Cup or Bottle Use and Their Effect on Exclusive Breast Feeding Rates in Preterm Infants: A Randomized Clinical Trial
Adriana Duarte Rocha*, Sabrina Lopes Lucena, Anniele Medeiros Costa and Maria Elisabeth Lopes Moreira
Instituto Fernandes Figueira/FIOCRUZ, Brazil
Submission: JANUARY 20, 2017; 2016; Published: February 20, 2017
*Corresponding author: Adriana Duarte Rocha, Av. Marechal Henrique Lott, 50 / 1911, Barra da Tijuca, Rio de Janeiro, Brazil, Tel: 552125541733; Email: chirol@iff.fiocruz.br
How to cite this article: Sabrina L L, Anniele M C, Maria E L M. TCup or Bottle Use and Their Effect on Exclusive Breast Feeding Rates in Preterm Infants: A Randomized Clinical Trial. rial. Acad J Ped Neonatol. 2017; 3(2): 555607. DOI:10.19080/AJPN.2017.03.555607
Abstract
Background: Researches has been conducted to evaluate effects of the use of cup on breastfeeding rates in term infants. Little empirical data exists regarding its relevance for preterm infants and moreover the studies present conflicting evidence
Objective: to compare the effects of cup and bottle on breastfeeding rates in preterm infants very low birth weight.
Method: The study was approved by Review Board Ethics Committee and was registered in www.clinicaltrials.gov NCT00703950. A blind, randomized, clinical trial was performed in 81 preterm infants, birth weight ≤1500 g and 26 to 32 GA. The preterm infants were allocated to the group using cup or bottle at supplementary feeding. We followed the preterm infants until 6 months age corrected.
Results: We did not observe significant differences in breastfeeding rates at discharge when the preterm infants used cup or bottle feeding (p=0.75) Likewise, we did not observed differences at one, at three and at six months after discharge (p = 0.62; 1.00 and 0.73 respectively).
Conclusion: There were no significant differences in the prevalence of exclusively breastfeeding in both groups at discharge, at one, at three and at six months age corrected.
Keywords: Breastfeeding; Bottle feeding; Feeding methods; Clinical trial
Introduction
Cups have been recommended instead of bottles when it is necessary to supplement the feeding once they would avoid “nipple confusion” [1-3]. However, clinical practice has shown that some preterm infants have difficulty to breastfeed after cup use. This is probably due to the fact that in this method the infant does not suck, just sips the milk (or swallows it).
Researches have been conducted to evaluate effects of the use of cup on breastfeeding rates in term infants. Little empirical data exists regarding its relevance for preterm infants and moreover the studies present conflicting evidence [3-11].
Then it is relevant to investigate if the cup use really facilitates the breastfeeding rate at discharge and subsequent months. The aim of this study is to compare the effects of cup and bottle feeding on breastfeeding rates in preterm infants very low birth weight at discharge and when they are one, three and six months age corrected.
Materials and Methods
The study was approved by the Fernandes Figueiras Institutional Review Board/Research Ethics Committee and by the neonatal unit where the research was conducted, and registered on www.clinicaltrials.gov NCT00703950. Informed consent was obtained from the parents/guardians of the preterm infants prior to their participation in the study.
A randomized clinical trial was performed. A total of 81 preterm infants were admitted to the study (31 boys and 50 girls) from the neonatal intensive care unit at Fernandes Figueiras Institute, FIOCRUZ, Rio de Janeiro, Brazil, which is a referral hospital in preterm delivery. These preterm infants met the following inclusion criteria: birth weight ≤1500 g, gestational age from 26 to 32 complete weeks. The gestational age was determined by date of last menstruation or first trimester ultrasound or by the New Ballard Scale. They did not present congenital anomalies, severe asphyxia (as defined by 5-min Agar score <5 or convulsions in the first 24h) and broncho pulmonary dysplasia. Infants with sepsis and intra ventricular hemorrhage grade III or IV documented by ultrasound were excluded.
All the preterm infants were stimulated by the program proposed by Fucile, Gisel & Lau [12]. The procedures were performed for 15 min per day until the preterm infants began oral feeding. The change from gavage to oral feeding started when the preterm infants reached a gestational age of at least 32 weeks, became clinically stable and performed the sucking evaluation using the technique described in previous study [13].
