Premedication for Non-Emergent Neonatal Intubation: Evolution of UK Practice, 1998-2015
Jennifer Waspe*, Lahtinen A and Prakash Thiagarajan
Department of Women's and Children's Health, Sweden
Submission: February 05, 2017; Published: March 10, 2017
*Corresponding author: Jennifer Waspe, Department Division for Women's and Children's Health, Apt 9, Fridhemsgatan 37, Stockholm 11240, Sweden, Tel: +447473984969; Email: jennifer.waspe@stud.ki.se
How to cite this article: Jennifer W, Lahtinen A , Prakash T . Premedication for Non-Emergent Neonatal Intubation: Evolution of UK Practice, 1998-2015. Acad J Ped Neonatol. 2017; 3(4): 555620 DOI: 10.19080/AJPN.2017.03.555619
Abstract
Objective: To study current practice in administering pre-intubation drugs in UK Neonatal Units for non-emergent neonatal intubations when compared to earlier UK studies on this topic.
Design: A telephonic survey of all level 2 and 3 UK neonatal units was conducted, using the same methodology as the two previous UK studies conducted in 1998 and 2007 on the same topic. Routinely intubating units, those only intubating prior to transfer to a higher level of care and the practices of level 3 units were considered separately in a subgroup analysis.
Results: The survey achieved responses from 96% of UK neonatal units. Administration of pre-intubation medications was found to be routine in 100% of units compared to 93% in 2007 and 37% in 1998. Increased proportions of units employed formal written preintubation drug guidance compared to previous studies: 14% in 1998, 76% in 2007, 86% in this study. Combined use of morphine, atropine and suxamethonium remained the most frequently used pre-intubation regimen reported by one third of all units although for the first time this regimen was rivalled by co-administration of fentanyl, atropine and suxamethonium; 33% and 30% of units reporting these regimens, respectively. Co-administration of neuromuscular blocking agents with analgesia and or sedation increased overall: from 22% in 1998, 78% in 2007 and 92% in this survey.
Conclusion: The importance of pre-intubation medication in neonates is well established and the routine use of medications prior to non- emergent intubation is now standard practice. However, there are significant variations in current practice across the UK. The authors believe that there is a need for national best practice guidance on this topic.
Introduction
Elective endotracheal intubation is frequently undertaken in neonatal units [1]. The procedure is invasive, unpleasant and predictably induces physiological stress, resulting in systemic and intracranial hypertension [2,3]. In addition there are attendant risks of bradycardia and hypoxia associated with laryngeal instrumentation and failed, prolonged or repeated attempts at correct endotracheal tube placement [3,4]. It is now widely accepted that distress caused to the neonate in order to facilitate intubation should be minimized [3,5].
A study by Whyte, Birrell and Wyllie conducted in 1998, demonstrated considerable variation between UK neonatal units (NNU) management of non-emergent endotracheal intubations [6]. A follow-up publication in 2007 by Kelleher et al. [7], showed increasing numbers of NNUs with formal written guidelines on pre-intubation medication; 14% of units in 1998 compared to 76% of units in 2007. The percentage of units using any premedication regimen had similarly risen from 37% to 93%. Our aim is to study current practice in use of premedication for endotracheal intubation of neonates in a non-emergent setting; comparing the use of written guidelines and medication regimens in UK NNUs to these two earlier studies.
Method
A list of level 2 and 3 NNUs (as defined by British Association of Perinatal Medicine, BAPM) [8] in the UK and Isle of Man was collated, on the basis that level 1 units would not be expected to care for intubated neonates [9-11]. All 7 NNUs in Northern Ireland were included, as none of them provided exclusively level 1 care.
Data collection was conducted over three, 4-week periods (November 2014, July 2015 and October/November 2015). Each unit was contacted via telephone during one of these three periods and presented with a questionnaire regarding their preintubation practices. All data collection was via telephone.
