Use of a Nebulizer to Deliver High Frequency High Flow with a Nasal Cannula
Mitchell Goldstein*, Carter Tong, T. Allen Merritt, Elba Fayard, Michael Terry, Michael Tiras, Ricardo Peverini
Department of Pediatrics, Loma Linda University School of Medicine, USA
Submission: February 10 2017; Published: March 09, 2017
*Corresponding author: Mitchell Goldstein, Department of Pediatrics, Loma Linda University School of Medicine, USA, Email: MGoldstein@llu.edu
How to cite this article: Goldstein M, Tong C, Allen TM, Fayard E, Terry M, et al. Use of a Nebulizer to Deliver High Frequency High Flow with a Nasal Cannula. Acad J Ped Neonatol. 2017; 3(4): 555619. DOI: 10.19080/AJPN.2017.03.555619
Abstract
Introduction: The Vortan Percussive NEB™ (P-NEB) is a compact, disposable high frequency intrapulmonary percussive nebulizer for the clearance of endobronchial secretions in adults. According to the specification, "During exhalation the pneumatic capacitor and pulmonary modulator cycle to deliver high frequency (typically 11-30Hz) pressure bursts to provide an effective intrapulmonary percussion treatment”. We demonstrated the potential use for nasal cannula HFV with this device, but noted that the mean airway pressure (MAP) produced may be insufficient when required level exceeds 6cm H2O.
Hypothesis: We asked if the P-NEB produced adequate flow to use as a high frequency nasal cannula ((HF)2NC) device.
Materials and methods: Variable gas flow was connected to the P-NEB with the device outlet connected in parallel with a Fleisch pnuemotachograph connected to Validyne Flow and Pressure transducers. Flow to the P-NEB was varied from 35-50LPM while the nebulizer "bias” control was "twisted” (or adjusted) to its maximal setting. The exit port of the pnuemotachograph was occluded to simulate low compliance. Data was sampled at 1kHz using Easy Sense (Validyne) sensor and analyzed using Matlab R2012b (8.0.0.783) (The Mathworks, Inc.) and Signal Processing Toolbox 6.18. Data were analyzed using Statistica 10 (Stat Soft, Inc. (2011). STATISTICA, version 10. www.statsoft. com).
Results: As shown for the 50 LPM setting, changes in the bias flow produced significant flow perturbations, as well as, a logarithmic increase in the positive proportion of time in high flow with increased "twists”. Frequency varied from 7.5 to 47Hz.
Discussion: Although the PEEP generated was to be at low end (4-6cm H2O), there may be application of this technology for nasal ventilation. High frequency nasal ventilation has been described previously using specific pressure settings. These results demonstrate the feasibility of a nasal cannula flow based oscillation using the P-neb that provides flow based nebulizer treatments. The frequency range measured extends beyond usual oscillation ranges that may enhance the usefulness of the device. At 35LPM (below stated minimum flow), the dynamic appeared flow "starved” with an erratic rise time.
Conclusion: Although the P-NEB may not have sufficient flow to provide ventilation in all situations, its ability to generate an oscillating flow signatures may be useful in neonatal ((HF)2NC).
Introduction
The Vortan Percussive NEB™ (P-NEB) is a compact single patient, multiple use and disposable high frequency percussive nebulizer intended for the clearance of endobronchial secretions in adult patients. According to the manufacturer's specification, "During exhalation the pneumatic capacitor and pulmonary modulator cycle to deliver high frequency (typically 11-30Hz) pressure bursts to provide an effective intrapulmonary percussion treatment.” According to the product user guide, "the high frequency pressure bursts are identical to those delivered by a high frequency ventilator.” There no studies to support whether this device could be used to provide high frequency ventilation for infants. We demonstrated the potential for HFV using this device previously [1], but noted that the PEEP levels produced may be insufficient to support its use in situations greater PEEP greater than 6cm H2O. We hypothesized that P-NEB produced adequate flow to use as a high frequency nasal cannula ((HF)2NC) for infants.