After first evaluation, the preterm infants were allocated to cup or bottle group at supplementary feeding. Randomization was stratified based on gestational age ranges (26-28, 28.1-30, 30.132.6) and done in 4 blocks. The allocation sequence was generated by Excel program. The method used to implement the random allocation sequence was numbered containers. Considering a difference in 20% in the percentage of preterm infants in full breastfeeding, fixing the level of confidence of 95% and statistical power of 80% the sample size calculated was 56 preterm infants.
According to hospital guideline, the preterm infants remained with orogastric tube until being able to breastfeeding. At this moment, the mothers are requested to come back to hospital in special accommodation for them, so they could breastfeed all the time.
The preterm infants allocated to cup feeding group were breastfed and received supplementation using cup, according to the technique described by Lang, Lawrence & L'E Ormer [14] and previously standardized. During the days, the feeding was performed by two speech therapists or the babies’ mothers who were trained. At night and on the weekend’s staff members or babies mothers performed the feeding. The preterm infants allocated to cup feeding group were breastfeed and received supplementation using Medela  cup.
cup.

The preterm infants allocated to bottle feeding group were breastfed and received supplementation using bottle with orthodontic nipple. The nipple used was NUK® for milk as it limits the milk flow during sucking and it is cheaper. The study protocol can be seen in (Figure 1).
In both methods, the preterm infants were continuously monitored before, during and after feeding using a cardio respiratory monitor and pulse oximeter and the feeding was interrupted when the saturation level was less than 85% or there was a change in heart rate (bradycardia or tachycardia).
The researchers did not influence on the kind of supplement used in both methods. The progression of oral feeding occurred according to the written routine of the unit based on acceptance of 20 ml/kg/day and was the same for the two groups. The infants weight was measured daily by nurses using a Filizola™ scale sensitive to 5 g according to the routine of the hospital.
The numbers of days before starting oral feeding and the numbers of days before reaching full oral feeding were counted from day of birth. According to the routine of the hospital, full oral feeding starts when the preterm infant ingests at least 2/3 of the oral feeding.
Period of hospitalization was counted from day of birth until the preterm infants were capable to suck all the feeding, without saturation level less than 85%, not needing 02 supplemental and without apnea for 7 days.
The researchers noted the number of time that the preterm infants were breastfed and number of times they received supplemental feeding using bottle or cup. Furthermore, it was noted if the mothers pumped the milk in the hospital, if skin- by-skin contact was done, the types of mothers’ nipples and the feeding method used at discharge.
We followed the preterm infants until 6 months age corrected and observed the feeding method used by mothers after discharge. We used the infant feeding’s definitions based on UNICEF. Statistical analysis of the data was done by used SPSS for Windows, version 13.0 (SPSS Incorporation, 1998). An Alpha 0.05 or less was considered evidence of statistical significance.
Results
Of the 278 very low birth weight infants who were screened for enrollment, 197 were not included (71 presented broncho pulmonary dysplasia; 24 presented congenital anomalies; 2 presented necrotizing enterocolitis; 85 succumbed to death; 8 were transferred to other units before the criteria for enrollment was established; 1 declined to participate; 1 presented intra ventricular hemorrhage grade III; 5 for other reasons).