The same basic questionnaire was used in this survey as for a similar study conducted in Australia and New Zealand in 2012 [12], with the omission of one question regarding use of a direct imaging laryngoscope. This questionnaire allowed for similar analyses to those presented in the above mentioned UK surveys by Whyte and Kelleher, allowing for comparable results between all three series of UK data. The original questionnaire used in the UK studies was not obtained. To standardize the data collection, questions were directed to the nurse in charge of each unit, using the same approach as the two previous UK studies. Where the nurse in charge was unavailable, an alternative nurse or doctor present on the unit and familiar with the unit procedure completed the questionnaire. In every case a single interviewer explained the purpose of the data collection and sought verbal consent to proceed.
Subgroup analysis
In the 1998 and 2007 studies, data was stratified by selfreported undertaking of intubations either routinely or only prior to transfer to a tertiary unit (termed 'routine' and 'transfer' respectively). A further subgroup in the 2007 paper separately analysed level 3 units. For continuity, these subgroup analyses have been repeated.
Results
Of a total of 153 units contacted, two were excluded from the survey as they had merged with larger units since the registries were compiled. Six units declined to participate, achieving a response of 96% (145/151). This is comparable to the 99% and 97% responses in 1998 and 2007 respectively.
Use of guidelines
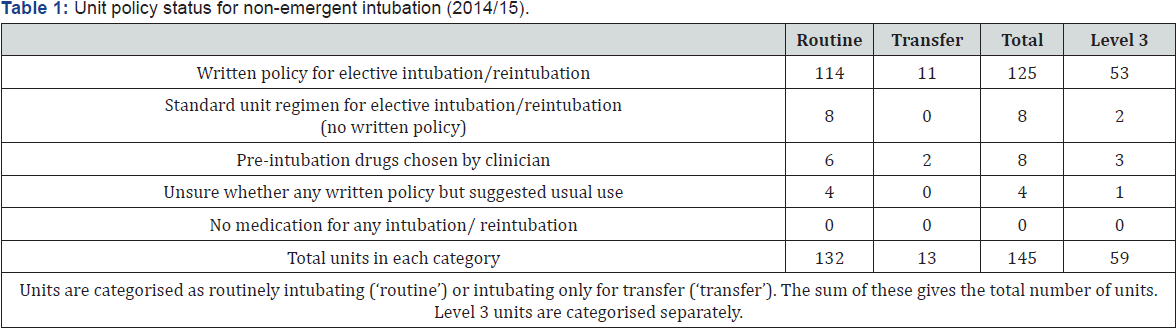
Table 1shows the format of policies for pre-intubation medication in UK NNUs. Where a unit denied having a written policy they were asked about following a standard unit policy which was in use but without supporting documentation. This category included those who were able to state a combination of pre-intubation medications they most frequently prepared. This differentiated them from units stating considerable variation such that medication use was decided by the intubating clinician. These three categories constituted 97% of units (86% referred to a written policy), with the final 3% (4/145 units) stating they were unsure about written guidance and could not be placed definitively in any of the above three categories. No unit reported intubating neonates without medication.
When asked about premedication use in emergencies outside of the delivery room, 91% (132/145) units agreed that wherever bag-mask ventilation was able to maintain an individual's oxygen saturations, usual practice was to prepare and administer preintubation drugs. Two of the 13 units in disagreement with this considered the decision to vary, depending on the intubating clinician.
Data from 132/145 units are included in the following analysis. Two units were excluded on the basis of being unable to identify a drug or combination of drugs most frequently used in their workplace, although in one case the unit did report having a written policy. A further 11 units were excluded if pre-intubation medication was chosen by the attending clinician or because the respondent was unsure about unit policy.
Co-administration of medications
In this survey, the most frequently used pre-intubation medication regimen was combined use of morphine, atropine and suxamethonium; this was reported by one third of all units (44/132 units). The combined use of fentanyl, atropine and suxamethonium however constituted another 30% (39/132 units).