Methods
Wall gas flow was connected to the P-NEB according to manfacturer's specification. The P-NEB mouthpiece (outlet) was connected via an adapter in parallel with a Fleisch pnuemotachograph connected to a Validyne Flow and Pressure transducers. Flow to the P-NEB was varied from 35LPM to 50LPM while the nebulizer pressure “bias” control was systematically adjusted from minimal to maximal pressures. The exit port of the pneumotachograph was occluded to simulate a low compliance lung model in exhalation. Data were sampled at 1kHz using Easy Sense for the IBM PC (Validyne). Pressure and Flow scalers were analyzed with Matlab R2012b (8.0.0.783) (The Mathworks, Inc.) using the Signal Processing Toolbox 6.18. Data were analyzed and plotted using Statistica 10 (Stat Soft, Inc. (2011). STATISTICA (data analysis software system), version 10. www.statsoft.com). As the study did not involve human or animal subjects, approval by the hospital internal review board was neither sought nor indicated.
Results
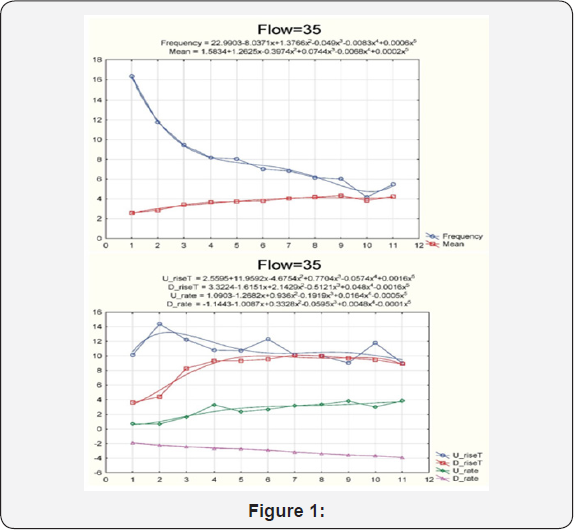
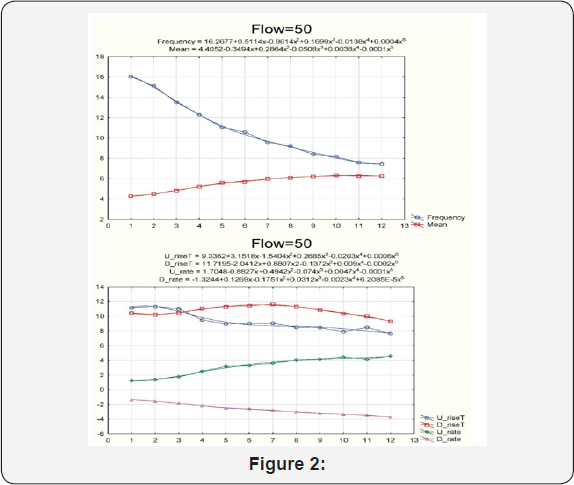
As illustrated in Figure 1 for the 50LPM setting, successive changes in the bias flow (“twists”) produced log based pressure gradient increases in peak pressure ventilation. As illustrated for the 50LPM setting, changes in the bias flow produced significant flow perturbations, as well as, a logarithmic increase in positive duty (proportion of time in high flow) with increased “twists” Frequency varied from 7.5 to 47Hz. Increased twists produced a concomitant exponential fall in frequency with an increase in mean airway pressure. Up rise time (U_rise T) and down rise time (D_rise T) were characteristically different between flows. The rate of rise of the waveform (U_rate) and the rate of fall of the waveform (D_rate) were similar across the two flows studied (see graphics).
Discussion
Although the measured range of mean airway pressure delivered is below where most high frequency ventilation occurs (Figure 2), there may be application of this technology to nasal ventilation especially during transport given the small size of the device. At 35LPM (below stated minimum flow), the dynamic appeared flow “starved” (needs to be better explained). At the higher flow rates (50LPM), there may be insufficient flow entrainment for larger pediatric or adult patients. Further, the higher than “usual” requisite flow rates may limit the usefulness of this technology during transport. A dampening effect is evident at the higher settings with respect to the peak pressures.
This may be related to an internal “dumping” mechanism within the device to prevent excessive pressure delivery; although a more physiologic test lung compliance or just a higher lung may change the propagation at the higher end of the curve. The frequency range measured extends below the manufacturer specification, which may in fact enhance the usefulness of the device. Although similar changes were noted with pressure and flow at entrainment of 35LPM (below stated minimum flow), there were situations where a number of settings appeared flow attenuated. Even at the higher end (50LPM), there may be insufficient flow entrainment for larger pediatric or adult patients. Although the mobilization component of the P-Neb was not studied in this model, there may be alterations in parameters based on the simultaneous entrainment of water vapor. This can result in deeper or more thorough gas mixing and rapid CO2 clearance.