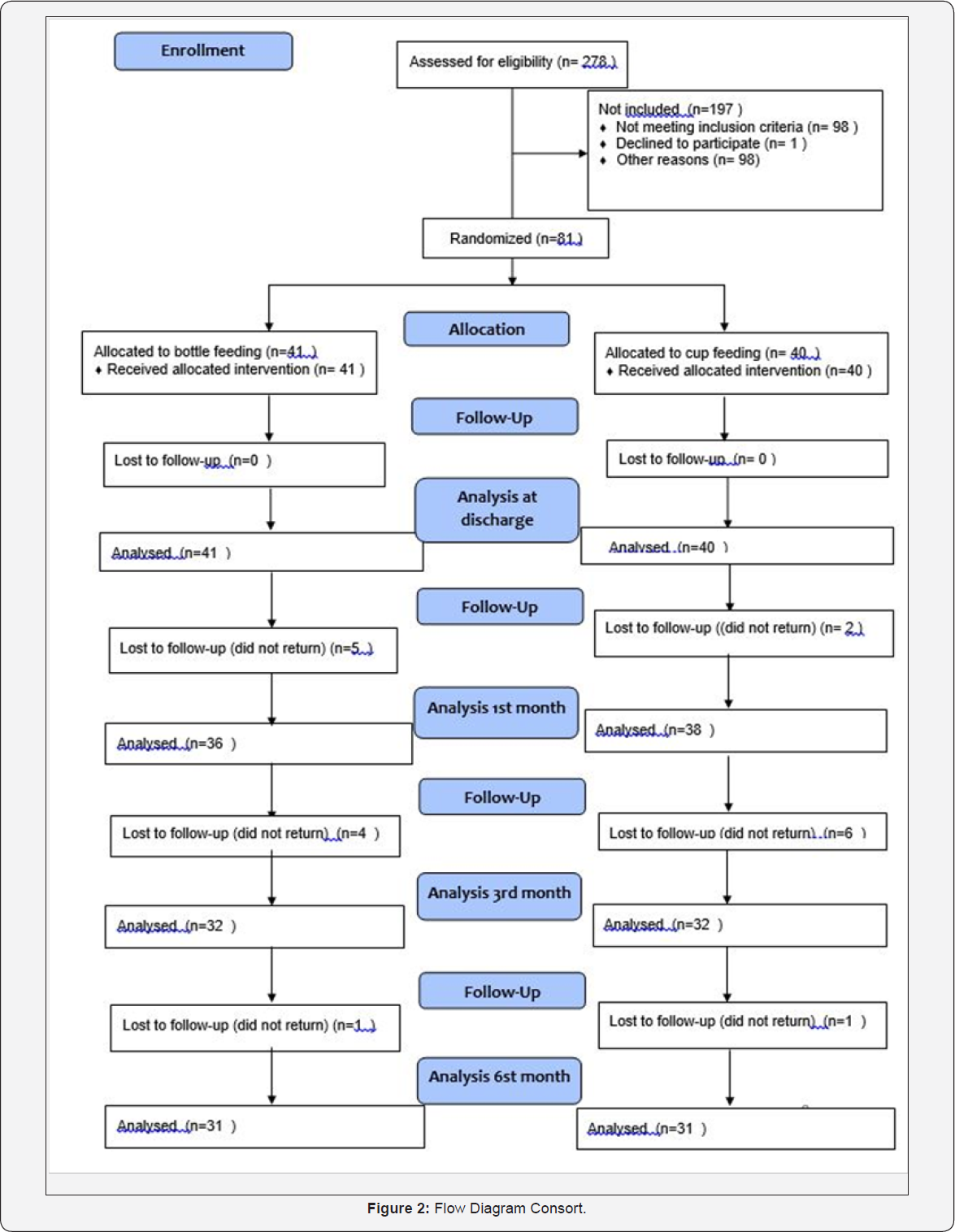
We studied a total of 81 very low birth weight infants, 41 in the bottle feeding group and 40 in the cup feeding group. The period of recruitment and follow up was between February 2006 and December 2012 (Figure 2). Demographic characteristics of preterm infants allocated for the cup and bottle feeding group are presented in (Table 1).
Although statistically significant differences were observed in birth weight between groups, they did not differ in weight at the time of study entry, ie, at oral feeding start (p = 0.21). The groups differed in gestational age at oral feeding start in favor of the group that used cup in supplemental feeding (p <0.05) (Table 1).

*t-test,**Fisher; *** Chi-Square
Using a multivariate model, the variable group wasn't associated with breastfeeding rates after controlling for weigh at oral feeding start and gestational age at oral feeding start. We observed that 66.7% of small for gestational age (SGA) were allocated in the cup group. Moreover, most appropriate for gestational age (62.5%) were in the bottle group. This difference in proportions between groups was statistically differences (p < 0.05), Infants had direct breastfeeding experiences during hospitalization with no statistically significant differences between the two groups (p = 0.82).The number of supplemental feeding did not differ in both groups either (p = 0.90).
