Cervical, Mediastinal, Intraspinal and Paraaortic Emphysema Secondary to Asthma Exacerbation Case Report
Abdussalam Khalifa Shah*, Wail Seleem, Saeed Saleh and Ashraf T Soliman
Department of Pediatrics, Hamad General Hospital, Qatar
Submission: September 24, 2016; Published: October 27, 2016
*Corresponding author: Abdussalam Khalifa Shah, Consultant General Pediatric, Department of Pediatrics, Hamad General Hospital, Qatar
How to cite this article: Abdssalam K S, Wail S, Saeed S, Ashraf T S. Cervical, Mediastinal, Intraspinal and Paraaortic Emphysema Secondary to Asthma 003 Exacerbation Case Report. Acad J Ped Neonatol. 2016; 2(1): 555578. DOI: 10.19080/AJPN.2016.02.555578
Abstract
Cervical and mediastinal emphysema associated with acute asthma exacerbation is very rare. In most cases, air leakage from ruptured alveolar escapes and dissects the hilum along peribronchovascular sheaths and spreads to mediastinum. Once in the mediastinum, air extends around the large vessel and esophagus to thoracic wall. This report presents the case of 3 years old patient with background of asthma who presented to the emergency room with palpable cervical emphysema, wheezy chest and CT evidence of cervical and mediastinal emphysema. There are only a limited number of case reports associated with cervical and mediastinal emphysema in the absence of pneumothorax in patient with asthma.. To our knowledge, this maybe the first report in pediatric where cervical, mediastinal, intraaspinal and paraaortic emphysema is induced by asthma exacerbation in the literatures.
Keywords:Asthma; Emphysema; Pediatric
Introduction
Cervical and mediastinal emphysema associated with acute asthma exacerbation is rare. This report presents 3-years old boy with recurrent asthma who presented with clinical significant cervical emphysema. Only limited number of cases have been reported with cervical and mediastinal emphysema in the absence of pneumothorax in patients with asthma.
Case Presentation
A 3 years old boy presented to our emergency department with cough, fever, shortness of breath, vomiting, muffled voice and throat pain for 2 days. He had history of recurrent chest wheezing attacks that were controlled by salbutamol nebulization. There was no history of contact with sick patients or animal pets. The child was fully vaccinated. He had manifest distress and his oxygen saturation on room air was 95%. His temperature was 38.5 °C, respiratory rate was 58per/min and heart rate=125/min. The Neck was swollen with crackling sensation due to subcutaneous emphysema. Sub costal and inter costal retraction was evident. On auscultation there was bilateral wheeze heard all over the chest. He was started on 5 L oxygen, salbutamol Nebulizer.
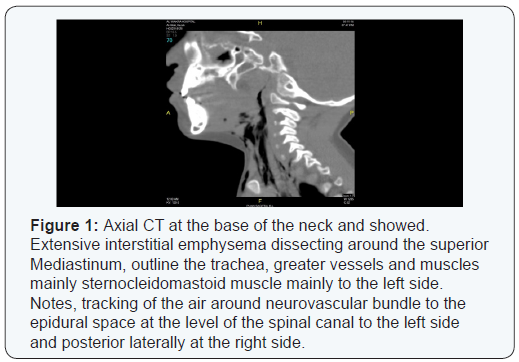
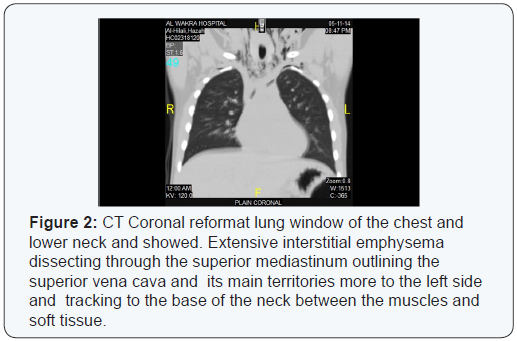
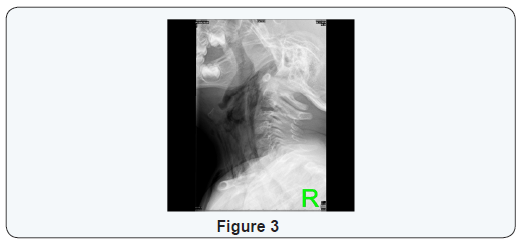
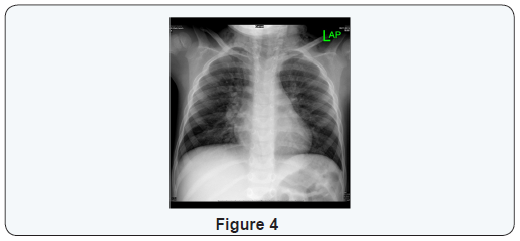
Lateral neck radiography showed increased thickness in the nasopharyngeal region and narrowing in the nasopharyngeal air column. CT scan of the neck revealed extensive air in the retropharyngeal space extending to the subcutaneous tissue of the neck, mediastinum and interaspinal canal. CT chest shows some air noted surrounding the aorta at the D 12 level. The lung parenchyma showed exaggerated broncho-vascular markings and mild septal thickening. The patient was shifted to pediatric ICU where he was started on high flow oxygen, intravenous antibiotics and continued on salbutamol nebulizer. Within 3 days of hospital admission he showed dramatic clinical and radiological improvement.