Turbulence from these entrained instantaneous high flow rates and pulsations may be responsible for augmented diffusion. Deep airway pulsation as well as an asynchronous filling of lung units may establish what is commonly known as the “Pendelluft” effect with rapid emptying and equilibration of CO2 across these areas of the lung where closely associated alveolar unit have unequal time constants. Direct bulk flow, Taylor dispersion, Pendelluft, asymmetric velocity profiles, cardiogenic mixing, and molecular diffusion have been suggested as mechanisms which may be responsible for rapid CO2 removal on high frequency ventilation [2] and may be applicable in this model. Optimal (HF)2NC produced by the P-NEB may produce these same effects especially if optimal magnitude and amplitude matching is used, resulting in improved lung volume recruitment, improved oxygenation, and lower pCO2 observed when supplemented by the infant's own spontaneous respiratory drive.
Pillow et al. [3] has termed these frequencies as "noise.” Measurements of terminal airway resistance [4] in collapsed canine lungs during slow volume recruitment of terminal airways have been found to be governed by power-law distribution arising from vibratory changes associated with threshold phenomena propagating down a branching structure such as the airways [5]. Application of variable respiratory rates and tidal volumes in porcine oleic acid model of lung injury has demonstrated improved oxygenation and compliance [6].
Fetal lambs (gestational age) ventilated using a high frequency CPAP device had higher pH, paO2, reduced alveolar protein, decreased paCO2, and improved ventilation homogeneity [7]. The P-NEB provides a vibratory component to the pressure waveforms superimposed on the desired mean CPAP setting set by the user that varies depending on gas flow, "twists setting” and compliance of the respiratory system. These vibratory pressure fluctuations, when superimposed on the infant's spontaneous respiratory rate may promote airway opening and lung volume recruitment resulting in improved gas exchange.
In fact, there are discrete frequencies and mean airway pressures that appear to be associated with increased "twists”. This may improve gas exchange over continuous flow CPAP and produce a clinically significant reduction in paCO2 in infants with Respiratory Distress Syndrome. Similar to High Frequency Ventilation, application of a vibratory CPAP may be protective. The (HF)2NC produced by the P-NEB in the presence of non- homogenous lung expansion may recruit alveoli without marked pressure waveforms generation thereby protecting the lungs.
Conclusion
We conclude that the P-Neb produces a clinically meaningful vibration that may reduce CPAP failure. Ongoing clinical studies continue to define the benefits of vibration in terms of reductions in paCO2 and improvement in paO2 when used as an alternative to continuous flow CPAP. Adaption of the "P-NEB may have value in providing high frequency ventilation in selected clinical applications, although it may not be powerful enough in all circumstances. Clinical trials are need to establish the ability to generate an oscillating flow signature may be useful in neonatal (HF)2NC.
References
- Holst JJ, Gribble F, Horowitz M, Rayner CK (2016) Roles of the Gut in Glucose Homeostasis. Diabetes Care 39(6): 884-892.
- Bagger JI, Knop FK, Lund A, Vestergaard H, Holst JJ, et al. (2011) Impaired regulation of the incretin effect in patients with type 2 diabetes. J Clin Endocrinol Metab 96(3): 737-745.
- Jacobsen SH, Bojsen-Moller KN, Dirksen C, Jorgenson NB, Clousen TR, et al. (2013) Effects of gastric bypass surgery on glucose absorption and metabolism during a mixed meal in glucose-tolerant individuals. Diabetologia 56(10): 2250-2254.
- Holst JJ, Knop FK, Vilsboll T, Krarup T, Madsbad S (2011) Loss of incretin effect is a specific, important, and early characteristic of type 2 diabetes. Diabetes Care 34(Suppl 2): S251-S257.
- ncretin effects of increasing glucose loads in man calculated from venous insulin and C-peptide responses. J Clin Endocrinol Metab 63(2): 492-498.