There was no significant difference in number of days to full oral feeding and the length of stay in hospital between those randomized to cup feeding or to bottle feeding ( p = 0.16 and p = 0.27 respectively). The differences in gestational age at discharge remained significant in favor of the group that used cup in supplemental feeding (Table 2).
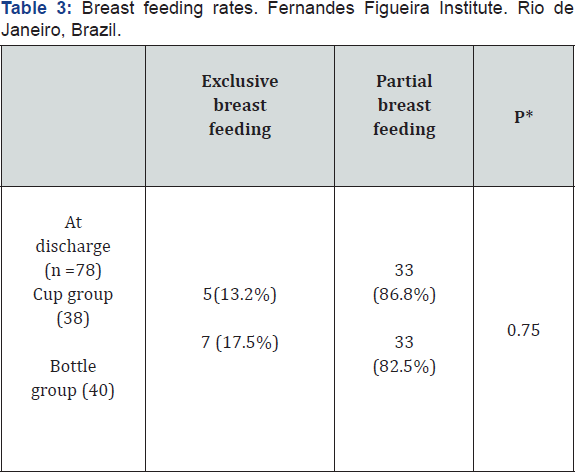
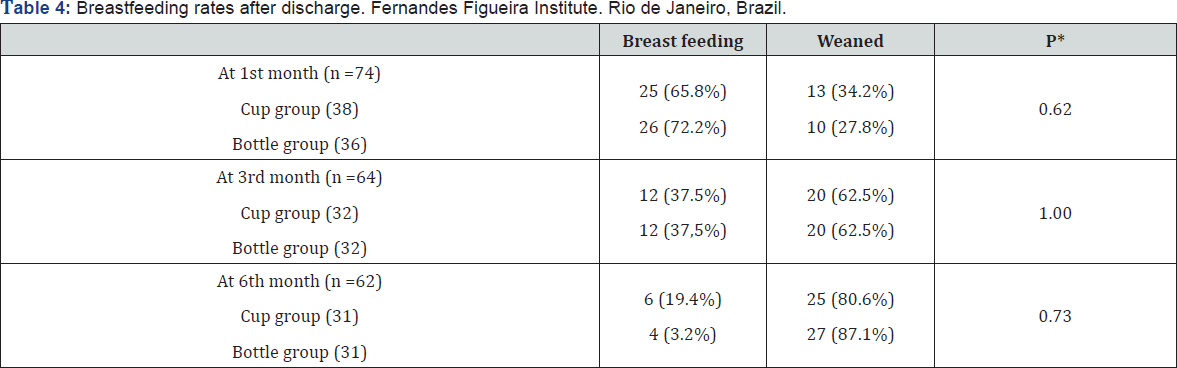
There were no significant differences in the prevalence of breastfeeding in preterm infants randomized to cup feeding compared with bottle feeding at discharge (Table 3), at one, at three and at six months after discharge (Table 4).
Using Poison Regression Model with Robust Variance controlling for factors: gestational age at birth, birth weight, gestational age and weight at oral feeding starts, maternal school education, maternal age, marital status, other children, twin pregnancy and delivery, there was no difference between the groups in breast feeding rates at discharge, with 1, 3 and 6 months.

*t-test
*Exact test-Fisher
*t-test
Discussion
Although the number of screened preterm infant was higher than estimated, the planned sample size based on available information was not attained because the attrition rate was higher. The trial had to be interrupted mainly because of a lack of on-going financial support. The main sources of attrition were the higher-than-expected prevalence of broncho pulmonary dysplasia, congenital anomalies and death.
In our study, preterm infants who were randomized to cup group started oral feeding on higher gestational age, indicating that this group might be more mature. However, this assumption was not reflected on the number of days to full oral feeding and at discharge, which was lower for bottle feeding group.
This finding was against the results observed by Gupta et al [6]. This author observed that preterm infants with lower gestational age were benefited by the use of cup use in comparison to preterm infants with higher gestational age. In literature, the difference in length of stay was 11 days [10], however in our study it was only 3 days. This difference may be a consequence of the use of different in methodologies in both studies.
