized as means±sfemales and in children < 11 years, but none of the differences by sex and age was Standard Deviations (SD) and categorical data as frequencies. Inferences for comparisons were performer with t- test for continuous data and chi-square for categorical ones. Statistical Package for Social Sciences (SPSS, version 12) was used.
Results
A total of 68 patients were enrolled in the study, 42 were males, 44 were children (6-11 years of age, the 64.7%) and 24 adolescents (>11-18 years of age, the 64.7%).
Mean age of the patients were 9 years 7 months (range 5 years 8 months-16 years 7 months, ±3.1).
Mean mothers’ age was 39 years (±4.3, range 29-59) and fathers’ mean age was 43 years (±4.9, range 32-57 years). Twelve patients (18%) had at least a brother/sister affected by NF1.
The majority of the parents has a school education ≥8 years (61.8% of the mothers and 57.4% of the fathers).
Psychological adjustment and behavior
The mean of total scores was higher than normal (56.9±11.2 versus 50.0±10) especially for internalizing behaviors (56.4±10.5) in comparison of externalizing ones (54.7±10.1). The Attention problems showed the highest score (60.7±9.0) and the Conduct problems the lowest (56.4±6.4).
According to the CBCL profile-syndrome scale, about a half of them (31 patients, the 45.6%) disclosed problems of behavior (either 11 border-line, the 16.2%, or 20 with definite clinical disorder), with an higher prevalence of internalizing problems in comparisons of externalizing behaviors (26, the 38.2% versus 19, the 27.9%).

When the patients were evaluated according to the CBCL DSMoriented scale, there was no significant difference between males and females by number of patients in the clinical or border-line range, except for a marginally significant higher prevalence of Somatic Complaints in females (Table 1); similarly no significant difference was observed between children (<11 years of age) and adolescents (> 11 years, data not shown).
Attention Deficit and Hyperactivity Disease
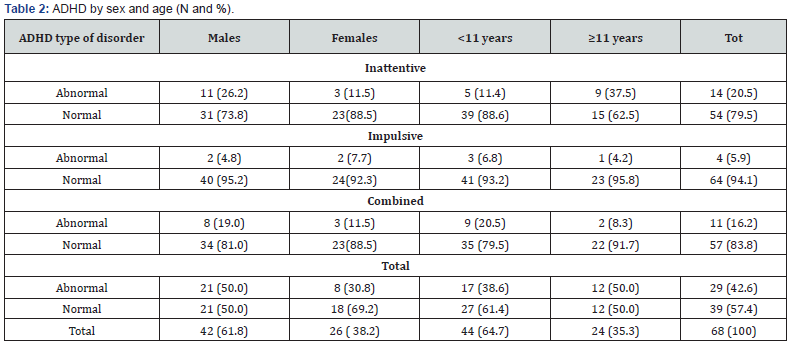
Twenty-nine children and adolescents with NF1 were affected by ADHD (42.6%) (Table 2). ADHD inattentive type showed the highest prevalence in males and >11 years of age and ADHD impulsive type the lowest, while ADHD combined seems to be more frequent in males than in significant except an higher prevalence of ADHD, inattentive type, in males vs females (26.2 vs 11.5, p = 0.02).
In children, 6-11 years, ADHD combined type is the most frequent, while among the adolescents the largest prevalence was that of the inattentive type (37.5%) (Table 2).
Attention Deficit Syndrome - Teachers version- could be obtained only for 31/68 patients, with an high prevalence of inattentive deficit (20/31, the 64.5%) and of hyperactive deficit (12/31, the 38.7%).
Relationship between ADHD and CBCL.