- Craig CM, Liu LF, Deacon CF, Holst JJ, McLaughlin TL (2016) Critical role for GLP-1 in symptomatic post-bariatric hypoglycaemia. Diabetologia 60(3): 531-540.
- Toft-Nielsen MB, Damholt MB, Madsbad S, Hilsted LM, Michelsen BK, et al. Determinants of the impaired secretion of glucagon-like peptide-1 (GLP-1) in type 2 diabetic patients. J Clin Endocrinol Metab 86(8): 3717-3723.
- Matikainen N, Bogl LH, Hakkarainen A, Lundbom J, Lundbom N, et al. (2014) GLP-1 responses are heritable and blunted in acquired obesity with high liver fat and insulin resistance. Diabetes Care 37(1): 242-251.
- Faerch K, Torekov SS, Vistisen D, Jhonsen NB, Witte DR, et al. (2015) GLP-1 Response to Oral Glucose Is Reduced in Prediabetes, Screen- Detected Type 2 Diabetes, and Obesity and Influenced by Sex: The ADDITION-PRO Study. Diabetes 64(7): 2513-2525.
- Eriksen M, Jensen DH, Tribler S, Holst JJ, Madsbad S, et al. (2015) Reduction of insulinotropic properties of GLP-1 and GIP after glucocorticoid-induced insulin resistance. Diabetologia 58(9): 920928.
- Hojberg PV, Zander M, Vilsboll T, Knop k, karup T, et al. (2008) Near normalisation of blood glucose improves the potentiating effect of GLP- 1 on glucose-induced insulin secretion in patients with type 2 diabetes. Diabetologia 51(4): 632-640.
- Vilsboll T, Krarup T, Madsbad S, Holst JJ (2002) Defective amplification of the late phase insulin response to glucose by GIP in obese Type II diabetic patients. Diabetologia 45(8): 1111-1119.
- Holst JJ (2007) The Physiology of Glucagon-like Peptide 1. Physiol Rev 87(4): 1409-1439.
- Holst JJ, Deacon CF (2013) Is there a place for incretin therapies in obesity and prediabetes? Trends Endocrinol Metab 24(3): 145-152.
- Kazda CM, Ding Y, Kelly RP, Garyan P, Shi C, et al. (2016) Evaluation of Efficacy and Safety of the Glucagon Receptor Antagonist LY2409021 in Patients With Type 2 Diabetes: 12- and 24-Week Phase 2 Studies. Diabetes Care 39(7): 1241-1249.
- Lund A, Vilsboll T, Bagger JI, Holst JJ, Knop FK (2011) The separate and combined impact of the intestinal hormones, GIP, GLP-1 and GLP-2, on glucagon secretion in type 2 diabetes. Am J Physiol Endocrinol Metab 300(6): E1038-1046.
- Chia CW, Carlson OD, Kim W, Shin Yk, Charles CP, et al. (2009) Exogenous glucose-dependent insulinotropic polypeptide worsens post prandial hyperglycemia in type 2 diabetes. Diabetes 58(6): 1342-1349.
- Lund A, Bagger JI, Wewer Albrechtsen NJ, Christensen M, Grondahl M, et al. (2016) Evidence of Extrapancreatic Glucagon Secretion in Man. Diabetes 65(3): 585-597.
- Holst JJ, Pedersen J, Wewer Albrechtsen NJ, Knop FK (2017) Glucagon and amino acids are linked in a mutual feed-back cycle: the liver-alpha cell axis. Diabetes 66(2): 235-240.
- Junker AE, Gluud L, Holst JJ, Knop FK, Vilsboll T (2016) Diabetic and nondiabetic patients with nonalcoholic fatty liver disease have an impaired incretin effect and fasting hyperglucagonaemia. J Intern Med 279(5): 485-493.
- Bagger JI, Knop FK, Holst JJ, Vilsboll T (2011) Glucagon receptor antagonism for the treatment of type 2 diabetes. Diabetes Obes Metab 13(11): 965-971.
- Edwards CM, Todd JF, Mahmoudi M, Wang Z, Wang RM, et al. (1999) Glucagon-like peptide 1 has a physiological role in the control of postprandial glucose in humans: studies with the antagonist exendin 9- 39. Diabetes 48(1): 86-93.






