The overall number of units co-administering neuromuscular blocking agents with analgesia and or sedation was 92% (126/132 units) in this survey.
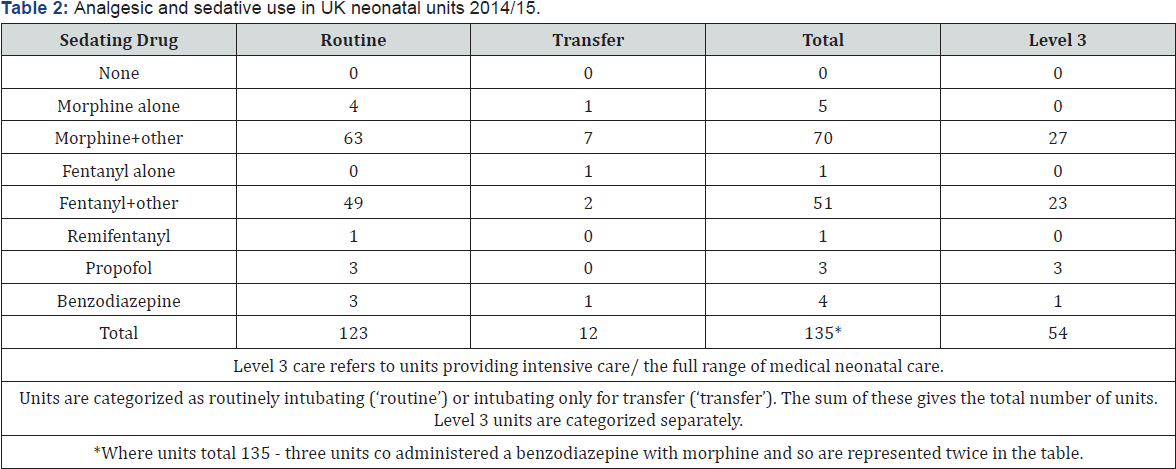
Premedication: analgesia and sedation
All 132 NNUs included an analgesic and or sedating drug in the pre-intubation regimen they most frequently used. The breakdown of drugs used is displayed in (Table 2). Morphine was used by 57% (75/132 units) with a further 39% (52/132 units) using fentanyl. Together these represent 96% of units, of which only 5% used either drug in isolation. Use of benzodiazepines was reported by 2% (4/132 units); in three instances this was coadministered with morphine and in the final case in combination with a paralysing agent.
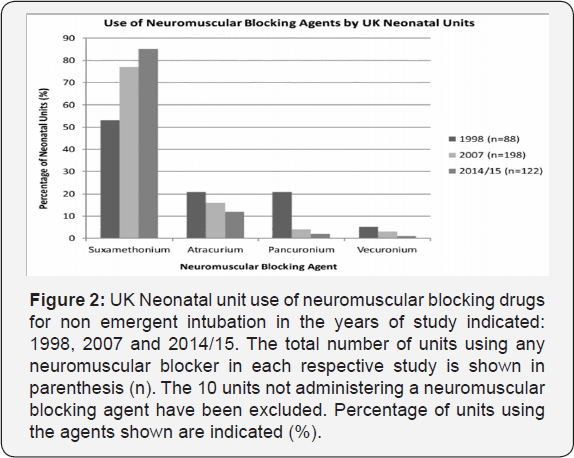
Premedication: paralysing agent (neuromuscular blocker, NMB)
As displayed in Table 3, 92% (122/132 units) included a NMB in their usual regimen. In 8S% (104/122 units) drug choice was suxamethonium, combined in all instances with fentanyl or morphine +/- atropine. Of the remaining units using a NMB, 12% (1S/122) used atracurium, 0.8% (1/122) used vecuronium and 1.6% (2/122) pancuronium. In these 18 cases not using suxamethonium there was greater variation in the co-administered sedative; morphine (11 units), fentanyl (3 units), remifentanyl (1 unit), midazolam (1 unit) and morphine plus midazolam (2 units). None of the units using propofol gave a NMB.