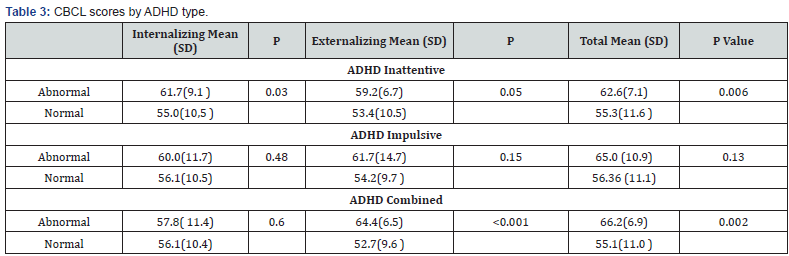
When we investigated the behavioral scores in patients with and without ADHD we found that patients with combined ADHD disclosed higher scores of behavior disorders because a striking difference of externalizing problems, as patients with inattentive type of ADHD, while in these last patients this was due mainly to internalizing problems (Table 3). A lower difference was shown in impulsive patients versus unaffected patients; in these patients externalizing scores were higher but did not attained significance, possibly for low statistical power (Table 3).
Discussion
In this study we found an high prevalence of children and adolescent with NF1 satisfying the DSM IV criteria for ADHD (42.6%) and an high prevalence of behavioral problems (45.6%). Attention deficits and behavior problems in children with NF1 have been recognized by several studies. Recent papers [3,9,13] report similar results in children and adolescents affected by NF1.
Furthermore, previous works have pointed out that attention problems are a matter of preeminent importance in children with NF1 [17,18]. Specifically, Hyman[19] and Pride [20] studies showed more difficulties in switching and sustained attention in patients with NF1, while other investigators [21] found deficit in selective attention too.
With regard to the social component, some researchers assume that deficits in perception of others emotional expressions could cause the difficulties shown by children with NF1. According to Huijbregts [22], these emotional problems could be explained by their general cognitive ability, considering processing speed, social and cognitive control information processing performances. Furthermore, conduct problems too could be explained by social information processing deficits. The general cognitive ability significantly contributes to social responsiveness, while social information processing is important for problems that individuals with NF1 have with their peers.
An high prevalence of behavioral disorders was found in our series, especially for internalizing problems and, as expected, in the subscale of attention problems. We found approximately the same results for total scores described in 46 Swiss patients [7]. In an American series all the subscales were found higher in patients with NF1, especially for Social Problems, Attention and Thought [8] while no difference of internalizing symptoms was found in 54 patients compared with peers in Texas [23]. In 17 Belgian children the highest scores of CBCL were found for Attention and Social Problems [24]. We could demonstrate that the psychological problems may arise in most patients with ADHD, except in those with impulsive type and these problems show different patterns, internalizing or externalizing, depending if ADHD is inattentive, associated with the first ones, or combined, associated with the second one, a fact not previously assessed to our knowledge.
There are some limitations of this study, such as the absence of control group of the same sex and age, or that emotional difficulties weren’t correlated with neuropsychological and cognitive aspects. Furthermore, we didn’t analyzed the relationship between the behavioral difficulties showed by our sample and aesthetic and physical problems commonly associated with this syndrome, aspects that could be useful for future investigations to better understand NF1 impact on patients’ life. Due to the crosssectional design of our study we cannot firmly define the direction of the cause-effect relationship we found between behavior and attention deficit, that is, whether internalizing or externalizing disorders adversely influence ADHD or vice versa.
Finally, our results cannot be necessarily true in other cultural environments, even assuming that no potential difference could be attributed to the language of questionnaires.
In summary, there are two important conclusions that can been drawn from this study. First, we showed an high prevalence of behavioral problems and of ADHD in our sample, suggesting that systematic screenings should be part of the clinical approach to the all the patients with NF1. Second, we found that different types of behavior disorders are associated with different types of ADHD, thus suggesting different approaches to interventions.
Acknowledgment
The research was funded by the Italian Ministry of Health. The authors have stated that they had no interests which might be perceived as posing a conflict or bias.
References
- North N (1998) Neurofibromatosis type 1 in Childhood. Cam Univ Press 4(5): 231-242.
- National Institutes of Health (1990) Neurofibromatosis 1 (Recklinghausen disease) and neurofibromatosis 2 ( bilateral acoustic neurofibromatosis). An update. Ann Intern Med 113(1): 39-52.
- Kayl AE, Moore BD (2000) Behavioral phenotype of neurofibromatosis, type 1. Ment Retard Dev Disabil Res Rev 6(2): 117-124.
- Barton B, North K (2007) The self-concept of children and adolescent with neurofibromatosis type 1. Child: care, health and develop 33(4): 401-408.