Discussion
Cervical and mid mediastinal emphysema may occur secondary to bronchial asthma, retropharyngeal abscess or lateral space abscess. Pneumo-mediastinum (PM) usually results from the over distension of the alveoli, with rupture, allowing air to enter interstitial tissues and extend into the mediastinum, neck, or intrathoracic areas. Wong et al. [1] analyzed 87 children with spontaneous pneumothorax. Forty-three patients (49.4%) had a primary idiopathic spontaneous pneumothorax (SPM). The most common cause of secondary SPM was bronchial asthma with an acute exacerbation. None of the patients <6 years (n=16) had primary PM while 60% of patients >6 years had primary PM (0% vs 60%) Therefore, a high index of suspicion for underlying causes of SPM should always be kept in mind for young children younger than 6 years [1].
Bronchial asthma predisposes to the development of SPM [2] because asthma augments airway epithelial injury and increases alveolar rupture due to lung hyperinflation [1]. Pneumomediastinum is defined as the presence of free air in the mediastinum. It can be divided into spontaneous pneumomediastinum (SPM) (without any obvious primary source) and secondary or traumatic pneumomediastinum due to a mediastinal organ injury caused by trauma, surgery or medical procedures. According to Macklin’s experimental animal model, alveolar rupture leads to air infiltration along the bronchovascular sheath with free air finally reaching the mediastinum. Furthermore, if the air travels along tissue planes it can reach the neck, face, abdomen or even the limbs, leading to subcutaneous emphysema [3].
SPM was originally described by Louis Hamman in 1939 (34), while later it was identified as Hamman’s syndrome. Sudden onset of symptoms of SPM include retrosternal pain (80%), rhinophonia and/or hoarseness (65%), dyspnea (46%), cough (26-45%), subcutaneous emphysema (32%), sore throat (18%), and neck pain (4-38%) (43). According to several reports, the most common presenting complaints are chest pain, shortness of breath and subcutaneous emphysema. The diagnosis of pneumomediastinum is based upon radiographic examination. CT chest scan is a better means of diagnosis compared to plain chest X-ray film [4].
Management of Pneumomediastinum depends upon whether or not it is complicated. Uncomplicated SPM is managed conservatively with analgesia, rest, and avoidance of maneuvers that increase pulmonary pressure (Valsalva or forced expiration, including spirometry). Therapy with high concentration oxygen has been used in an effort to enhance nitrogen washout, but is probably not necessary except in patients with severe symptoms. If such patients have underlying chronic lung or airway disease that predisposes to atelectasis, 100 percent oxygen therapy should be administered with caution, because it may lead to absorptive atelectasis [5].
Massive pneumomediastinum may be complicated by tension pneumomediastinum, which may interfere with breathing or venous return. In this case, limited mediastinotomy may be performed to drain the pneumomediastinum [5]. The outcome of SPM is usually good and this benign condition usually resolves without consequences within 2 to 15 days, often after a transient worsening of symptoms. Recurrent SPM occurs in less than 5 percent of cases, and such recurrences are typically also benign [6].
Learning Points
Although cervical and pneumomediastinum is a rare complication of asthma in pediatric age group, specially those who are less than 6 years, it should be considered always in the differential diagnosis. The clinical presentation of pneumomediastinum secondary to asthma exacerbation varies widely, so imaging study, including CT scan and X-ray are recommended to narrow the differential diagnosis. Supportive measurement is a treatment modality in most of the cases, but surgical intervention is needed in some of the cases (Figure 1 to 4).
References
- Wong KS, Wu HM, Lai SH, Chiu CY (2013) Spontenous pnuemomediastinum analysis of 87 pediatric paitents. Pediatr Emerg Care 29(9): 988-991.
- Chiu CY, Wong KS, Yao TC, Huang JL (2005) Asthmatic versus nonasthmatic spontaneous pneumomediastinum in children. Asian Pac J Allergy Immunol 23(1): 19-22.
- Macklin CC (1939) Transport of air along sheaths of pulmonic blood vessels from alveoli to mediastinum: Clinical implications. Arch Intern Med(Chic) 64(5): 913-926.
- Porpodis K (2014) Pneumothorx and asthma. J Thorac Dis 6(Suppl 1): S151-S161.
- ht t p ://www. u p toda t e . c om/co n t e n t s / s p o n t a n e o u s - pneumomediastinum-in-children-and-adolescents
- Abolnik I, Lossos IS, Breuer R (1991) Spontaneous pneumomediastinum. A report of 25 cases. Chest 100(1): 93-95.






