Premedication: atropine
Premedication included administration of atropine in 67% (88/132 units). In 92% (81/88 units), atropine was used in combination with suxamethonium and either morphine or fentanyl. In the remaining cases, atropine was combined with atracurium and either morphine or fentanyl and in a single case, morphine alone.
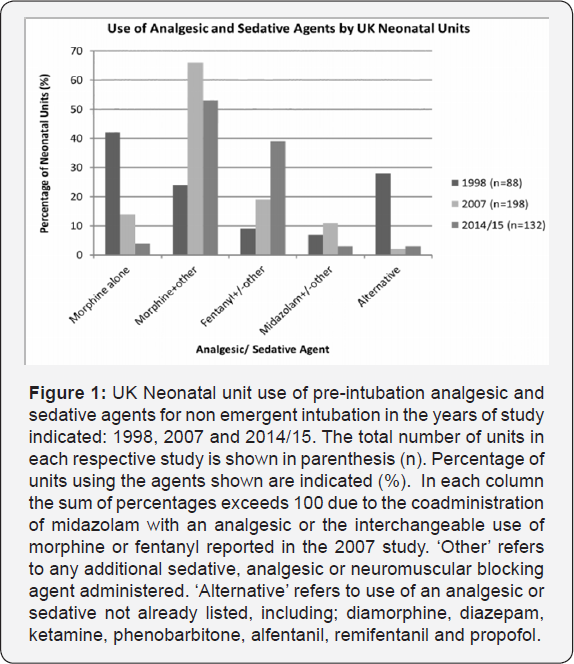
Comparison of practice: 1998, 2007 and 2014/15
In this survey of UK NNUs, 100% units administered pre-intubation drugs, compared to 37% in 1998 [6] and 93% in 2007 [7]. This illustrates that the use of premedication in a non- emergent setting is now accepted practice. Furthermore, in this survey an increased number of units reported the employment of written pre-intubation drug guidance compared to the previous UK studies: 14% in 1998, 76% in 2007 and 86% in this study.
Combined use of morphine, atropine and suxamethonium remained the most frequently used drug regimen, however for the first time in the UK, the use of fentanyl, atropine and suxamethonium almost equalled this; 33% compared to 30% of units used the morphine or fentanyl containing regimen, respectively.
The increased use of fentanyl in premedication regimens may be a reflection of both increased experience with the drug in this setting and acknowledgement of the good safety profile and considerably more rapid onset of action compared to morphine [3]. For this reason, the American Academy of Pediatrics 2010 guidance on premedication for non-emergent neonatal intubation described the use of fentanyl as preferred, compared to morphine or remifentanyl [4].
In each of the previous surveys, the use of suxamethonium as a proportion of all NMB use increased and this was again reflected in our results. In this survey, 92% (122/132 units) included a NMB in their stated regimen, compared to 78% (154/198 units) in 2007 and 22% (19/88 units) in 1998. Although neuromuscular blockade can precipitate respiratory muscle paralysis and render bag-mask ventilation challenging [13], this trend of increasing suxamethonium use is likely reflective of recognition that successful oxygenation and ventilation may only be possible following administration of a NMB. This is particularly pertinent in the face of laryngospasm or the chest wall rigidity associated with administration of fentanyl. Additionally, there is evidence that reduced numbers of both moderate and severe adverse events related to intubation are seen when NMBs are used in neonatal (and critically ill adult) populations [14].
An interesting trend demonstrated by this survey was the apparent increase in the repertoire of drug combinations used by NNUs across the UK. A minimum of 20 different regimens were encountered in this study (not including second line or agents with specific indications, such as ketamine), comparing to approximately 14 in 2007 [7] and 11 in 1998 [6] (estimations based on published data). The precise reason for this is not presently clear, however it does highlight the absence of standardized practice across the UK.