- Achenbach TM, Rescorla LA (2001) Manual for the ASEBA school-Age Forms and Profiles: University of Verm, Res Cent for Child, Youth, and Families. Burlington (VT).
- Dilts CV, Carey JC, Kircher JC, Hoffman RO, Creel D, et al. (1996) Children and adolescents with neurofibromatosis 1: a behavioral phenotype. Develop Behav Pediatr 17(4): 229-239.
- Graf A, Landolt MA, Capone Mori A, Boltshauser E (2006) Quality of life and psychological adjustment in children and adolescents with neurofibromatosis type I. J Pediatr 149(3): 348-353.
- Johnson NS, Saal HM, Lovell AM, Schorry EK (1999) Social and emotional problems in children with Neurofibromatosis type 1: evidence and proposed interventions. J Pediatr 134(6): 767-772.
- Mautner VF, Kluwe L, Thakker SD, Leark RA. (2002) Treatment of ADHD in neurofibromatosis type 1. Dev Med Child Neurol 44(3): 164-170.
- Prinzie P, Descheemaeker MJ, Vogels A, Cleymans T, Curfs, et al. (2003) Personality Profile of Children and Adolescent With Neurofibromatosis Type 1. Am Med Genetics 118(1): 1-7.
- Riccardi VM (1992) Neurofibromatosis. Phenotype, natural history and pathogenesis. (2nd edn), J Hopkins University Press, Baltimore, USA, 51(6): 658.
- Eliason MJ (1986) Neurofibromatosis:implications for learning and behavior. J Dev Behav Pediatric 7(3): 175-179.
- De Winter AE, Moore BD, Slopis JM, Jackson EF, Leeds NE (2006) Quantitative morphology of the corpus callosum in children with Neurofibromatosis and Attention-Deficit Hyperactivity Disorder. J Child Neurol 15(2): 90-96.
- Wadsby M, Lindehammar H, Eeg-olofsson O (1989) Neurofibromatosis in childhood: neuropsychological aspects . Neurofibromatosis 2(5-6): 251-260.
- Eliason MJ (1988) Neuropsychological patterns: Neurofibromatosis compared to developmental learning disorders. Neurofibromatosis 1(1): 17-25.
- Cornoldi C, Gardinale M, Masi A, Pettenò L (1996) Impulsività ed autocontrollo. Erickson, Trento, Italy, p. 327.
- Hachon C, Iannuzzi S, Chaix Y (2011) Behavioural and cognitive phenotypes in children with neurofibromatosis type 1 (NF1): the link with the neurobiological level. Brain Dev 33(1): 52-61.
- Lehtonen A, Howie E, Trump D, Huson SM (2013) Behaviour in children with neurofibromatosis type 1: cognition, executive function, attention, emotion, and social competence. In Develop Med & Child Neurol 55(2): 111-125.
- Hyman SL, Shores A, North KN (2005) The nature and frequency of cognitive deficits in children with neurofibromatosis type 1. Neurology 65(7): 1037-1044
- Pride N, Payne JM, Webster R, Shores EA, Rae C, et al. (2010) Corpus callosum morphology and its relationship to cognitive function in neurofibromatosis type 1. J Child Neurol 25(7): 834-841.
- Payne JM, Hyman SL, Shores EA, North KN (2011) Assessment of executive function and attention in children with neurofibromatosis type 1: relationships between cognitive measures and real-world behavior. Child Neuropsycol 17(4): 313-329.
- Huijbregts S C J, de Sonneville L M J (2010) Does Cognitive Impairment Explain Behavioral and Social Problems of Children with Neurofibromatosis Type 1? Behav Genet 41(3): 430-436.
- Noll RB, Reiter Purtill J, Moore BD, Schorry EK, et al. (2007) Social, emotional, and behavioral functioning of children with NF1. Am J Med Genet Part A 143A(9): 2261–2273.
- Descheemaeker MJ, Ghesquiére P, Symons H, Fryns JP, Legius E (2005) Behavioural, academic and neuropsychological profile of normally gifted Neurofibromatosis type I children. J Intellec Disabil Res 49(Pt1): 33-46.






