There are statistically significant differences in proportions of small for gestational age (SGA) and appropriate for gestational age (AGA) between groups with the highest percentage of SGA in the cup group. Costa et al. [15] in his study found that preterm SGA infants presented normal sucking pattern later than preterms AGA. Many preterms also developed normal mature sucking pattern only after they had reached term age. However, there is no evidence in literature supporting.
We did not observe significant differences in breastfeeding rates at discharge when the preterm infants used cup or bottle feeding. Similar results were found in other studies [3,7,11]. Controversially, Collins et al. [10] observed that the use of cup increased the odds of exclusive breastfeeding at discharge in comparison to the group that used bottle. However there was no difference between the groups at 3 and 6 months. The author reports that it is difficult to recommend the use of cup due to the difficulties of acceptance by the nursing staff and parents, for example, mothers reported that they had lost milk with the use of cup.
We did not observe significant differences in breastfeeding rates at 1, 3 and 6 months after discharge. However, findings about breastfeeding rates after discharge in our study should be interpreted in the light of the following limitation: some mothers did not return to hospital, so we cannot know the real breastfeeding rates in each group.
Studies show that efficiency in sucking increases with the advance of gestational age, and higher gestational ages are predictors of higher breastfeeding rates and frequency [16-18]. In our study, the preterm infants in the cup group had higher gestational ages when they started oral feeding, what could have been reflected in higher breastfeeding rates, however it did not occur.
Moreover, Wrotniak et al. [19] showed that birth weight is positively associated with maturation in preterm infants. Therefore, in our study, higher breastfeeding rates in preterm infants in the bottle group could be explained, at least in part, for this reason. However, using a multivariate model, the variable group wasn't associated with breastfeeding rates after after controlling for weigh at oral feeding start.
In fact, these two factors alone are not able to explain breastfeeding rates. Authors have shown that maternal factors such as older age, being married, higher social class, and not smoking have a positive association with a longer duration of breastfeeding [20,21]. In this study, none of the factors discussed in several studies [20, 22-25]. As potentially favorable to negative influence on breastfeeding, such as gestational age at birth, birth weight, gestational age and weight at oral feeding starts, maternal school education, maternal age, marital status, other children, twin pregnancy and delivery, there was no difference between the groups in breastfeeding rates at discharge, with 1, 3 and 6 months.
There is no consensus in the literature about how to offer supplementary feeding to preterm infants [26,27]. More controlled studies should be conducted in order to compare the different methods of feeding transition in preterm infants so it would be possible to define which one is the most suitable. Moreover, for specifying a method, it is necessary to consider the peculiarities of preterm infants so their widespread use does not jeopardize the safety and efficacy of oral feeding.
Breastfeeding, especially in preterm infants, is a highly complex mechanism. The use of a cup or a bottle as an isolated factor was not sufficient to change the breastfeeding status of preterm infants in our unit after discharge from hospital.
Conclusion
Cup feeding cannot be recommended over bottle feeding as a supplement to breastfeeding in preterm infants due to the fact that it confers no significant benefit in maintaining breastfeeding at discharge and at 1,3 and 6 months.
References
- WHO, UNICEF (2017) Innocenti Declaration on the protection, promotion and support of breast-feeding.
- Neifert M, Lawrence R, Seacat J (1995) Nipple confusion: toward a formal definition. J Pediatr 126(6): 125-129.
- Rocha NMN, Martinez F E, Jorge SM (2002) Cup or bottle for preterm infants: effects on oxygen saturation, weight gain, and breastfeeding. J Human Lact 18(2): 132-138.
- Freer Y (1999) A comparison of breast and cup-feeding in preterm infants: effect on physiological parameters. J Neonatal Nurs 5:16-21.
- Brown SJ, Alexander J, Thomas P (1999) Feeding outcome in breast-fed term babies supplemented by cup or bottle. Midwifery 15(2): 92-96.
- Gupta A, Khanna K, Chattree S (1999) Cup feeding: an alternative to bottle feeding in a neonatal intensive care unit. J Trop Pediatr 45(2): 108-110.