Limitations of study
One limitation of this survey was the duration over which data was collected. However, the use of a single interviewer did reduce variation in delivery of the questionnaire as well as data recording, and achieving a high response rate.
Unfortunately, data collections regarding the sequence or dose of individual drug administrations was not included in this survey nor were questions on routine use of atropine, compared to administration in response to bradycardia. This would have been interesting to examine since it has not yet been studied in the UK and variation in practice was also indicated in the 2007 UK survey.
An additional consideration may be that limiting the survey to level 2 and 3 units is now inadequate. Our results in 2015 revealed that very few of these units intubate for transfer purposes only, and it may now be appropriate to include level 1 units to be inclusive of the spectrum of regimens used in transfer circumstances.
Conclusion
The authors were pleased that all the units surveyed reported routine use of premedication in non-emergent intubation of neonates. Even though the number of units with established guidance has increased, this survey revealed that a portion of NNUs remain without formal pre-intubation drug guidelines. Given the era of protocol based medicine, this was surprising, particularly as in such settings the experience of the intubating clinician is known to be variable [12]. However, now that the question of whether premedication is used for endotracheal intubation of neonates has been addressed, establishing standard practice across a Neonatal Network or wider in the UK may be the next step in promoting familiarity and confidence in the use of such physiologically active drugs, and help further reduce adverse events related to the procedure (Figure 1 &2).
References
- Wyllie JP (2008) Neonatal endotracheal intubation. Archives of Disease in Childhood Education and Practice edition 93(2): 44-49.
- Topulos GP, Lansing RW, Banzett RB (1993) The experience of complete neuromuscular blockade in awake humans. Journal of Clinical Anesthesia 5(5): 369-374.
- Barrington KJ (2011) Premedication for endotracheal intubation in the newborn infant.Paediatr Child Health 16(3): 159-164.
- Kumar P, Denson S, Mancuso T (2010) Committee on Fetus and Newborn, Section on Anesthesiology and Pain Medicine. Premedication for Nonemergency Endotracheal Intubation in the Neonate. Pediatrics 125(3): 608-615.
- Allen K (2012) Premedication for Neonatal Intubation Which Medications Are Recommended and Why. Advances in Neonatal Care 12(2): 107-111.
- Whyte S, Birrell G, Wyllie J (2000) Premedication before intubation in UK neonatal units. Arch Dis Child Fetal Neonatal Ed 82: F38-F41.
- Kelleher J, Mallya P, Wyllie J (2009) Premedication before intubation in UK neonatal units: a decade of change? Archives of disease in Childhood Fetal and Neonatal Edition 94: F332-F335.
- British Association of Perinatal Medicine (2001) Standards for Hospitals Providing Neonatal Intensive and High Dependency Care. (2nd Edition) and Categories of Babies requiring Neonatal Care.
- Imperial College of Science, Technology and Medicine (2013) Neonatal Units 2013.
- Hallsworth M, Farrands A, Oortwijn WJ, Hatziandreu E (2007) The provision of neonatal services Data for international comparisons Technical Report. Pp. 1-187.
- The Scottish Government Maternity Services Action Group (MSAG) (2009) Neonatal Services Sub Group. Review of Neonatal Services Scotland.
- Wheeler B, Broadbent R, Reith D (2012) Premedication for neonatal intubation in Australia and New Zealand: A survey of current practice. J Paediatr Child Health 48(11): 997-1000.
- VanLooy J, Schumacher R, Bhatt-Mehta V (2008) Efficacy of a Premedication Algorithm for Nonemergent Intubation in a Neonatal Intensive Care Unit. Ann Pharmacother 42(7): 947-955.
- Foglia EE, Ades A, Napolitano N, Leffelman J, Nadkarni V, et al. (2015) Factors Associated with Adverse Events during Tracheal Intubation in the NICU. Neonatology 108(1): 23-29.






