- Mosley C, Whittle C, Hicks C (2000) A pilot study to assess the viability of a randomized controlled trial of methods of supplementary feeding of breastfed pre-term babies. Midwifery 17(2): 150-157.
- Marinelli KA, Burke GS, Dodd (2001) A comparison of the safety of cup feedings and bottle feedings in premature infants whose mothers intend to breastfeed. J Perinatol 21(6): 350-355.
- Howard CR, Howard FM, Lanphear B (2003) Randomized clinical trial of pacifier use and bottle feeding or cupfeeding and their effect o breastfeeding. Pediatrics 111(3): 511-518.
- Collins C T, Ryan P, Crowther C A, Mcphee A J, Paterson S (2004) Effect of bottles, cups, and dummies on breast feeding in preterm infants: a randomized controlled trial. BMJ 329: 193-198.
- Gilks J, Watkinson M (2004) Improving breast feeding in preterm babies: Cup feeding versus bottle feeding. Journal of Neonatal Nursing 10(4): 118-120.
- Fucile S, Gisel E, Lau C (2002) Oral stimulation accelerates the transition from tube to oral feeding in preterm infants. The Journal of Pediatrics 141(2): 230-236.
- Rocha AD, Lopes JM, Ramos JR (2011) Development of a technique for evaluating temporal parameters of sucking in breastfeeding preterm newborns. Early Human Development 87(8): 545-548.
- Lang S, Lawrence C, L’E Ormer R (1994) Cup feeding: an alternative method of infant feeding. Arch Dis Child 71: 365-369.
- Costa SP, Van der Schans CP, Zweens MJ, Boelema SR, Van der Meij E, et al. (2010) The Development of sucking patterns in preterm, small-for- gestational age infants. J Pediatr 157(4): 603-609.
- Mizuno K, Ueda A (2003) The maturation and coordination of sucking, swallowing, and respiration in preterm. J Pediatr 142(1): 36-40.
- Lee H C, Gould J B (2009) Factors influencing breast milk versus formula feeding at discharge for very low birth weight infants in California. J Pediatr 155(5): 657-662.
- Niela Vilen H, Melender H, Axelin A, Loyttyniemi E, Salantera S (2016) Predictors of Breastfeeding Initiation and Frequency for Preterm Infants in the NICU. J Obstet Gynecol Neonatal Nurs 45(3): 346-358.
- Wrotniak BH, Stettler N, Medoff Cooper B (2009) The relationship between birth weight and feeding maturation in preterm infants. Acta Paediatr 98(2): 286-290.?
- Zachariassen G, Faerk J, Grytter C, Esberg B, Juvonen P, et al. (2010) Factors associated with successful establishment of breastfeeding in very preterm infants. Acta Paediatr 99(7): 1000-1004.
- Pineda RG (2011) Predictors of breastfeeding and breast milk feeding among very low birth weight infants. Breastfeed Med 6(1): 15-19.
- Killersreitter B, Grimmer I, Buhrer C, Dudenhausen J W, Obladen M (2001) Early cessation of breastmilk feeding in very low birth weight infants. Early Human Development 60(3): 193-205.
- Nascimento M B R, Issler H (2005) Breastfeeding the premature infant: experience of a baby-friendly hospital in Brazil. J Hum Lact 21(1): 4752.
- Flacking R, Nyqvist K H, Ewald U, Wallin L (2003) Long term duration of breastfeeding in Swedish birth weight infants. J Hum Lact 19(2): 157-165.
- Scott J A, Landers M C G, Hughesm R M, Binns C W (2001) Psychosocial factors associated with the abandonment of breastfeeding prior to hospital discharge. J Hum Lact 17(1): 24-30.
- Zachariassen G, Faerk J, Grytter C, Esberg B, Juvonen P, et al. (2010) Factors associated with successful establishment of breastfeeding in very preterm infants. Acta Paediatr 99(7): 1000-1004.
- Lopez CP e Silva RG (2012) Métodos de alimentaçao alternativos para recém-nascidos prematuros. Rev Paul Pediatr 30(2): 278-282.






























